New Jersey residents deserve clear, compassionate treatment that works. This overview walks through how clinicians assess substance use, choose the right level of care, and coordinate medications, therapy, and family support. Readers learn what to expect from detox through aftercare, how to plan for costs & access, and how safety and privacy are protected.
Key Takeaways
- Care starts with a thorough screening and a full biopsychosocial assessment using ASAM dimensions; co-occurring mental health is treated together; privacy is protected under HIPAA & 42 CFR Part 2.
- Level of care is matched to risk: medical detox, outpatient, IOP, partial care, or residential; patients step up or down as needs change, not just a fixed calendar.
- Medications for opioid and alcohol use disorders are paired with CBT, DBT, and contingency management; family involvement, overdose education with naloxone, and urine testing are used to support, not punish.
- Practical steps in New Jersey include verifying insurance parity (including NJ FamilyCare), handling preauth, FMLA, and short-term disability when needed; planning transport and childcare; and calling 988 in a crisis.
Assessment and Levels of Care in NJ
What Drug Abuse Treatment Programs Are
Drug abuse treatment programs are structured medical and behavioral services designed to help people reduce or stop harmful substance use, improve health, and rebuild daily functioning.
In New Jersey, high‑quality programs combine medical care, counseling, family therapy, peer support, and recovery monitoring, with attention to social needs such as housing, legal matters, and employment.
Rolling Hills Recovery Center provides evidence-based treatments and holistic approaches under licensed clinical oversight, aligning with state and national standards.
The ASAM Dimensions in Plain Language
Most New Jersey programs use the ASAM Criteria to match a person’s needs to the right level of care. Treatment planning looks across six dimensions:
- Acute Intoxication/Withdrawal Potential: current use, risk of withdrawal, need for detox.
- Biomedical Conditions: medical issues that affect safety or care.
- Emotional/Behavioral/Cognitive Conditions: mental health symptoms, suicide risk, cognitive status.
- Readiness to Change: motivation, ambivalence, stage of change.
- Relapse/Continued Use/Continued Problem Potential: triggers, past patterns, risk factors.
- Recovery/Living Environment: housing, support, transportation, safety, legal issues.
These dimensions are reviewed at intake and at set intervals. Level of care can step up or step down as needs change, not a one‑way path.
From Screening to a Comprehensive Intake
Initial screening identifies risk quickly and determines if urgent safety steps are required.
- Screening tools often include the DAST-10, AUDIT-C, PHQ-9 for depression, and suicide screens. Brief intervention (motivational conversation) follows when appropriate.
- A comprehensive biopsychosocial intake then documents substance use history, withdrawal history, medical and psychiatric conditions, medications, family and social context, legal matters, strengths, and goals. Collateral information is gathered only with consent.
- Lab work and, when indicated, urine toxicology are used to inform care. Results are discussed openly and respectfully to support, not punish, progress.
Choosing the Right Level of Care in New Jersey
Programs align level of care with risk, stability, and support. The table below summarizes common options.
| Level of care (ASAM-aligned) | Who it’s for (typical indications) | Core elements | Typical duration (variable) |
|---|---|---|---|
