Seeking inpatient drug rehab in New Jersey can feel overwhelming. A medical addiction specialist breaks down what inpatient care is, who benefits, and how treatment plans, medications, and therapy work together for safe, sustainable recovery. This introduction prepares adults and families to understand admissions, costs & insurance, and the steps that follow discharge.
Key Takeaways
- Inpatient rehab in NJ provides 24/7 care & withdrawal monitoring with a steady daily routine; most helpful for moderate to severe substance use, or when home triggers and medical or mental health risks make outpatient tough.
- Early on, expect intake, labs, and a personalized plan; evidence-based therapies (CBT, MI, relapse prevention), plus MAT when needed. Safety first. Skills next.
- Costs vary by length of stay, staffing, and meds. Verify insurance benefits up front, ask for in-network estimates, save EOBs, and appeal denials quickly. FMLA or short-term disability can protect work.
- Quality matters: licensed clinicians, accredited programs (Joint Commission or CARF), clear detox protocols, transparent pricing; avoid “guaranteed cures” or vague claims. Plan discharge early with MAT, PHP/IOP, family support & 30/90-day follow-ups.
What Inpatient Drug Rehab is and Who Benefits
Inpatient drug rehab (also called residential treatment) provides 24/7, structured care in a live‑in setting. The goal is stabilization, safety, and skill-building, with support for withdrawal management when needed. Programs are staffed by medical and behavioral health professionals who guide patients through detox (if indicated), treatment planning, therapy, and recovery routines without the distractions or risks present at home.
Who benefits most:
- Individuals with moderate to severe substance use disorders who need a safe environment to stop using and stabilize.
- People with a history of overdose, complicated withdrawal, or medical/psychiatric issues that make outpatient care risky.
- Patients who tried outpatient care but continue to relapse.
- Those with co‑occurring mental health disorders who need a structured milieu and coordinated care.
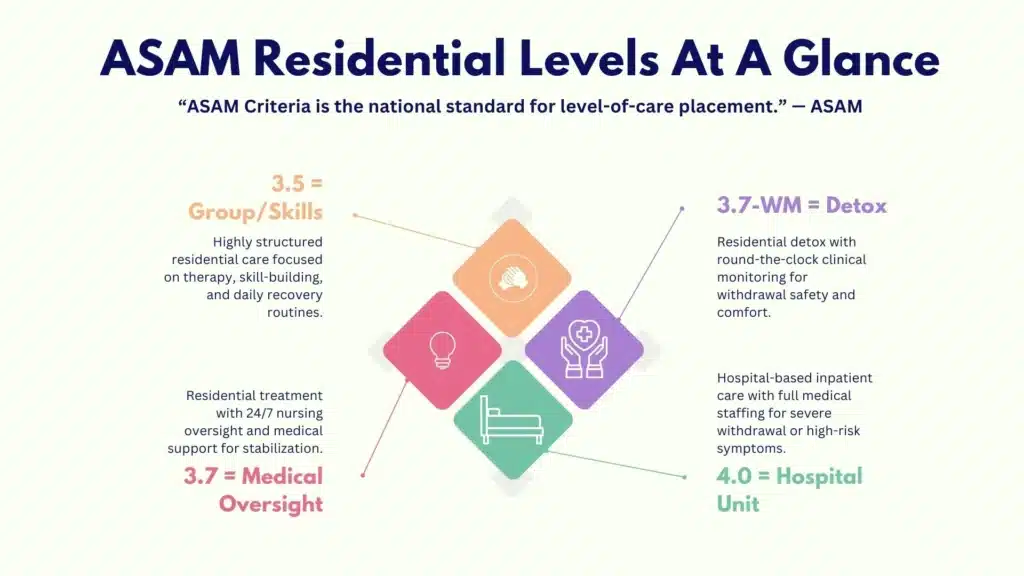
Placement is guided by the ASAM Criteria, which helps clinicians match people to the least restrictive, safe level of care. Inpatient/residential levels commonly used include ASAM 3.5 and 3.7. When withdrawal is complicated, ASAM 3.7‑WM (medically monitored withdrawal management) or ASAM 4.0 (hospital-based, medically managed intensive inpatient) may be recommended.
