Considering a 60‑day rehab in New Jersey? This overview is clinical and straight to the point: who qualifies, how to verify NJ DMHAS licensing & Joint Commission/CARF status, what treatment actually includes, insurance and parity basics, measurable outcomes to ask for, and logistics for admission and aftercare. No spin, actionable steps, credible sources, clear decisions.

Key Takeaways
- 60 days fits people with high‑severity addiction, relapse after 30 days, or co‑occurring mental health needs; often aligns with ASAM 3.5–3.7 residential.
- Verify safety & quality: active NJ DMHAS license, Joint Commission or CARF, physician and psychiatry oversight, counselor credentials. No data? red flag.
- Care should include daily medical checks, MAT when needed, CBT & DBT, trauma care, family sessions, peer support; discharge planned from day one to PHP/IOP + local supports.
- Insurance and rights: prior auth and utilization review are common; NJ FamilyCare or commercial plans must follow parity. Get a written out‑of‑pocket estimate and clear appeal steps.
Eligibility, Admissions, and Licensing in New Jersey
Who a 60-Day Rehab Program Fits in NJ (Blunt Criteria)
- You already tried a 28–30 day program and relapsed or never stabilized.
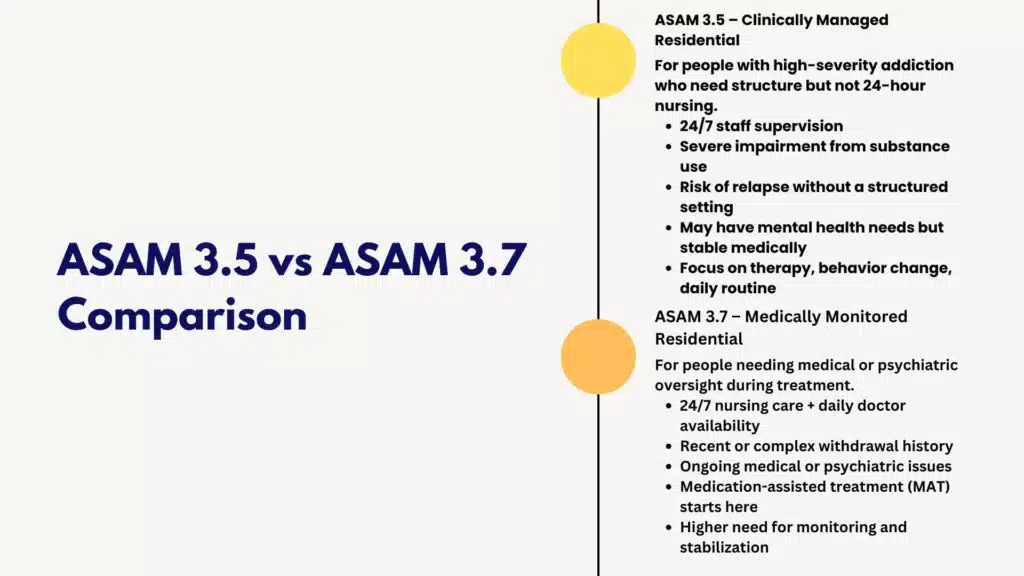
- You meet ASAM 3.5 or 3.7 level of care:
- 3.5: clinically managed residential, high-intensity services, severe functional impairment, risk of relapse without 24/7 support.
- 3.7: medically monitored residential, need for 24-hour nursing with daily physician availability (e.g., complicated withdrawal history, significant medical/psychiatric comorbidity).
- You have co-occurring disorders (depression, PTSD, bipolar, anxiety) needing integrated psychiatry with therapy and medication.
- You need time for medication-assisted treatment (MAT) induction/titration (buprenorphine, methadone continuation, naltrexone), and stabilization of psychiatric meds.
- You have polysubstance use, chronic cravings, high-risk triggers, or limited supports at home.
- You require structured family therapy to reduce relapse risk in the home system.
- You lack safe housing or recovery supports for the first 6–8 weeks of sobriety.
Rolling Hills Recovery Center is designed for people who meet the above profiles and want a longer stabilization window with evidence-based treatment and holistic options. If you’re unsure which level you meet, request an ASAM-guided screening before admission.