| Ambulatory Withdrawal Management (Outpatient Detox) | Mild–moderate withdrawal risk; stable housing; daily check-ins feasible | Daily nursing/medical visits; withdrawal medications; safety checks; rapid transition to counseling/MAT | 3–7 days, then transition |
| Inpatient/Residential Withdrawal Management (Detox) | Moderate–severe withdrawal (e.g., alcohol with seizure risk, benzodiazepines), unstable vitals, polysubstance, pregnancy, limited support | 24/7 nursing and medical care, symptom monitoring, medications, safety | 3–10 days, then step-down |
| Outpatient (OP) | Lower severity; stable work/school; strong support | 1–3 therapy sessions/week; case management; urine toxicology as needed | Weeks to months |
| Intensive Outpatient (IOP) | Moderate severity; need for structure; co-occurring issues are manageable in an outpatient setting | 9–19 hours/week groups + individual therapy; MAT; family work | 6–12 weeks on average |
| Partial Hospitalization/Partial Care (PHP) | High severity; daytime structure needed; medical/psychiatric monitoring but not 24/7 | 20+ hours/week; psychiatry; nursing; intensive therapy; contingency management | 2–6 weeks |
| Residential/Inpatient Rehab | Unsafe environment; repeated relapse; major functional impairment | 24/7 structured milieu; medical and psychiatric care; integrated therapies | 2–6+ weeks; step-down after |
| Recovery Housing (not treatment) | Supportive living while in outpatient care | Drug- and alcohol-free residence; peer accountability; curfew | As clinically useful |
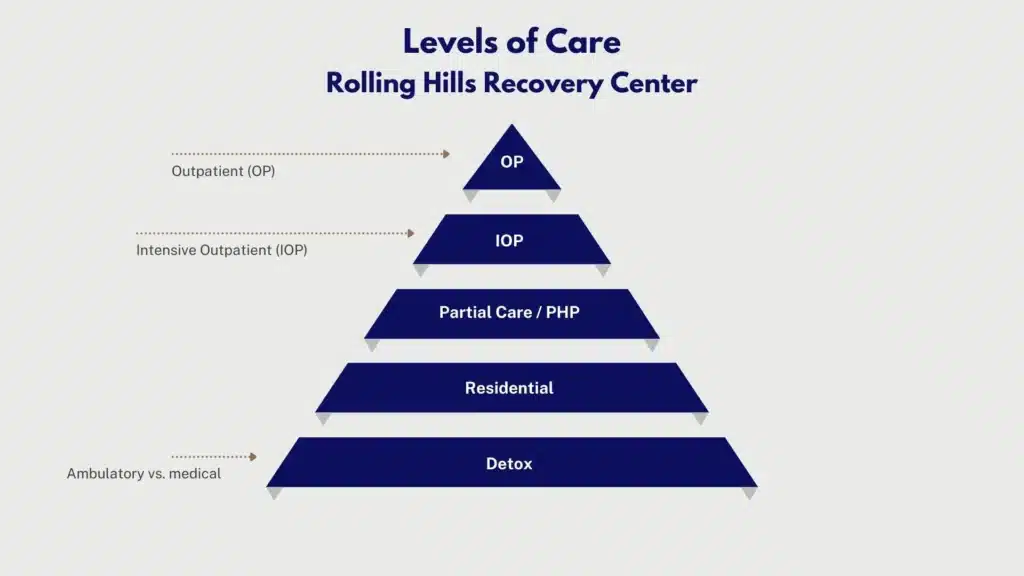
Programs like Rolling Hills Recovery Center support movement up or down based on ASAM re-assessment and progress, not a fixed calendar.
When Medical Detox is Needed vs Outpatient, IOP, Partial Care, Residential
- Consider medical detox for substance abuse when there is past severe withdrawal (seizures, delirium tremens), daily alcohol or benzodiazepine use, heavy opioid use with medical instability, pregnancy, or significant medical comorbidity. Detox alone is not treatment; immediate transition to ongoing care prevents relapse.
- Consider PHP or residential when use is daily with safety risks, co-occurring psychiatric instability, high environmental triggers, or multiple recent relapses despite lower care.
- Consider IOP when motivation is present but day-to-day triggers are strong, or when co-occurring symptoms or cravings require more structure.
- Consider OP when use is less frequent, risks are low, supports are stable, and goals are focused on maintenance and skill-building.
Care for Co-Occurring Mental Health Disorders
Integrated care is the standard. Depression, anxiety, PTSD, bipolar disorder, ADHD, and psychotic disorders should be treated in the same program whenever possible. Expect:

- Coordinated psychiatric evaluation and medication management.
- Therapies with evidence for co-occurring disorders, such as CBT, DBT skills, Seeking Safety, and trauma-focused CBT components, are delivered when the person is stable enough.
- Screening for suicide risk with clear crisis protocols and 988 access.
Medications for Addiction Integrated with Therapy
Medication for opioid use disorder (MOUD), buprenorphine, methadone (via OTP), and naltrexone, reduce mortality and promote retention. For alcohol use disorder, naltrexone, acamprosate, and disulfiram are considered. Best practice integrates medication with:
- Cognitive Behavioral Therapy (CBT) is used to change thought patterns and habits.
- Dialectical Behavior Therapy (DBT) skills for emotion regulation and distress tolerance.
- Contingency Management (CM), which uses small, immediate rewards for objective recovery behaviors (attendance, negative toxicology, medication adherence).
- Motivational interviewing to reduce ambivalence and support change.