Typical length of stay ranges from 28 to 90 days, adjusted by clinical need, withdrawal severity, co‑occurring conditions, and response to treatment. Some patients benefit from shorter stays followed by robust step‑down care; others need a longer time to stabilize and practice skills.
How inpatient differs from outpatient:
- The environment is controlled and drug‑free, which lowers triggers, improves safety, and allows medications and therapy to work.
- The schedule is full, predictable, and supervised; patients attend therapy, groups, and skills training throughout the day.
- Medical and nursing monitoring helps address withdrawal, cravings, sleep, and nutrition, areas often overlooked in outpatient settings.
- Family work can happen in a structured way, with boundaries and education that support recovery.
Why structure helps co‑occurring disorders: Depression, anxiety, PTSD, bipolar disorder, and ADHD frequently co‑occur with substance use. Inpatient programs can stabilize medications, deliver trauma‑informed therapy, and reinforce sleep and nutrition routines that improve mood and cognition. This combination, alongside peer support, often moves recovery forward more quickly and safely.
ASAM residential and inpatient levels at a glance:
| ASAM Level | Name | Typical Setting | Key Features | Who It Helps |
|---|---|---|---|---|
| 3.5 | Clinically Managed High-Intensity Residential | Residential facility | 24/7 support, high-structure groups/therapy, focus on skill-building | Moderate–severe SUD, relapse risk, co‑occurring needs |
| 3.7 | Medically Monitored Intensive Inpatient | Residential with onsite medical oversight | 24/7 nursing availability; physician-directed services | Severe SUD, medical/psychiatric needs requiring close monitoring |
| 3.7‑WM | Medically Monitored Withdrawal Management | Residential detox unit | Physician-directed withdrawal care with nursing | Alcohol, benzodiazepine, or opioid withdrawal with risks |
| 4.0 | Medically Managed Intensive Inpatient | Hospital unit | Acute medical management; intensive monitoring | Severe/unstable medical or psychiatric conditions |
Inpatient vs outpatient care:
| Feature | On-site or coordinated | Outpatient (IOP/OP) |
|---|---|---|
| Setting | Live-in, 24/7 | Home-based |
| Safety | Highest; controlled milieu | Varies; exposure to triggers |
| Detox | On-site or coordinated | Often referred out |
| Therapy Dose | High frequency, daily | Fewer hours per week |
| Monitoring | Medical and nursing services are available | Limited medical monitoring |
| Fit | Moderate–severe SUD, relapse risk | Mild–moderate SUD, stable housing/support |
What to Expect in NJ Inpatient Care
Patients are guided by an interdisciplinary team, medical providers, nurses, addiction counselors, therapists, case managers, and peer recovery coaches, under NJ licensure standards.

Intake, Assessment, and Individualized Planning
On arrival, patients complete a comprehensive evaluation:
- Medical history and physical exam, laboratory tests as indicated (e.g., CBC, CMP, liver function, pregnancy test when relevant), and toxicology screening.
- Withdrawal risk assessment using standardized tools (e.g., CIWA‑Ar for alcohol, COWS for opioids).
- Biopsychosocial evaluation covering substance use history, mental health, trauma, housing, family, legal/employment needs, and motivation for change.
- Risk and safety assessment for overdose, suicidality, or violence.
- Medication review and coordination with outside providers when appropriate.
An individualized treatment plan is created within the first 24–72 hours, with patient input. Goals include withdrawal stabilization, medication management, core therapies, family involvement, and discharge planning from day one.