Licensing and Accreditation You Should Verify (New Jersey-Specific)
Because public information can be thin or outdated, prioritize verification:
- Facility license: Confirm the program is licensed by the New Jersey Division of Mental Health and Addiction Services (DMHAS). Ask for the facility license number and service categories (residential, withdrawal management level, and outpatient). Verify at the DMHAS site: New Jersey Division of Mental Health and Addiction Services.
- Accreditation: Ask if the facility is accredited by The Joint Commission or CARF. Accreditation is not mandatory, but it is a quality signal tied to standardized safety and outcome processes.
- Physician credentials: Ask for board certification (Addiction Medicine, ABPM or ABAM; Addiction Psychiatry, ABPN), and experience treating your primary substances and co-occurring disorders.
- Nursing and counseling staff: Look for NJ CADC or LCADC, LCSW, LPC, LMFT; ask staff-to-patient ratios by shift; ask if they have 24/7 nursing if they admit ASAM 3.7.
- Medication handling: Confirm DEA compliance, controlled-substance storage, and MAT protocols.
- Safety and reporting: Ask for policy on critical incident reporting, seclusion/restraint (should be rare), and infection control audits.
Useful resource:
- New Jersey Division of Mental Health and Addiction Services: https://www.nj.gov/humanservices/dmhas/
Admissions Workflow (Step-by-Step)
- Pre-admission screening
- Phone screen using ASAM dimensions (intoxication/withdrawal, biomedical, emotional/behavioral, readiness to change, relapse potential, recovery environment).
- Insurance verification (benefits, in-network status, pre-authorization steps).
- Medical and psychiatric history collection (med list, prescriber information, allergies).
- Detox handoff (if needed)
- If you require alcohol, benzodiazepine, or opioid withdrawal management, complete medically supervised detox before residential admission, or admit into a facility with ASAM 3.7-WM capabilities. If you need alcohol detox first, learn how we coordinate with an alcohol detox in New Jersey.
- Nurse-to-nurse handoff including last CIWA/COWS scores, vitals, and detox protocol completion. Ensure continuity for MAT (e.g., buprenorphine, methadone dosing, or naltrexone timing).
- Medication reconciliation
- Bring a current meds list with doses, prescriber names and numbers, and last fill dates.
- The admitting clinician will reconcile home meds with the new treatment plan. High-risk meds (benzodiazepines, stimulants) are carefully reviewed for necessity and alternatives.
- Medical clearance
- Basic labs may be required (CBC, CMP, UDS, pregnancy test if applicable). TB screening per facility policy. Infectious disease risk assessment. Bring CPAP or other medical devices as instructed.
- Financial and consent forms
- Sign releases to coordinate with past providers, family (optional), and employer if leave paperwork is needed.
- Review patient rights, grievance policy, visitation, and phone policy.
- Arrival
- On arrival day: nursing intake, safety search, orders for medications, and introduction to unit expectations and schedule.
If you need inpatient-level structure and medical oversight as described, explore our inpatient drug rehab in New Jersey post.
What a 60-Day Program Includes
Medical Oversight and MAT
- Daily or near-daily nursing assessment early on; regular vitals; withdrawal monitoring.
- Physician or advanced practice provider evaluation on admission and weekly, with additional visits as clinically needed.
- MAT when indicated:
- Opioids: buprenorphine or methadone continuation/transfer, extended-release naltrexone scheduling if appropriate.
- Alcohol: acamprosate, naltrexone, disulfiram when suitable.
- Craving/sleep/mood/safety medications managed carefully.
- Chronic condition management: hypertension, diabetes, asthma, pain, coordinated with primary care and specialists if needed.
Core Psychotherapies and Trauma-Informed Care
- Cognitive Behavioral Therapy (CBT) for triggers, thinking patterns, and skills practice.
- Dialectical Behavior Therapy (DBT) skills: distress tolerance, emotion regulation, interpersonal effectiveness.
- Trauma-informed care: pacing, grounding, and stabilization work prior to trauma processing. If formal trauma processing is indicated (e.g., CPT), timing is individualized.