Family Engagement and Privacy Under 42 CFR Part 2
Family and supportive others often help recovery stick. With consent, programs can include family in education, boundary setting, and relapse-prevention planning. However, 42 CFR Part 2 sets strict rules on sharing substance use treatment information. Key points:
- No disclosure without a valid, written patient consent (with specific recipient, purpose, and what can be shared), unless a narrow exception applies.
- Patients can revoke consent at any time.
- Courts and probation require specific, time-limited consents; general medical releases are not enough.
- In emergencies, limited disclosure may occur to protect life. Documentation must be precise.
Family can still receive general education on addiction without discussing a person’s protected information. Programs should explain these basics at intake so everyone understands how to communicate.
Core Components and What to Expect
The Individualized Plan and Measurable Goals
Treatment plans should be personal and practical. A strong plan includes:
- Problems and strengths are stated in plain language.
- SMART goals (specific, measurable, achievable, relevant, time‑bound).
- Objectives tied to ASAM dimensions (e.g., “Reduce daily alcohol use to zero with naltrexone; attend IOP 4 days/week; identify 5 high-risk situations and coping strategies.”).
- Assigned interventions (CBT sessions, CM schedule, family sessions, medication visits).
- Target review dates aligned to progress.
Clinicians review and adjust the plan regularly. Goals can be harm-reduction oriented (e.g., reduce use, avoid overdose) and progress toward abstinence as appropriate.
What Sessions Look Like
Expect a mix of individual therapy, skills groups, medication visits, and peer services. Sessions are structured, often with brief check-ins, skills teaching, practice, and take-home assignments. If trauma is present, therapy follows trauma-informed principles: safety first, choice, collaboration, empowerment, and cultural responsiveness. Pace matters; rushing trauma processing can backfire.
Peer Support and Mutual-Help Choices
Peer recovery specialists bring lived experience and practical coaching. Patients choose mutual-help options that fit their values, AA/NA, SMART Recovery, Refuge Recovery, Women for Sobriety, or faith-based groups. Programs should not force a single pathway.
Relapse-Prevention Skills
Core skills include trigger mapping, craving management (urge surfing, delay/decide strategies), sleep hygiene, mood regulation, scheduling sober rewards, refusal skills, and building sober social networks. CM can reinforce these behaviors in small, frequent ways.
Overdose Education and Naloxone
All patients and families should receive overdose education. Naloxone is recommended for anyone at risk or living with someone at risk. Training covers recognizing overdose, calling 911, rescue breathing, and using naloxone nasal spray. In NJ, pharmacies can dispense naloxone without an individual prescription.
Recovery Monitoring, Urine Toxicology, and a Non-Punitive Approach
Urine toxicology and breathalyzer testing are tools to inform care, not punish. Best practice:
- Explain testing upfront, including frequency and how results are used.
- Discuss results collaboratively; when unexpected results occur, increase support or adjust medications and safety plans.
- Avoid automatic discharge for use. Return-to-use is treated as a clinical signal, not a failure.
Timelines Adjust to Progress
Length of treatment is individualized. While insurers sometimes authorize in blocks (e.g., 1–2 weeks), clinical teams advocate for ongoing care when medically necessary. Progress is reflected in engagement, reduced use, improved health, and safer behaviors, not just abstinence alone.
Helpful Templates and Tools
- Brief personal safety plan: warning signs, internal coping steps, people/places for distraction, family and clinician contacts, steps to make the home safer (lockboxes, disposal of unused medications), when to call 988 or 911.
- Medication tracker: daily dose checklist, side effects, refill dates.
- Recovery routine planner: weekly schedule for sleep, meals, movement, meetings, therapy, and rewards.
Rolling Hills Recovery Center uses measurement-based care to adjust plans, combining evidence-based care with counseling and holistic supports. Readers interested in structured drug abuse counseling can explore options aligned with these practices.
Access, Costs, and Practical Steps in New Jersey
Insurance Coverage and Parity, Including NJ FamilyCare
Under federal and NJ parity laws, most commercial plans and NJ FamilyCare (Medicaid) must cover substance use disorder treatment similar to medical/surgical benefits. Key points:
- Covered services often include detox, residential, PHP, IOP, OP, medication visits, and labs.
- Prior authorization (preauth) may be required. Programs submit clinical notes aligned to ASAM dimensions to justify level of care.
- Network status matters for cost-sharing, but out-of-network benefits may apply.
How to verify benefits, step by step:
- Call the number on the insurance card; ask for behavioral health/substance use benefits.