What to bring (and what not to bring) often confuses people. Use this short, practical checklist:
- Photo ID, insurance card, prescription list, and any current medications in original bottles
- Names/contacts for primary care, therapists, and emergency contacts
- Comfortable clothing, closed-toe shoes, simple toiletries (no alcohol-containing products)
- A small notebook; preferred recovery literature
- Leave valuables, weapons, and non‑prescribed substances at home; follow the program’s tobacco and vaping policy
A Realistic Daily Schedule
Days are structured to keep treatment active and focused without feeling rushed. A typical day:
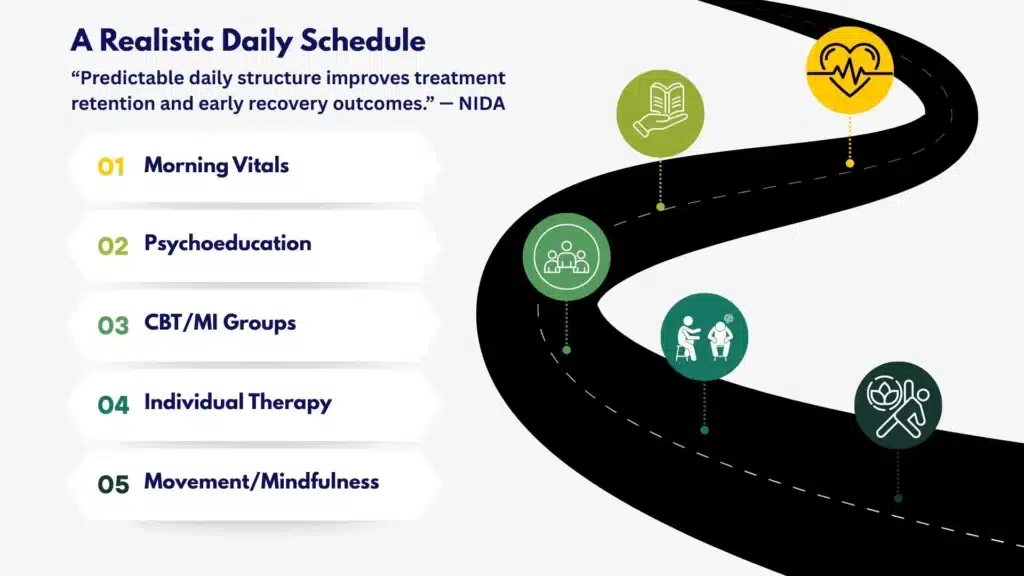
- Morning vitals, medications, breakfast, and a brief community check‑in
- Psychoeducation groups on the brain and addiction, craving cycles, and relapse prevention
- Cognitive behavioral therapy (CBT), motivational interviewing (MI), and skills groups
- Individual therapy one to two times per week, more if needed
- Family sessions (in‑person or telehealth)
- Contingency management elements (clear goals with tangible reinforcers)
- Movement, mindfulness, and recovery meetings (e.g., 12‑step, SMART Recovery)
- Nutrition-focused meals, hydration reminders, and lights‑out routines for sleep recovery
Medications for Opioid and Alcohol Use Disorders
Medication is often essential. The team explains options, verifies medical suitability, and monitors response:
- Opioid use disorder:
- Buprenorphine: a partial opioid agonist, is started after adequate withdrawal to reduce cravings and overdose risk.
- Methadone: full agonist managed through certified Opioid Treatment Programs; residential programs coordinate dosing and transitions.
- Naltrexone (oral or extended‑release): opioid antagonist used after full detoxification to block effects and reduce relapse.
- Alcohol use disorder:
- Naltrexone (oral or extended‑release): reduces reward from alcohol and cravings.
- Acamprosate: supports post‑acute withdrawal stabilization and craving reduction; best after abstinence starts.
- Disulfiram may be considered case‑by‑case; the priority is safety and adherence.
Medications are integrated with therapy and recovery supports. Patients are educated about benefits, side effects, safe use, and long‑term maintenance options.
Trauma‑Informed and Co‑Occurring Care
Many patients have trauma histories. Clinicians use trauma‑informed principles: safety, choice, collaboration, trust, and empowerment. Grounding skills, paced exposure to difficult topics, and careful medication management help stabilize PTSD symptoms.