- Measurement-based care: brief tools (e.g., craving scales; PHQ-9 for depression; GAD-7 for anxiety) at baseline and at discharge to track change.
Family Therapy and Education
- Structured family sessions (virtual or in-person) to map triggers, boundaries, and relapse warning signs.
- Psychoeducation on enabling vs support, communication skills, and safety planning.
- If your family will be part of care, see our page about family support during rehab.
Psychiatry, Peer Support, and Structured Days
- Weekly psychiatry or prescriber visits. More frequent early on if mood or psychosis symptoms need close titration.
- Certified peer or recovery coaching to model day-to-day recovery skills.
- Structured daily blocks:
- Morning: vitals, goals group, psychoeducation/skills.
- Midday: individual therapy or psychiatry, experiential groups.
- Afternoon: CBT/DBT groups, relapse prevention, fitness, or mindfulness.
- Evening: peer-led recovery meetings or community groups.
- Weekend programming is not empty time: family workshops, recreational therapy, relapse prevention labs, and alumni talks.
Holistic and Wellness Options
- Mindfulness, yoga, movement, and simple breath work as tolerated.
- Nutrition basics, sleep hygiene, and pain self-management strategies.
Co-Occurring Disorder Care
- Integrated treatment for depression, anxiety, PTSD, bipolar, ADHD, and others.
- Psych med management with side-effect monitoring and functional targets (sleep, focus, affect).
Example Weekly Rhythm (Sample)
- Monday: medical check-in, CBT group, individual therapy, evening peer meeting.
- Tuesday: DBT skills, family session, recreation therapy.
- Wednesday: psychiatry visit, trauma-focused group (stabilization), mindfulness.
- Thursday: relapse prevention lab, case management (housing/work), community meeting.
- Friday: skills rehearsal, med review, weekend plan.
- Saturday/Sunday: family workshop or alumni talks, structured recovery activities.
Discharge Planning and Step-Down
- Planning starts week 1. You will get:
- A written relapse prevention plan with triggers, coping steps, and people to call.
- MAT continuity plan (prescriber appointment within 7 days; pharmacy coordination).
- Step-down level of care: PHP or IOP within 72 hours of discharge if possible.
- Community supports: mutual-help (12-step, SMART Recovery, Refuge Recovery), peer support, therapy appointments near home.
- Naloxone training for you and your family; kit access before discharge.
- Rolling Aftercare: alumni groups or check-ins; verify frequency and format with your coordinator.
Costs, Insurance, and Protections
Coverage in New Jersey
- NJ FamilyCare (Medicaid): Many residential and withdrawal management services are covered for eligible members; benefits vary by plan. Review eligibility and benefits at NJ FamilyCare.
- Commercial PPO/HMO: Coverage depends on plan, network status, pre-authorization, and medical necessity determinations using ASAM criteria.
- Medicare Advantage and commercial exchange plans: check network status and prior auth rules. Original Medicare rarely covers residential SUD; partial hospitalization or IOP may be covered.
If we are out-of-network, we may pursue a single case agreement with your plan when appropriate. We will inform you of the requirements and likely timelines.
Parity Rights, Pre-Authorization, and Appeals
- Mental health parity: New Jersey enforces federal and state parity laws. Your insurer must not impose more restrictive limits on SUD than on medical/surgical care of similar complexity. See NJ Department of Banking and Insurance mental health parity resources.
- Prior authorization: Expect initial authorization and ongoing utilization review (UR) every few days. We provide clinical updates tied to ASAM dimensions.
- If denied:
- Request denial rationale in writing.
- File a same-day expedited appeal for urgent care; include a physician letter, ASAM criteria mapping, and risk factors.
- If internal appeal fails, request an external review. Document all calls (date/time/agent).
- Simple appeal template (copy and adapt):
- Subject: Expedited Appeal – Residential SUD, ASAM 3.5/3.7, [Member Name, DOB, ID]
- Medical Necessity: Diagnosis, ASAM dimension risks, failed lower levels of care, co-occurring conditions, and MAT needs.
- Safety Risks: Overdose, severe withdrawal history, psychiatric instability, unsafe home environment.