- Ask for coverage details by level of care (OP, IOP, PHP, residential, detox), copays/coinsurance, deductibles, and prior authorization requirements.
- Confirm coverage for medications (buprenorphine, naltrexone, oral, and extended-release).
- Request information on transportation benefits if on NJ FamilyCare.
- Document the call reference number and representative name.
Preauthorization Tips
- Provide recent clinical notes, withdrawal risk, medical/psychiatric comorbidities, living environment stressors, and past treatment history.
- Link every requested service to an ASAM dimension.
- If denied, ask for the denial rationale in writing and file an expedited appeal when a safety risk is present.
Employer Leave and Short-Term Disability Basics
- FMLA provides up to 12 weeks of unpaid, job-protected leave for eligible employees for serious health conditions, which include substance use disorders when treated by a health professional.
- New Jersey Temporary Disability Insurance (TDI) may provide partial wage replacement if unable to work due to a disabling condition, including treatment and recovery periods certified by a clinician.
- Keep documentation secure. Programs can provide work notes that protect privacy under 42 CFR Part 2 (disclose only what is necessary, with consent).
Transportation Options
- NJ Transit bus and rail may suffice for OP/IOP; ask about reduced fares or disability passes when applicable.
- NJ FamilyCare members may access non-emergency medical transportation for covered services; schedule ahead.
- Some programs offer or coordinate rideshares or shuttle services based on need.
Childcare Planning
- Ask the program about onsite or partner childcare options. If none, coordinate with family or licensed providers during session hours.
- Build a contingency plan: backup caregivers, written consent for caregivers to seek emergency care for the child, and a simple schedule.
Safety Planning and Crisis Resources
A brief written plan is recommended for everyone beginning care, and it should be revisited. Include:
- Top personal triggers and early warning signs.
- Three coping steps to try before calling someone.
- Names and numbers of 1–2 supportive people.
- How to make the home safer (lock up medications & remove paraphernalia).
- When to call 988 (suicidal thoughts, escalating distress) or 911 (overdose, immediate danger).
What to Bring to an Intake or First Session
- Government ID and insurance card (or NJ FamilyCare info).
- Current medication list (name, dose, prescriber) and allergies.
- Past treatment records, if available; hospital discharge summaries; lab results.
- Legal paperwork if relevant (probation terms, court orders).
- Contact information for primary care, psychiatrist, and any case managers. Signed consents will be completed at intake, so coordination stays compliant.
Coordinating with Primary Care, Psychiatry, and Courts
- Sign 42 CFR Part 2-compliant releases for specific providers and agencies. Separate consents are needed for primary care, therapist, probation officer, and any court.
- Ask for a single point of contact on the treatment team. That clinician or case manager can send progress updates (attendance, medication adherence, general progress) per consent terms.
- Courts and probation typically request attendance and toxicology summaries. Programs should share the minimum necessary information, time-limited.
- Return-to-use events are handled clinically first. Legal stakeholders are notified per consent language, not by default.
Getting Started in New Jersey
- Call a licensed provider and request a same- or next-day screening. If unsure where to start, the NJ Department of Human Services DMHAS website lists public resources and hotlines.
- If short on time or juggling work, ask about evening IOP, telehealth options when clinically appropriate, and medication starts before full program entry.
- Programs like Rolling Hills Recovery Center offer pathways for adults; specialized treatment for substance abuse in NJ can be matched to age, substance type, and co-occurring needs. Those managing prescribed medications with misuse concerns can also review focused prescription drug addiction treatment.
Outcomes, Quality, and Aftercare
Measuring Outcomes That Matter
Quality programs track and share results. Common metrics:
- Engagement: percent attending a second visit within 7 days of intake.
- Retention: percent still in care at 30 and 90 days.
- Medication adherence: percent of eligible patients on MOUD or AUD medications; refill persistence.
- Use-related outcomes: reduction in use days, negative toxicology rates, fewer ED visits or hospitalizations.
- Functioning: housing stability, employment/school participation, legal events, quality-of-life scores.
Measurement-based care means using brief, repeated tools, craving scales, symptom checklists, urine toxicology, blood pressure/weight for med monitoring, to adjust treatment in real time.
Harm-Reduction Goals and Managing Return-to-Use
Abstinence is a valid goal for many. For others, harm reduction is a safer first step: fewer use days, safer use practices, avoiding overdose, and stabilizing housing and health. Programs should:
- Avoid “discharge for relapse” policies. Instead, they increase support, adjust medications, or step up level of care.