Co‑occurring depression, anxiety, bipolar disorder, and ADHD are addressed with psychiatric consultation and medication adjustments within the structure of residential care, so patients aren’t managing these changes alone.
Peer Recovery Coaching and Family Work
Peer recovery specialists provide lived-experience support that complements clinical care. They help patients define personal recovery goals, navigate cravings in the moment, and build a support network for discharge.
Family sessions focus on communication, boundary setting, and education about enabling vs supporting. The aim is a safer, less reactive home environment that matches the patient’s treatment goals.
Privacy and Patient Rights
Substance use treatment confidentiality is protected by HIPAA and 42 CFR Part 2. Patients control consent for information sharing, including with family. Rights include:
- Informed consent for treatment and medications
- Participation in treatment planning
- The right to file a grievance without retaliation
- Access to emergency medical care and to communicate with legal representatives
Programs outline search policies, visitor rules, and contraband procedures. Staff explain each step, so patients know why policies exist and how safety is maintained for the community.
NJ Licensure and Evidence Standards
In New Jersey, residential programs are licensed by the Department of Human Services’ Division of Mental Health and Addiction Services (DMHAS). Quality programs also pursue accreditation (The Joint Commission or CARF), use ASAM placement criteria, and report outcomes.
Evidence‑Based Therapies and Medications
Core Psychotherapies
- Cognitive behavioral therapy (CBT): Targets thinking patterns and behaviors that drive substance use; patients practice triggers-and-coping drills.
- Motivational interviewing (MI): Builds intrinsic motivation without confrontation. Helpful for ambivalence.
- Dialectical behavior therapy (DBT) skills: Distress tolerance, emotion regulation, interpersonal effectiveness, and mindfulness.
- Relapse prevention therapy: Identifies high-risk situations, early warning signs, and recovery responses.
Where helpful, acceptance and commitment therapy (ACT), trauma-focused modalities, and family‑based approaches are added. Therapy is paced by clinical need and readiness to change.
Contingency Management Done Responsibly
Contingency management (CM) reinforces specific, measurable behaviors (attendance, negative drug screens, skill practice). When implemented with transparency, fairness, and cultural sensitivity, CM can improve engagement and early abstinence. Programs should clearly explain criteria, incentives, and guardrails.
Integrating Medication Treatment with Monitoring
Medication for addiction treatment (MAT) is not a stand‑alone fix. It works best when:
- Started based on a clear indication and patient preference
- Monitored with vitals, side effect tracking, and labs when needed
- Paired with therapy, housing/supports, and relapse prevention plans
- Transitioned smoothly to outpatient prescribers before discharge
Crucially, continuing MAT after discharge lowers overdose risk. Patients should leave with a bridge prescription, a confirmed follow‑up appointment, and a plan for missed doses.
Harm Reduction and Safety
Evidence supports harm‑reduction education even in abstinence-focused care. In residential settings, this includes:
- Overdose recognition and naloxone training
- Safer-use counseling for patients who may lapse after discharge
- Tolerance education to reduce post‑discharge overdose risk
- Fentanyl and xylazine awareness
- Linkage to community syringe services where legal; HIV and hepatitis screening and vaccination when appropriate
Sleep, Nutrition, and Physical Health
Sleep and nutrition are part of treatment, not add‑ons. Recovery plans target:
- Consistent sleep windows, light exposure in the morning, and movement during the day
- Hydration, adequate protein and complex carbohydrates, mineral repletion when indicated
- Addressing pain, dental issues, and chronic conditions that can undermine sobriety
Culturally Responsive and Population‑Specific Care
Quality care adapts to culture, language, gender identity, sexual orientation, age, and veteran status. Rolling Hills coordinates specialized supports and referrals as needed, including programs tailored to unique needs such as drug rehab for veterans in NJ and women’s drug rehab in New Jersey. These services often integrate trauma care, reproductive health considerations, and military/veteran cultural competence.