- Treatment Plan: 60-day residential with medical oversight, MAT, CBT/DBT, family therapy, step-down plan.
- Requested Action: Approve continued stay through [date] with step-down authorization pre-arranged.
Useful resources:
- NJ Department of Banking and Insurance mental health parity: https://www.nj.gov/dobi/bulletins/blt24_14.pdf
- SAMHSA treatment and recovery resources: https://www.samhsa.gov/
Out-of-Pocket (OOP) Considerations
- Potential OOP items:
- Deductible, copays, coinsurance.
- Out-of-network differential if applicable.
- Pharmacy co-pays for take-home meds.
- Travel costs.
- Ask for:
- Verification of benefits (VOB) in writing.
- A Good Faith Estimate (for self-pay/uninsured) under the No Surprises Act.
- Clear pharmacy billing plan (on-site vs local pharmacy).
- Payment options: HSA/FSA, payment plans, and employer-assistance programs, where available.
Work Leave, Confidentiality, and Forms
- FMLA: Up to 12 weeks of job-protected leave for your own serious health condition (SUD included) if eligible. See the U.S. Department of Labor FMLA page: https://www.dol.gov/agencies/whd/fmla
- New Jersey state benefits:
- Temporary Disability Insurance (TDI): May apply to your own medical condition; check eligibility and documentation requirements.
- NJ Family Leave Act (NJFLA): Applies to caring for a family member, not for your own treatment.
- HIPAA: Your treatment is confidential. Releases are required before speaking with your employer or family.
What to Bring and What Not to Bring
Bring:
- Government ID, insurance card, payment method.
- Current medication list and labeled prescriptions (no loose pills); prescriber contacts.
- Comfortable clothing, closed-toe shoes, light jacket.
- CPAP or medically necessary devices, glasses, and hearing aids.
- A list of important phone numbers (family, employer, HR, outpatient providers). Do not bring:
- Illicit substances, weapons, or paraphernalia.
- Large amounts of cash or valuables.
- Opened supplements or unapproved OTC meds.
- Vapes and combustible tobacco may have restrictions; ask in advance.
- Smart devices may be limited; confirm phone/electronics policy.
Outcomes and Quality Signals You Should Demand
What to Ask Programs For (and Expect a Straight Answer)
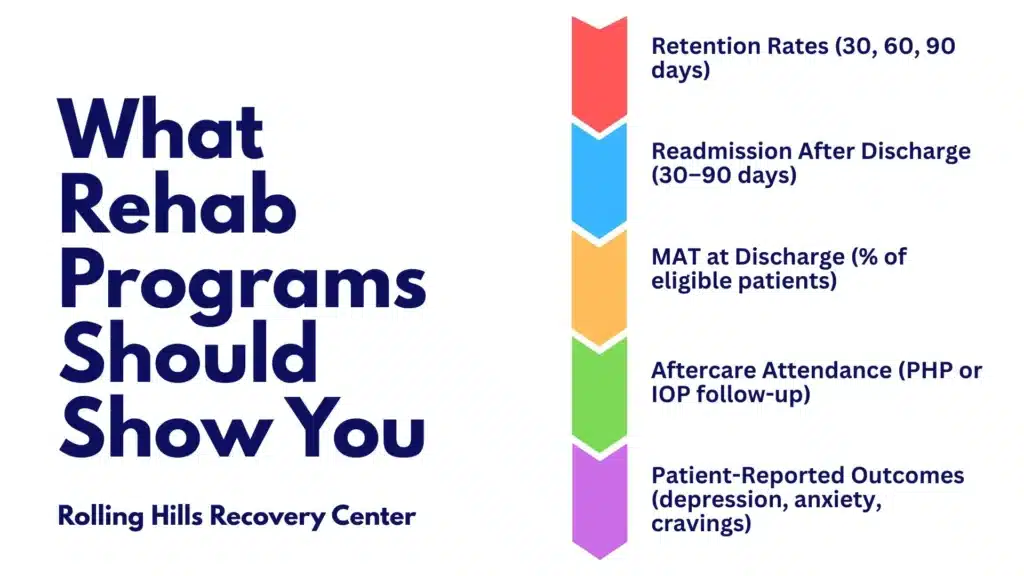
- Retention and completion:
- 30-, 60-, and 90-day retention and completion rates for your diagnosis group.