- Offer naloxone to all. Educate on tolerance loss after detox or incarceration.
- Maintain engagement even if a person is not ready to stop fully; motivation often grows with continued contact.
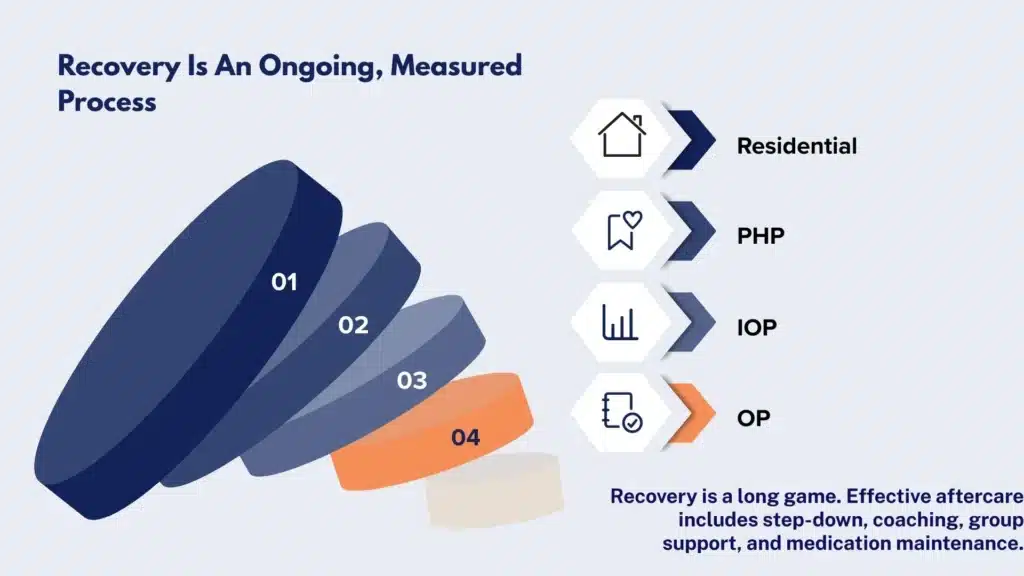
Aftercare and Continuing Care
Recovery is a long game. Effective aftercare usually includes:
- Step-Down: from residential to PHP, then IOP, then OP as milestones are met.
- Mutual-Help: AA/NA, SMART Recovery, or other groups that fit the person’s beliefs and schedule.
- Recovery Coaching: peer support to navigate triggers, jobs, school, and court requirements.
- Medication Maintenance: continue buprenorphine or naltrexone as long as benefits outweigh risks, often 12 months or more. Medication duration is individualized; premature tapering raises relapse risk.
- Medical Follow-Up: primary care for preventive care, hepatitis C and HIV screening, vaccines, and management of chronic conditions.
- Family Support: periodic family sessions, education refreshers, boundary planning for home stressors.
Choosing Programs with Quality Signals
When comparing programs in New Jersey, look for:
- Accreditation by The Joint Commission or CARF.
- Use of ASAM Criteria for assessment and level-of-care decisions.
- Integration of medications for addiction with counseling.
- Contingency management and evidence-based psychotherapies (CBT, DBT skills).
- Trauma-informed care practices and co-occurring psychiatric care are onsite or tightly coordinated.
- Measurement-based care with outcome reporting.
- Clear policies for non-punitive urine toxicology and managing return-to-use.
- Family engagement is compatible with 42 CFR Part 2.
Programs should also align with guidance from federal agencies and NJ DMHAS. Rolling Hills Recovery Center emphasizes these standards while providing local access, experienced clinicians, and practical supports tailored to New Jersey residents.
Special Populations and Age-Specific Care
Adolescents benefit from family-based approaches, school coordination, and developmentally appropriate groups. Older adults may need medication reviews for interactions, mobility supports, and focus on chronic disease.
Pregnant patients require obstetric collaboration and MOUD when appropriate. NJ programs should offer or coordinate specialty tracks; families seeking adolescent options can explore youth-focused resources alongside adult care planning.
Using Results to Refine the Plan
A person’s post-acute phase often involves adjusting visit frequency, targeted skills practice, and gradual exposure to higher-risk settings with support. Regular plan reviews, monthly or more often, look at:
- What’s working: medications, skills, peer contact, housing stability.