Measuring Progress with Validated Tools
Programs should use validated instruments to monitor change:
- Addiction Severity Index (ASI) for multi-domain assessment
- Brief Addiction Monitor (BAM) for recovery progress and risk factors
- PHQ‑9, GAD‑7, and PTSD checklists for co‑occurring conditions
- Craving scales and sleep assessments
These measures guide adjustments to therapy, medication, and discharge planning rather than relying on subjective impressions.
Overdose Education and Naloxone
Every patient and family should receive overdose education and a naloxone kit at discharge. Staff provide training on recognizing overdose, rescue breathing, and calling 911. Local pharmacies in New Jersey often dispense naloxone without an individual prescription; staff help patients locate options and add a refill plan to the aftercare packet.
Cost, Insurance, and Access
What Drives the Cost of Inpatient Rehab
- Length of stay: More days cost more, though higher acuity may compress work into fewer days.
- Level of medical care: ASAM 3.7 and withdrawal management require more clinical resources.
- Staffing ratios and credentials: 24/7 nursing, physician coverage, and licensed therapists raise costs but improve safety.
- Medications and lab work: Especially with MAT initiation or complex detox.
- Room type and amenities: Private rooms and added services increase fees; not all are clinically necessary.
Transparency matters. Ask for an itemized estimate that differentiates facility fees, professional fees, lab charges, and medication costs.
How to Verify Insurance Benefits Quickly
Most people start by calling their insurer and the treatment center. A short, organized call saves time. Patients can also use Rolling Hills’ team to verify benefits for them. For self‑verifying, use this script-like checklist:
- Call the number on the back of your insurance card for “behavioral health” or “member services.”
- Ask if your plan covers ASAM 3.5 and 3.7 residential/inpatient substance use treatment in New Jersey.
- Confirm in‑network status for Rolling Hills Recovery Center; if out‑of‑network, ask about coverage and deductibles.
- Ask about preauthorization requirements, concurrent review frequency, and how medical necessity is determined.
- Confirm your deductible, out‑of‑pocket maximum, copays/coinsurance, and whether lab work and medications are billed separately.
- Request written confirmation via your insurer’s secure message or email.
- Share this information with admissions to finalize an accurate estimate.
How to Know if Your Insurance Covers Drug Rehab in NJ. For more details on benefits and costs, see Rolling Hills’ overview of insurance coverage for rehab in New Jersey.
Parity Protections and In‑Network Options
The Mental Health Parity and Addiction Equity Act (MHPAEA) requires most plans to offer behavioral health benefits comparable to medical/surgical benefits. If a plan denies care, ask for the specific medical necessity criteria used and request a written denial. Consider filing an appeal; programs often assist with clinical documentation.
In‑network care typically reduces out‑of‑pocket costs and simplifies authorizations. If an in‑network bed is not available and medical risk is high, discuss single case agreements or gap exceptions with your insurer.
Prior Authorization Tips Without the Run‑Around
- Complete a thorough preadmission clinical with the center so the initial request matches ASAM criteria.
- Document unsuccessful outpatient trials, recent ED visits, overdoses, or safety risks.
- Align the request with the level of care and expected length of stay based on ASAM 3.5 or 3.7 criteria.
- Ask for the timeframe for decisions; escalate to a clinical reviewer if delayed.
- If denied, request a peer‑to‑peer review promptly; bring objective data (vital signs, CIWA/COWS scores, lab results, psychiatric risks).
How to Read an Explanation of Benefits (EOB)
An EOB is not a bill. It shows what was billed, what the insurer allowed, what they paid, and what you may owe. Check dates of service, CPT/HCPCS codes, and place of service (should reflect residential/inpatient). Compare against your estimate and call the insurer if the patient responsibility seems inconsistent with your benefits. Ask the provider to rebill if coding is off.
