Alcohol withdrawal can be physically and psychologically intense and, in some cases, life-threatening. When a person who has been drinking heavily for an extended period suddenly stops or significantly reduces alcohol use, the brain and nervous system must rapidly adapt. This sudden shift can trigger a range of withdrawal symptoms that may escalate quickly without proper medical care, particularly in individuals at risk for moderate to severe withdrawal.
Medical professionals treat alcohol withdrawal using structured detox protocols that emphasize safety, symptom stabilization, and prevention of serious complications. National treatment standards, including guidance published by the Substance Abuse and Mental Health Services Administration (SAMHSA), emphasize the importance of medically supervised detox and individualized treatment planning when managing alcohol withdrawal. In addition, recommendations from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) support the use of appropriate medications based on symptom severity, medical history, and overall health status.
This guide explains how alcohol withdrawal is treated medically, the types of medications that may be used during detox, and why professional supervision is critical for reducing health risks during the withdrawal process.
In This Guide, You’ll Learn
- Which medications are commonly used in alcohol withdrawal
- How clinicians determine treatment using symptom-severity tools
- When benzodiazepines are used and when alternatives may be appropriate
- Why medical detox protocols are essential for safety
- What typically happens after alcohol detox is complete
How Alcohol Withdrawal Is Treated Medically
Alcohol acts as a central nervous system depressant. Over time, the brain adapts by increasing excitatory activity. When alcohol is removed, the nervous system becomes overstimulated, leading to withdrawal symptoms that may include anxiety, tremors, nausea, hallucinations, seizures, and delirium tremens (DTs).
For many individuals near Morris, Bergen, and Somerset counties, safely managing alcohol withdrawal requires help from alcohol detox and rehab treatment in New Jersey that provides symptom relief and reduces health risks.
Medical detox for alcohol is designed to stabilize the nervous system, prevent complications, and keep the patient safe during this transition. Untreated alcohol withdrawal can lead to:
- Seizures
- Dangerous blood pressure changes
- Cardiac arrhythmias
- Confusion and hallucinations
- Delirium tremens, which can be fatal without treatment

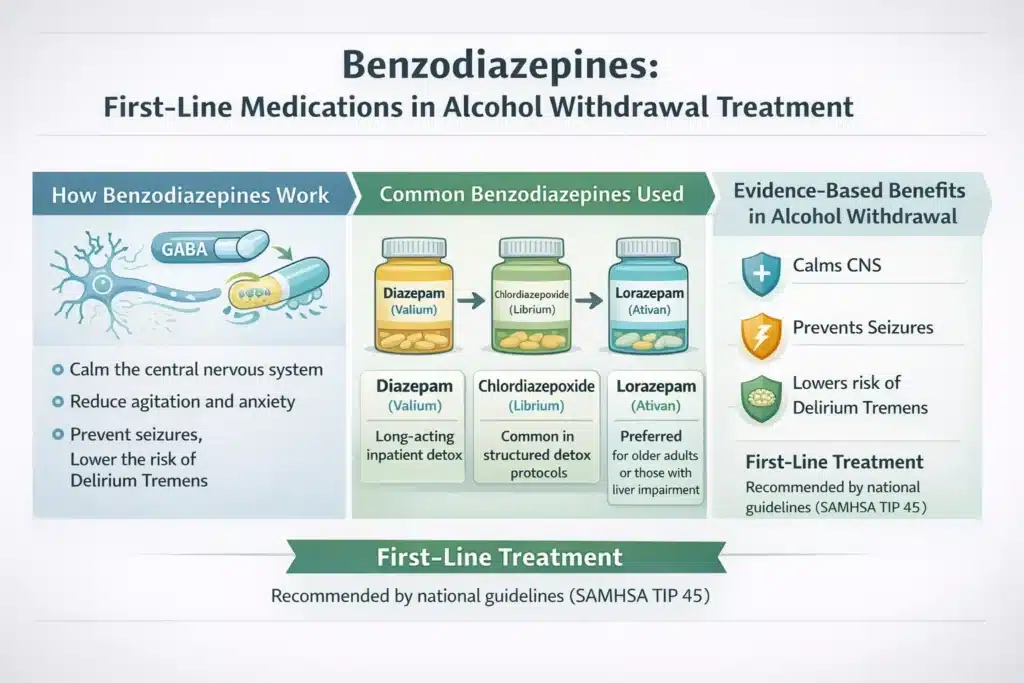
Benzodiazepines: The First-Line Treatment
Benzodiazepines are widely recognized as the first-line medications for managing moderate to severe alcohol withdrawal. Clinical guidelines and evidence-based reviews consistently support their use due to their ability to reduce withdrawal severity and prevent serious complications such as seizures and delirium tremens. Large clinical reviews examining pharmacologic management of alcohol withdrawal continue to identify benzodiazepines as the most effective treatment option for acute withdrawal stabilization (National Library of Medicine – Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond).