- What’s not working: barriers to attendance, side effects, and specific triggers.
- Next steps: add CM if motivation is low; trial extended-release naltrexone if cravings persist on oral naltrexone; step up to IOP if OP isn’t enough structure; problem-solve transportation or childcare.
If legal obligations exist, the team uses consented updates to demonstrate progress, which can improve court outcomes.
Cost Transparency and Outcome Reporting
Ask programs for a plain-language estimate of costs (by level of care), typical insurance approvals, and any payment plans. Quality programs publish or share aggregate outcomes at least yearly. This transparency helps families and referral sources know what to expect.
Practical Tools to Sustain Gains
- A small relapse-prevention card in a wallet or phone: personal top three triggers, three coping steps, sponsor/peer number, 988.
- Calendar reminders for medication and refill dates.
- Digital mutual-help meetings when travel is hard.
- Routine “recovery checkups” at 3, 6, 9, and 12 months, quick visits or calls to catch issues early.
References and Tools (Non-Competing, Evidence-Focused)
- NIDA – Principles of Effective Treatment: https://nida.nih.gov/sites/default/files/podat-3rdEd-508.pdf
- SAMHSA – Evidence-Based Practices Resource Center: https://www.samhsa.gov/resource-search/ebp
- ASAM Criteria overview: https://www.asam.org/asam-criteria/about
- NJ Department of Human Services – Division of Mental Health and Addiction Services: https://www.nj.gov/humanservices/dmhas/
Conclusion
New Jersey residents can choose care that fits their needs by starting with a solid assessment, matching the right level, and blending medication & therapy. Remember insurance basics, safety planning, and aftercare, small steps, steady wins.
Frequently Asked Questions (FAQs)
What do Drug Abuse Treatment Programs in New Jersey Include?
Drug abuse treatment programs in New Jersey start with a clinical assessment that reviews substance use history, withdrawal risk, mental health, medical needs, family supports, and safety.
Care is then matched to the ASAM level: ambulatory detox or inpatient detox for withdrawal, standard outpatient, intensive outpatient (IOP), partial hospitalization, or residential care.
Effective programs blend FDA-approved medications for opioid or alcohol use disorders (MAT) with evidence-based therapy such as CBT & DBT, trauma-informed care, contingency management, and family sessions. Co-occurring disorders (depression, anxiety, PTSD) are treated at the same time, not later.
Privacy is protected under HIPAA and 42 CFR Part 2. Relapse prevention, overdose education with naloxone, and recovery monitoring are built in.
How Should Someone Choose Among Drug Abuse Treatment Programs in NJ?
Start with a comprehensive evaluation; it should cover substances, mental health, medical status, and social needs.
Ask if the program provides medications for opioid and alcohol use disorders, plus weekly therapy and family involvement.
Confirm the level of care recommended (detox, IOP, residential) and that step-down and aftercare are planned from day one.
Verify insurance, transportation, and work or school coordination (FMLA/short-term disability when needed).
Also check accreditation, the use of measurement-based care (regular symptom and craving tracking), and policies that treat return-to-use as a clinical signal, not grounds for discharge. If safety is a concern, call 988 for immediate support and then return to treatment decisions once stable.
What Do Drug Abuse Treatment Programs in NJ Cost, and is Insurance Accepted?
Costs vary by level of care. Detox and residential are higher; outpatient, IOP, and partial hospitalization are generally lower. Most New Jersey programs accept commercial plans, Medicare, or NJ FamilyCare due to parity laws, though prior authorization may apply.
Ask about in-network status, deductibles, and copays; request a written estimate and help with preauthorization. Many employers offer FMLA and short-term disability for treatment time.
If needed, ask about payment plans, limited sliding scales, or transportation help; small supports often remove big barriers.
How Long Do Drug Abuse Treatment Programs Take in New Jersey, and What Happens After?
Timelines are individualized. Detox can last 3–7 days; residential may run 2–6 weeks (sometimes longer), partial hospitalization about 2–4 weeks, and IOP often 8–12 weeks.
Medication for opioid or alcohol use disorders may continue for months or years; that’s normal and evidence-based.
Aftercare includes step-down to a lower level, ongoing counseling, MAT & recovery coaching when helpful, urine toxicology used therapeutically, and linkage to mutual-help or faith-based recovery communities if desired.
Plans adapt to progress, care is adjusted, not simply ended, when a person struggles.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