Travel, Leave, and Practical Paperwork
Admissions staff help coordinate travel to New Jersey, arrange safe pick‑up if needed, and set arrival times to align with nursing coverage. For work leave, the clinical team can complete FMLA or short‑term disability paperwork. When legal or child welfare issues are involved, case managers communicate with courts or caseworkers, with your written consent.
Scholarships and State Support
Financial assistance varies by program and eligibility. Options may include:
- State block grant funding or county resources for uninsured/underinsured residents
- NJ FamilyCare (Medicaid) plan coverage for eligible services
- Sliding‑scale scholarships from the facility when funds exist
- Public navigators such as the SAMHSA National Helpline and FindTreatment.gov to identify low‑ or no‑cost options nearby
Patients should ask admissions about which funding sources they participate in and how to apply. Admissions teams can also direct you to local recovery community organizations for added support.
Aftercare, Outcomes, and Choosing Quality
Discharge Planning and Step‑Down Care
Planning for what comes next begins on day one. Discharge options generally include:
- Partial Hospitalization Program (PHP): 5–6 days per week, several hours daily.
- Intensive Outpatient Program (IOP): 3–5 days per week, 9–15 hours total weekly.
- Outpatient therapy/medication management: Weekly or biweekly sessions.
- Recovery housing or sober living is used when a stable home environment is not yet available.
Care coordination includes scheduling first appointments, arranging transportation when possible, transferring records, and sending a clear medication list. Patients should leave with a copy of their plan and a contact person for questions.
Continuing Medications Safely
For OUD and AUD, continuing medication after discharge reduces relapse and overdose. A safe medication transition includes:
- A bridge prescription and a pharmacy confirmed to stock the medication
- A scheduled appointment with an outpatient prescriber within 7–14 days
- A backup plan if the appointment is missed
- Education about storage, missed doses, and common side effects
When methadone is used, coordination with a certified Opioid Treatment Program ensures continuity, including guest dosing if travel is involved.
Relapse Prevention Plan: A Simple Template
A written plan moves recovery from ideas to actions. Use these prompts to build a clear, personal plan:
- My top three triggers and early warning signs
- My 24‑hour coping steps if cravings spike (people to call, places to go, skills to use)
- My medication schedule and what to do if I miss a dose
- My daily recovery routine (sleep window, meals, movement, meeting schedule)
- My safe people and emergency contacts (with phone numbers)
- My “if I slip” plan (how I will get back to safety within 24 hours)
- My overdose safety plan (where naloxone is kept; who knows how to use it)
Patients review and rehearse this plan with their therapist and family before discharge.
Alumni and Family Involvement
Alumni programming offers ongoing connection, support meetings, mentorship, and events that keep motivation and accountability high. Families benefit from continued education and support groups of their own to sustain healthy boundaries and reduce relapse risk.
How to Evaluate Programs Before You Commit
Signs of quality:
- Accreditation by The Joint Commission or CARF, and licensure by NJ DMHAS
- Clear use of ASAM criteria and evidence‑based therapies (CBT, MI, DBT skills, contingency management)
- Access to MAT for OUD/AUD with safe initiation and continuity planning
- Qualified staff, including licensed clinicians, 24/7 nursing, and access to medical providers
- Transparent pricing and utilization review processes
- Trauma‑informed environment and culturally responsive care, including gender‑specific supports like women’s drug rehab in New Jersey
- Measured outcomes and willingness to share de‑identified data
Red flags:
- Guaranteed cures or fixed outcomes
- Vague pricing or refusal to provide itemized estimates
- No plan for medications or insistence that MAT is “not real recovery”
- One‑size‑fits‑all programming without individualized plans
- Limited discharge planning or no coordination with aftercare providers
If specialized needs exist, military trauma, women’s health, or veteran‑specific services, confirm programming and staff expertise up front.
Reliable programs follow up after discharge. Common checkpoints are 30 and 90 days, assessing:
- Substance use status, cravings, and recovery activities
- Medication adherence and side effects
- Mood, sleep, and safety concerns
- Housing, employment/school, and legal progress
- Connection to primary care and specialist follow‑ups
These data inform quality improvement and help the team offer extra support if a patient is struggling. Patients can opt in to regular check‑ins and secure messaging for quick problem-solving.