For a more in-depth look at how these medications are used during detox, see our article: Why Are Benzodiazepines Used for Alcohol Withdrawal?
How Benzodiazepines Work
Benzodiazepines act on the central nervous system by enhancing the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that plays a key role in calming brain activity. During alcohol withdrawal, GABA activity is reduced while excitatory signaling increases, leading to nervous system overstimulation. By restoring inhibitory balance, benzodiazepines help to:
- Calm the central nervous system
- Reduce agitation and anxiety
- Prevent withdrawal-related seizures
- Lower the risk of delirium tremens
Common Benzodiazepines Used in Alcohol Detox
- Diazepam (Valium) – A long-acting medication often used in inpatient detox settings
- Chlordiazepoxide (Librium) – Commonly used in structured detox protocols due to its longer duration of action
- Lorazepam (Ativan) – Frequently preferred for older adults or individuals with liver impairment
According to SAMHSA TIP 45, benzodiazepines remain the most effective medications for preventing severe alcohol withdrawal complications when used appropriately and under medical supervision.
“The Cochrane Collaborative found that benzodiazepines are more effective than placebo for protecting against seizures caused by alcohol withdrawal syndrome. Researchers also found that benzodiazepines may offer protection against many outcomes when compared with other medicines” (Source: Office of Disease Prevention and Health Promotion).
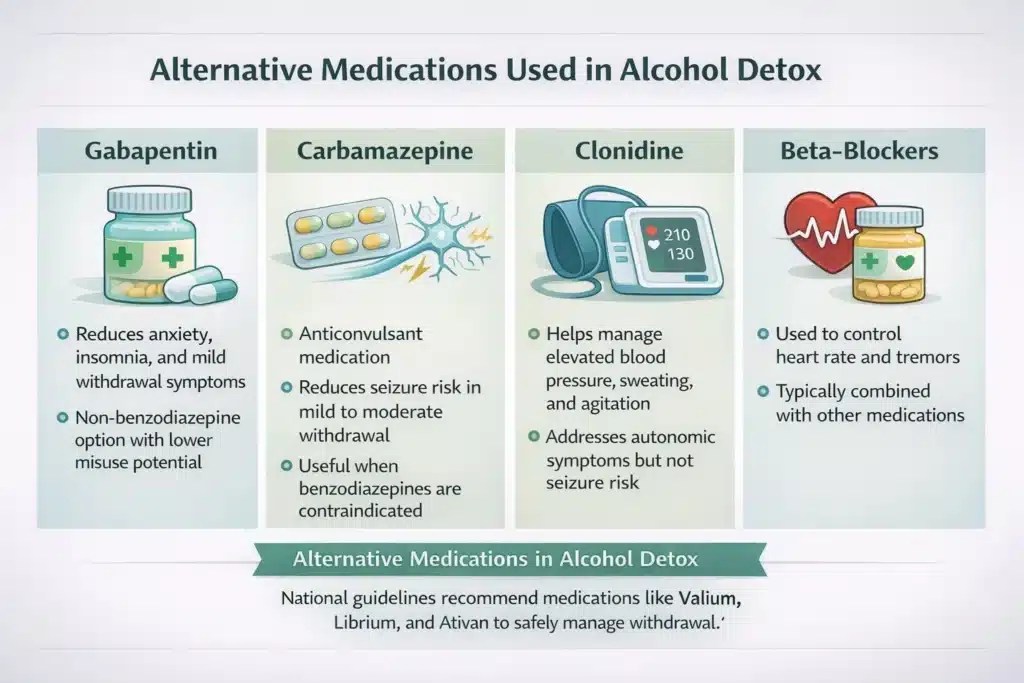
Alternative Medications Used in Alcohol Detox
Some patients may not be ideal candidates for benzodiazepines, or may experience mild to moderate withdrawal that can be managed with alternative medications. These options may also be used as adjuncts.