- Readmission:
- 30-day and 90-day readmission rates after discharge and reasons (overdose, relapse, housing instability).
- Overdose prevention:
- Percent discharged with naloxone and training; post-discharge overdose follow-ups.
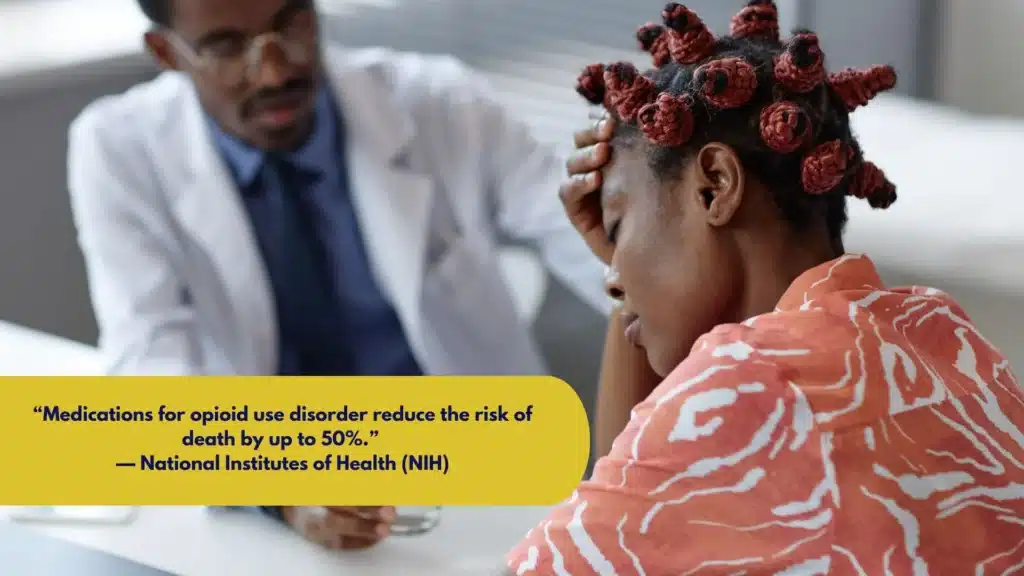
- MAT continuity:
- Percent of eligible patients on MAT at discharge, and 30-day MAT adherence.
- Patient-reported outcomes:
- Change in craving scores; depression/anxiety measures (e.g., PHQ-9, GAD-7) from admission to discharge.
- Safety and staffing:
- Staff-to-patient ratios by shift; serious safety events per 1,000 patient-days; restraint/seclusion frequency (should be near zero).
- Aftercare engagement:
- Percent attending PHP/IOP within 7 days; 30-day aftercare appointment adherence.
Programs unwilling to share de-identified, aggregate metrics are asking you to trust without data. Ask for a one-page outcomes summary.
Why 60 Days Can Improve Stabilization vs 30 Days (For High-Severity Cases)
- Medication timelines:
- MAT induction and stabilization, especially methadone titration or timing naltrexone, often require more than 3–4 weeks to settle.
- Antidepressants, mood stabilizers, or sleep interventions benefit from extra time to adjust and evaluate.
- Skills acquisition:
- CBT/DBT skills require practice, feedback, and correction cycles; 4 to 8 weeks is a practical window.
- Family systems:
- Scheduling, conducting, and integrating family therapy takes time; new boundaries need rehearsal.
- Discharge readiness:
- Coordinating housing, employment leave, and step-down access is smoother with a 60-day runway.