Finding Local Supports
Strong outcomes depend on local resources: mutual‑help meetings, therapy, MAT providers, primary care, and recovery‑friendly employers. Rolling Hills connects patients with community partners across New Jersey. Those seeking services for themselves or a loved one can explore neighborhood options or ask admissions to help identify the right level of care. If you are comparing nearby programs and need a starting point, Rolling Hills maintains an overview of local drug rehab centers and can explain how levels of care differ.
Practical Tools Patients Can Use Today
- Insurance benefits file: A one‑page summary listing deductible, out‑of‑pocket max, copays, and authorization contact information. Keep a photo on your phone.
- Medication wallet card: Current medications, dosages, prescriber names, and allergies.
- Appointment map: Dates and locations for step‑down care, with backup contact numbers.
- Naloxone plan: Where it’s stored, who is trained, and how to replenish it.
- Sleep tracker: Note bedtime/wake time and quality. Bring to your follow‑up appointments.
Patients and families can also consult impartial resources for education and access, such as the SAMHSA National Helpline, FindTreatment.gov, NIDA’s Principles of Effective Treatment, the ASAM Criteria overview, and the NJ Department of Human Services’ Division of Mental Health and Addiction Services for licensure and consumer information. Rolling Hills’ admissions team helps translate these resources into a clear, personal next step.
Conclusion
NJ inpatient rehab stabilizes use, delivers evidence-based care, and plans aftercare. Key: safety, family, clear costs & follow‑through. It’s okay to go step by step.
Frequently Asked Questions (FAQs)
What is Inpatient Drug Rehab in New Jersey, and Who Benefits?
Inpatient drug rehab is 24/7 residential care for people with moderate to severe substance use disorders, or for those who’ve tried outpatient but keep relapsing.
In NJ, it often starts with medical detox if needed, followed by a structured routine that includes daily therapy, medication for addiction treatment when appropriate, and support for co‑occurring mental health concerns.
It’s especially helpful for safety during withdrawal, stabilizing health, and building new habits away from triggers & stressors at home.
What Happens During the First Few Days of Inpatient Drug Rehab?
The team completes a full medical and behavioral health assessment, checks labs, reviews meds, and screens for withdrawal risk. If detox is needed, it’s started right away with 24/7 monitoring.
An individualized plan is then set: goals, therapy schedule, family involvement, and aftercare ideas from day one. Expect a calm routine, nursing checks, groups, one‑to‑one counseling, meals, and sleep support, nothing fancy, but steady and therapeutic.
How Long Does Inpatient Drug Rehab Last, and What Does a Day Look Like?
Length varies: commonly 28–45 days, sometimes up to 60–90 days based on medical needs, progress, and insurance approvals. A typical day includes:
Morning vitals and a brief check‑in; skills groups (CBT or relapse prevention); individual therapy; medication support (for example, buprenorphine or naltrexone when indicated); family time or education blocks; and movement, meals, sleep hygiene; some mindfulness or spirituality if the patient chooses.
The goal is simple: stabilize the brain & body, practice coping skills, and leave with a clear next‑step plan.
How Do Costs and Insurance Work for Inpatient Drug Rehab in NJ?
Most commercial plans and NJ FamilyCare/Medicaid cover medically necessary inpatient rehab, but prior authorization is common. Practical steps:
Call the number on the insurance card to verify behavioral health benefits and deductibles; ask about in‑network inpatient rehab and any pre‑cert rules. Ask the program for a benefits check and a plain‑language estimate; get it in writing. If employed, consider FMLA paperwork and short‑term disability. Save explanations of benefits (EOBs) and appeal denials quickly; medical notes and ASAM level‑of‑care criteria help. It’s okay to ask for a peer‑to‑peer review if coverage is cut early.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