Gabapentin
- Used to reduce anxiety, insomnia, and mild withdrawal symptoms
- Non-benzodiazepine option with lower misuse potential
- Often used in outpatient or step-down detox settings
(gabapentin for alcohol withdrawal)
Carbamazepine
- Anticonvulsant medication
- Can reduce seizure risk in mild to moderate withdrawal
- Useful when benzodiazepines are contraindicated
Clonidine
- Helps manage elevated blood pressure, sweating, and agitation
- Addresses autonomic symptoms but not seizure risk
Beta-Blockers
- Used to control heart rate and tremors
- Typically combined with other medications
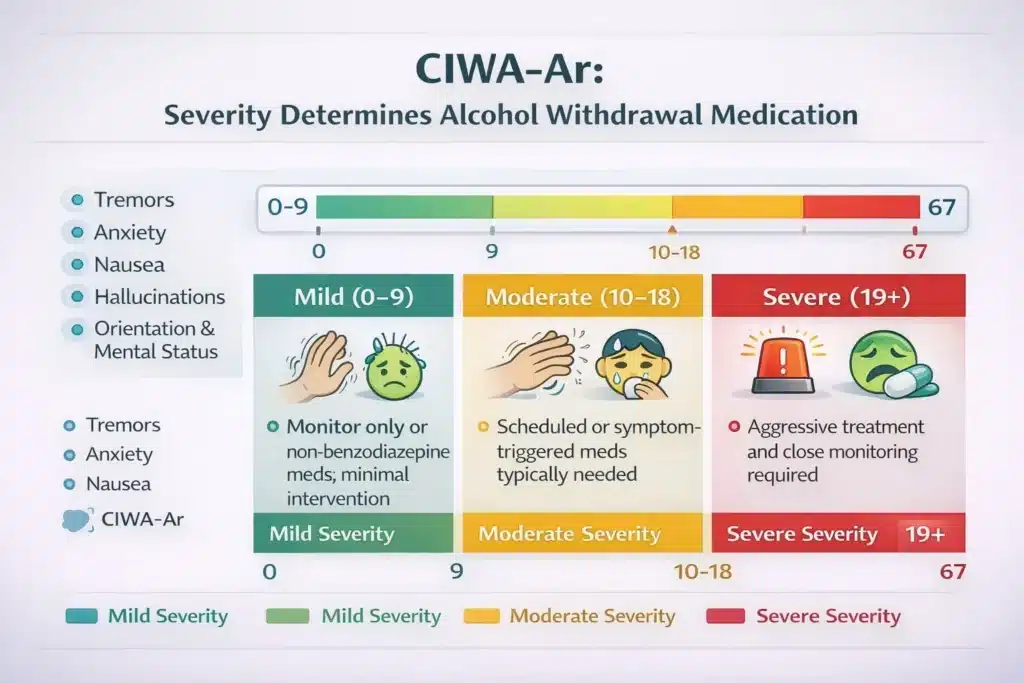
Medication Use Depends on Severity (CIWA-Ar)
Clinicians rely on the CIWA scale for alcohol withdrawal (Clinical Institute Withdrawal Assessment for Alcohol, Revised) to determine which medications are needed and at what dosage.
The CIWA-Ar assesses symptoms such as:
- Tremors
- Anxiety
- Nausea
- Hallucinations
- Orientation and mental status
CIWA-Ar Scoring and Treatment
- 0–9 (Mild): May require monitoring only or non-benzodiazepine medications
- 10–18 (Moderate): Typically treated with scheduled or symptom-triggered medication
- 19+ (Severe): Requires aggressive treatment and close medical monitoring
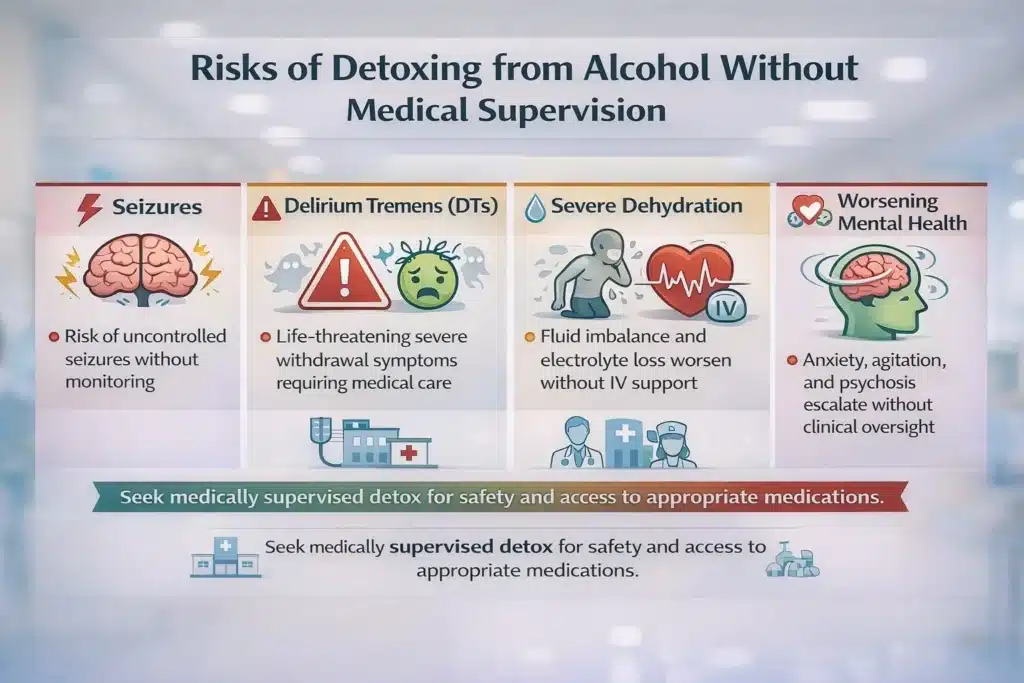
Risks of Detoxing Without Medication
“It is important to note that patients who lose access to their medications and are unable to access care may try to obtain benzodiazepines from an illicit source. With high rates of counterfeit pills containing fentanyl, these individuals are at an increased risk for overdose or death.” Source: New Jersey Department of Health
Detoxing from alcohol without medical supervision significantly increases health risks. Sudden withdrawal can overwhelm the nervous system, leading to emergencies that cannot be safely managed at home.
Risks include:
- Seizures
- Delirium tremens
- Severe dehydration
- Cardiac complications
- Worsening mental health symptoms
For these reasons, safe alcohol detox options always involve medical monitoring and access to appropriate medications.
What Happens After Detox?
Detox addresses physical dependence, but it does not treat the underlying causes of alcohol use disorder. After detox, patients typically transition into continued care, which may include:
- Residential or inpatient treatment
- Intensive outpatient programs (IOP)
- Individual and group therapy
- Relapse-prevention planning
- Ongoing medical or psychiatric care
Many patients also benefit from medication-assisted treatment (MAT) after detox to reduce cravings and support relapse prevention. Medications like naltrexone, acamprosate, or disulfiram may be recommended based on the individual’s history and goals. These are typically used alongside therapy and ongoing support.
Need Help with Alcohol Withdrawal or Treatment?
Understanding which medications are used during alcohol withdrawal is an important first step, but treatment decisions should always be made with qualified medical professionals. If you or someone you love has questions about withdrawal symptoms, medication options, or what level of care may be appropriate, our team can help you explore next steps and connect with trusted treatment resources.
Frequently Asked Questions (FAQ)
What is the Most Commonly Used Medication for Alcohol Withdrawal?
Benzodiazepines are the most frequently used medications due to their effectiveness in preventing seizures and severe symptoms.
Are There Natural Alternatives to Medication During Detox?
Supplements may support recovery, but they are not a safe substitute for medical detox.
How Long Are Medications Used During Alcohol Withdrawal?
Most detox protocols last between 3 and 7 days, depending on severity.
Is Detox from Alcohol Dangerous Without Medication?
Yes. Unmedicated detox increases the risk of life-threatening complications.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