- Caveat:
- Not everyone needs 60 days. If you stabilize quickly, step-down may happen sooner; if risk remains high, longer stays or stepped care may be indicated.
| Program length | Best fit profile | Core advantage | Trade-off |
|---|---|---|---|
| 30 days | Lower to moderate severity, stable supports, rapid MAT response | Fast stabilization, cost/time efficient | Less time to optimize meds and family systems |
| 60 days | Moderate to high severity, co-occurring disorders, failed 30-day | More time for meds, skills, and aftercare setup | Higher cost and time away from work/home |
| 90+ days | High chronicity, repeated relapses, unstable housing | Strong habit change, comprehensive system resets | Resource intensive; needs careful step-down |
Logistics and Aftercare in New Jersey
Packing, Visitation, and Phone Policies
- Packing:
- Pack for 1–2 weeks; laundry is typically on-site weekly. Label items. Bring weather-appropriate layers.
- Visitation:
- Often limited to scheduled windows after the first 1–2 weeks, supervised or structured. Visitors may need to be pre-approved and searched. Photo ID required.
- Phones and devices:
- Expect limited access early on; calls are scheduled. Devices may be held and returned at approved times to reduce triggers.
- HIPAA releases:
- If you want loved ones to get updates, sign a Release of Information specifying who, what, and for how long. You can revoke at any time.
Transportation and Arrival Options
- Public transit:
- NJ Transit rail and bus can connect most of the state; plan routes to the nearest station to your facility.
- Airports:
- Newark Liberty International (EWR) is the primary hub; some use Trenton-Mercer (TTN) regionally.
- Pickups:
- Facilities may offer scheduled pickups from transit hubs. If not, arrange a rideshare with a sober escort if possible.
- Hospital or detox transfer:
- Coordinate nurse-to-nurse report and direct transport to avoid gaps in care or missed MAT doses.
Aftercare, Alumni, and Relapse Prevention
- Alumni follow-up:
- Expect outreach calls/messages at 7, 30, and 90 days where possible. Verify cadence and point of contact.
- Naloxone:
- You and your family should receive naloxone education and a kit. Ask where to get refills; many NJ pharmacies dispense without a patient-specific prescription.
- 90-day relapse prevention calendar (template)
- Weeks 1–2: Attend PHP/IOP 4–5 days/week; confirm MAT prescription and pillbox setup; daily peer support meeting; finalize sleep schedule.
- Weeks 3–4: Add family session; rehearse high-risk scenario coping; build 3-person recovery network; start simple exercise routine.
- Weeks 5–6: Review and adjust meds; start volunteering or structured day activity; upgrade coping plan after two real-life tests.
- Weeks 7–8: Reduce IOP frequency if stable; plan for work re-entry or classes; revisit trauma stabilization skills.
- Weeks 9–12: Lock in weekly therapy; attend 2–3 mutual-help or SMART Recovery meetings; schedule primary care and dental; refresh naloxone.
- Local mutual-help options:
- 12-step meetings (AA/NA), SMART Recovery, Refuge Recovery, and medication-friendly groups.
- Tools you can use now:
- Mutual-help meeting finders (by county).
- Medication reminder apps and secure pillboxes.
- Crisis and warm lines via SAMHSA
For women seeking gender-responsive programming or family-involved treatment plans, see our women’s drug rehab in New Jersey article.
Practical Checklists and Templates
Pre-Admission Checklist
- Insurance card and photo ID.
- Current medication list, doses, and prescriber contacts.
- Contact info of prior providers and therapist.
- Employer HR contact (if using FMLA/TDI).
- Names and numbers for family/friends you want involved.
- Transportation plan to the facility (backup plan set).
- Basic clothes, hygiene items (non-alcohol-based if required), and CPAP if applicable.
Verification and Quality Checklist
- DMHAS facility license verified.
- Accreditation: Joint Commission or CARF (ask for certificate).
- Physician addiction board certification or equivalent experience confirmed.
- Staff ratios by shift are documented.
- MAT availability and protocol reviewed.
- Outcomes one-pager received (retention, readmission, PROs).
- Grievance process explained.
Insurance Appeal Notes (Fill-In)
- Plan name/ID:
- Initial authorization dates:
- Denial date and reason:
- Clinical highlights supporting 60-day need:
- ASAM dimensions documenting risk:
- Treating clinician name/phone:
- Appeal filed (date/time/person spoken with):
- External review requested (date):
Packing Quick List
- Must bring: ID, insurance card, meds list, comfortable clothes, closed-toe shoes, and a list of emergency contacts.
- Optional: small notebook, non-glass water bottle, photos.
- Do not bring: illegal substances, weapons, large amounts of cash, scent-heavy products, or unsealed OTC meds.
How Rolling Hills Recovery Center Approaches 60-Day Care
- Evidence-based care and holistic supports: CBT/DBT skills, trauma-informed therapy, MAT when indicated, mindfulness, and movement.
- Family engagement is built into the plan and aligned with discharge goals.
- Step-down planning to PHP/IOP plus alumni touch points to reduce gaps in care.
Ask us for our current licensure, accreditation status, staffing ratios, and outcome summaries. You should have that transparency before you decide.
Helpful External Resources
- New Jersey Division of Mental Health and Addiction Services: https://www.nj.gov/humanservices/dmhas/
- NJ FamilyCare (Medicaid) eligibility and benefits: https://www.njfamilycare.org/
- NJ Department of Banking and Insurance mental health parity: https://www.nj.gov/dobi/bulletins/blt24_14.pdf
- U.S. Department of Labor FMLA: https://www.dol.gov/agencies/whd/fmla
- SAMHSA treatment and recovery resources: https://www.samhsa.gov/

Conclusion
A 60‑day rehab in NJ makes sense when 30 days didn’t stick. Check licensing & outcomes, expect evidence‑based care and aftercare. Verify credentials, understand coverage, and plan step‑down.
Frequently Asked Questions (FAQs)
What is a 60 Day Rehab New Jersey Program, and Who Actually Needs It?
A 60 day rehab New Jersey program is an extended residential level of care for substance use disorders when 30 days wasn’t enough or clinical severity is high. It fits people with recent relapse, co‑occurring mental health conditions, complex withdrawal histories, or unstable home settings.
Clinically, this often aligns with ASAM 3.5–3.7 levels of care. Always verify the facility’s New Jersey DMHAS license before admission via the state’s site at the New Jersey Division of Mental Health and Addiction Services. Ask for an in‑person or telehealth assessment, meds reconciliation, and a written plan covering detox handoff (if needed), medication‑assisted treatment (MAT), and step‑down after discharge.
What Happens Day to Day in a 60 Day Rehab Program?
Expect a tightly structured day: medical check‑ins, MAT when indicated, individual therapy, skills groups (often CBT & DBT), trauma‑informed sessions, family work, nutrition, peer support, plus evening recovery activities. Evidence‑based psychotherapies like cognitive behavioral therapy are standard; see the National Institute of Mental Health on psychotherapy basics. MAT for opioid or alcohol use disorders should follow federal guidance; review SAMHSA on medications for SUD. Weekends should include relapse‑prevention, leisure in recovery, and discharge planning touchpoints; if you don’t see a schedule with clinical minutes and staff roles, red flag.
How Does Insurance Work for 60 Day Rehab and What Will it Cost?
It depends, but here’s the short answer. Costs vary by setting, staffing, and insurance contracts. Many plans require prior authorization and ongoing utilization review. Do three things:
1. Call your insurer and ask for 60‑day residential SUD benefits, required copays/coinsurance, and in‑network options.
2. Request parity protections in writing.
3. If you have NJ Medicaid, check NJ FamilyCare.
Have the provider run a full benefits verification, provide a good‑faith estimate, and explain appeals, single‑case agreements, and any out‑of‑pocket exposure. If a center can’t show denial/appeal pathways and your parity rights, push back.
How Do I Verify Quality and Safety for a 60 Day Rehab Provider?
Use a simple checklist:
License: Confirm active NJ DMHAS licensing.
Accreditation: Ask for the current certificate from The Joint Commission or CARF.
Staff: Verify physician oversight, psychiatric coverage, nursing ratios, and counselor credentials.
Data: Request last 12 months’ program metrics—30/60/90‑day retention, completion rates, readmissions, overdose events, MAT continuity at discharge, and patient‑reported outcomes.
Safety: Review medication policies, detox handoffs, incident reporting, and emergency transfers.
No data, no deal. A 60 day rehab New Jersey program should share de‑identified outcomes and credentialing on request, not vague claims.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts