Recovery from substance use is achievable with the right plan and support. From medically supervised detox for substance abuse & medication options to therapy, family involvement, and aftercare, this overview explains what works, why it works, and how to get started. Written from a clinician’s perspective, it guides adults toward safe, informed decisions for lasting change.
Key Takeaways
- Match care to need: detox, residential, PHP, IOP, or outpatient, stepping up or down as risks change, not one-size-fits-all
- Medications & therapy together work best; MOUD plus CBT, motivational work, and family support lowers relapse and improves safety
- Plan aftercare from day one… MAT maintenance, relapse prevention skills, and steady follow‑ups keep recovery on track
- Start simply: medical assessment and an insurance benefits check; confirm coverage, costs, transport, privacy, then schedule intake
What Rehab for Substance Abuse Means and What It Aims To Do
Rehab for substance abuse is a structured medical and behavioral program that helps people stop or reduce harmful alcohol and drug use, stabilize their health, and build skills to live well.
At Rolling Hills Recovery Center in New Jersey, care is delivered by a multidisciplinary team, including therapists and case managers, using evidence-based practices and holistic supports.
It is not “one size fits all.” The right plan depends on medical risks, the substances involved, psychiatric needs, motivation, and the safety of the home environment.
Who benefits most:
- People at risk for dangerous withdrawal (alcohol, benzodiazepines, heavy opioids).
- Those with impaired daily functioning, work, school, parenting, or legal difficulties.
- Individuals whose home setting is unsafe, unstable, or not conducive to recovery.
- People who have tried outpatient care but continue to return to use.
Core aims:
- Skill-building: coping skills, craving management, life structure, communication.
- Relapse risk reduction: medications when indicated, therapy, peer support, and environmental changes that lower triggers.
Treatment duration matters. Research summarized by the National Institute on Drug Abuse notes that longer engagement, about ~90 days of continuous treatment and recovery support across levels of care, is associated with better outcomes, including lower return-to-use and improved functioning.
That does not always mean 90 days in one setting; stepping down across levels while maintaining structure counts and often works best.
Rolling Hills Recovery Center blends therapeutic care with practical, day-to-day counseling. The team focuses on sustainable routines and movement, alongside therapy and medications when appropriate. That blend is what helps stick, long after discharge.
Levels of Care and Matching Severity

The ASAM Multidimensional Assessment
Placement into the right level of care is guided by a multidimensional assessment, often described using the ASAM Criteria. Clinicians evaluate:
- Acute intoxication or withdrawal potential (risk of severe withdrawal, seizure, delirium).
- Biomedical conditions and complications (pregnancy, infections, liver disease, pain).
- Emotional, behavioral, or cognitive conditions and complications (depression, trauma, ADHD).
- Readiness to change (motivation, ambivalence).
- Relapse, continued use, or continued problem potential (history of return-to-use).
- Recovery environment (housing safety, supportive family, transportation, access to substances).
This framework helps determine where to start, when to step up, and when to step down.
Level-of-Care Options
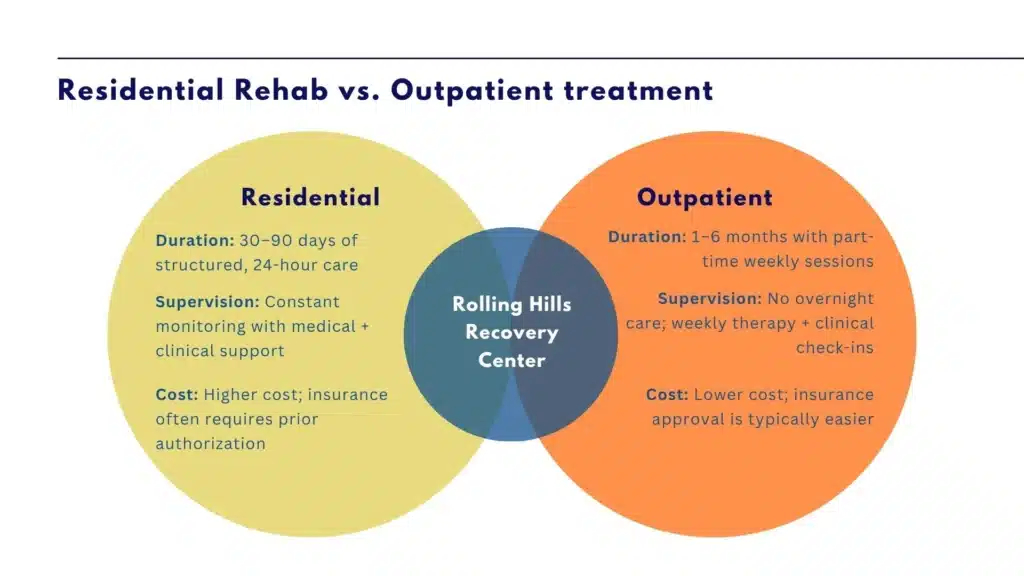
Here are common levels of care, who they fit, and typical lengths of stay. Individual plans vary based on progress and goals.
| Level of care | Who it’s for | Typical length-of-stay range | Focus |
|---|---|---|---|
| Medical Detox (Inpatient Withdrawal Management) | Risky alcohol, benzo, or opioid withdrawal; unstable vitals; complex medical issues | 3–7 days (sometimes longer) | Therapeutic immersion, structure, family engagement, and co-occurring care |
| Residential/Inpatient Rehab | Unsafe home setting, high relapse risk, severe symptoms, or failed lower levels | 2–6 weeks, often longer for complex cases | Needs intensive daily therapy without an overnight stay; transitioning from residential |
| Partial Hospitalization Program (PHP) | Therapy, medications, monitoring, recovery coaching, and alumni supports | 2–4 weeks on average | 5–7 days/week, 5–6 hours/day; skills, medication management, relapse prevention |
| Intensive Outpatient Program (IOP) | Step-down from higher care or step-up from standard outpatient; moderate stability | 6–12 weeks (flexible) | 3–4 days/week, group and individual therapy, family work |
| Outpatient Counseling/Medication Management | Stable housing and support; working or in school; maintenance phase | Ongoing (months to years) | Therapy, medications, monitoring, recovery coaching, and alumni support |
Step-Up/Step-Down Pathways and Duration
People commonly enter at the level matching current risk, then step down as stability improves. For example: medical detox → residential → PHP → IOP → outpatient and recovery support. If risks rise, strong cravings, new stressors, positive urine tests, or missed sessions, stepping back up prevents crises.
Length of stay is individualized. Rolling Hills Recovery Center encourages a full 90-day recovery arc across settings. This could look like 10 days of detox, 21 days of residential, 20–30 days of PHP or IOP, and ongoing outpatient care with medications and peer supports. The arc matters more than any single level.
Evidence-Based Treatments and Medications
Combining therapies and medications improves retention and outcomes. Medications for opioid use disorder, in particular, reduce all-cause mortality substantially and cut overdose risk. Therapy builds skills patients can use daily. Together, they work.
Core Psychosocial Therapies
- Cognitive Behavioral Therapy (CBT): identifies triggers, reshapes thinking, and teaches coping skills. Patients learn to map a trigger-thought-feeling-action chain and insert practical alternatives like urge surfing or delay-distraction tactics.
- Motivational Interviewing (MI): enhances motivation and commitment through non-confrontational conversation, resolving ambivalence.
- Contingency Management (CM): uses small, structured rewards for objective evidence of progress (attendance, negative toxicology). Especially helpful for stimulants and cannabis.
- Family therapy: involves partners and family in boundary-setting, communication, and relapse-prevention plans, which increases support and lowers conflict at home.
- Trauma-informed care: safety-first approach, with EMDR or other therapies when appropriate, to address trauma without destabilizing recovery.
Rolling Hills Recovery Center integrates most of these in individual, group, and family sessions. For dedicated counseling information, see the center’s page on substance abuse counseling in NJ.
Medications for Opioid and Alcohol Use Disorders
Opioid use disorder:
- Buprenorphine (includes extended-release options): reduces withdrawal and cravings, lowers relapse risk, and stabilizes brain chemistry.
- Methadone: highly effective for long-standing or severe opioid dependence; provided through opioid treatment programs with daily or take-home dosing when stable.
- Naltrexone (extended-release monthly injection): opioid blocker; best when detox is complete and the patient prefers a non-agonist approach.
Alcohol use disorder:
- Naltrexone (oral or monthly injection): reduces heavy drinking days and urges.
- Acamprosate: helps with protracted withdrawal symptoms and supports abstinence.
- Disulfiram: causes an adverse reaction if alcohol is consumed; works best with supervised dosing and clear external accountability.
Medication-assisted treatment plus counseling is more effective than either alone. SAMHSA’s guidance on medications for opioid use disorder and related evidence underpins this approach, and it is standard practice at Rolling Hills Recovery Center.
Integrating Co-Occurring Mental Health Treatment
Anxiety, depression, PTSD, ADHD, bipolar disorder, and personality-related traits can complicate recovery. The team screens and treats these conditions concurrently, including medication management, psychotherapy, and skills training. Treating mental health and substance use together is essential; addressing one without the other often leads to relapse.
Holistic and Recovery-Supportive Services
Mind-body practices (yoga, breathwork), nutrition coaching, sleep hygiene, and light fitness can reduce stress and improve mood. They are not substitutes for medications or therapy, but they make therapy stick. Case management helps with practical needs: FMLA paperwork, housing referrals, legal letters, school liaison, and job protections. These practical wins reduce relapse pressure.
Access, Cost, and Insurance Navigation
Finding care can feel confusing. A short, direct path helps.
Pre-Admission Steps (Quick Start)
- Call for a confidential screening. A clinician will gather medical history, substances used, last use, and withdrawal risks. If there is a seizure history or delirium tremens risk, medical detox is prioritized.
- Get medical clearance if requested. Simple labs or a physical exam may be needed to ensure safe admission, especially for detox or residential.
- Discuss level-of-care options. Based on ASAM dimensions, staff recommend the safest starting level: detox, residential, PHP, IOP, or outpatient.
- Confirm timing and logistics. Admission dates, transportation, packing list, and medication transfer. Keep it simple: ID, insurance card, current prescriptions, and a small set of clothes.
- Prepare your support. Identify at least one contact for emergencies and consent forms if the family will join therapy, and share schedules early.
For a New Jersey overview and program pathway, Rolling Hills provides details on treatment for substance abuse in NJ.
Verifying Benefits, Parity, and Coverage
- Provide insurance details to admissions. Staff can verify behavioral health benefits, deductibles, co-pays, and out-of-pocket maximums.
- Ask if your plan is in-network or if single-case agreements are available when needed.
- Discuss parity protections. Mental health and substance use treatment is protected by federal parity law, which requires comparable coverage to medical/surgical care.
- Clarify preauthorizations and utilization review. Many plans approve a certain number of days and re-review based on clinical progress. Keep documentation current; your team will help.
- Explore financial options. Sliding scale, payment plans, or state support programs may apply. Ask for all options.
Logistics: Transportation, Privacy, Consent, Cultural Responsiveness
Transportation:
- For local patients, ride share or a family drop-off works. Some programs can coordinate transportation within a reasonable radius; ask admissions.
- If coming from farther away, plan with check-in time in mind. Avoid arriving after detox medication windows.
Privacy, consent, and communication:
- Your health information is protected by HIPAA and 42 CFR Part 2. Written consent is needed to speak with employers, schools, or family unless there’s an emergency.
- Decide who can receive updates and what they can know. You can change this anytime.
Culturally responsive care:
- Share language needs, spiritual beliefs, gender identity, cultural values, and preferred family involvement. Treatment should fit the person, not the other way round.
Harm Reduction Alongside Abstinence Goals
Harm reduction and abstinence are not enemies. For many, abstinence is the long-term goal. Along the way:
- Offer naloxone to anyone with opioid use or at risk of exposure. The Centers for Disease Control and Prevention provides public guidance on overdose prevention and naloxone use.
- Provide fentanyl test strip education where legal.
- Educate on mixing risks (alcohol + benzodiazepines + opioids), tolerance changes after detox, and safer-use strategies that reduce overdose risk if return-to-use occurs.
- Maintain medication continuity; missed doses of buprenorphine or methadone increase risk; set reminders and backup pharmacy plans.
Aftercare and Relapse Prevention
Aftercare begins on day one. Discharge planning is not an exit interview; it is a living plan that changes as the patient progresses. The end point is a stable, sustainable routine with contingencies for rough days.
Discharge Planning From Day One
The treatment team collaborates with the patient to identify:
- Housing that reduces triggers.
- Work or school expectations and pacing.
- Recovery-support times that fit real life (mornings vs evenings, childcare needs).
- Medical and psychiatric follow-ups already on the calendar.
If legal or school reporting is required, consents and timelines are clarified early to avoid surprises.
Maintaining Medications and Therapy Continuity
For opioid use disorder, staying on buprenorphine, methadone, or naltrexone as long as it helps is often the safest choice. Discontinuation should be slow and planned, and it may not be the right move for a long time. For alcohol use disorder, continuing naltrexone or acamprosate while practicing behavioral skills is protective.
Therapy continuity matters:
- Keep the same therapeutic approach that worked, CBT skills, trauma work, family sessions, and set a predictable cadence (weekly or biweekly).
- Maintain contingency management if it was beneficial; tie rewards to objective behaviors.
Care coordination:
- A warm handoff to outpatient prescribers and therapists.
- Pharmacy alignment so refills are seamless.
- Clear coverage for holidays and travel; know who to call.
Peer Support and Recovery Capital
Many do well with structured peer supports, mutual-help groups, SMART Recovery, or faith-based communities, if they align with personal values. Alumni groups and sober activities build recovery capital: supportive people, places, and purposeful routines.

Return-to-Use Plan and Objective Measures
A written plan acknowledges that cravings and slips can happen. The goal is to reduce harm, shorten the episode, and return to stability quickly. Objective measures reduce guesswork and help adjust care.
Use these data points regularly:
- Craving ratings (0–10), tracked daily.
- Attendance at therapy, groups, and medication dosing.
- Urine toxicology screens (randomized schedule).
- Sleep hours, nutrition, and physical activity basics.
- Mood and anxiety scales as indicated (PHQ-9, GAD-7).
A simple rule: if objective measures worsen, higher cravings, missed appointments, positive tests, step up care. If they improve for several weeks, consider a cautious step-down with supports intact.
For the broader system perspective on where clinics fit and how they coordinate care, see this overview of the role of substance abuse clinics.
Practical Tools and Templates You Can Use Today
- 48-hour admission checklist:
- Day 1: call for screening, text or email insurance card photos, list current meds with doses and last use time; begin hydration and simple meals if safe; arrange pet or childcare.
- Day 2: confirm transportation, pack ID/insurance card/prescriptions/comfortable clothes; create a short list of emergency contacts and preferred communication; back up phone numbers on paper; plan for 1–2 weeks of basic financial needs.
- Weekly recovery schedule template: a one-page grid with columns (morning/afternoon/evening) and rows (Mon–Sun). Fill in medication times, therapy, work/school, exercise, meals, sleep target, and two “anchor” activities you enjoy. Keep it on the fridge or phone.
- Craving and trigger log: date/time, trigger, craving 0–10, skill used (urge surfing, call sponsor, 4-7-8 breathing, thought reframing), outcome, and a short note for what to try next time.
- Medication tracking sheet: name/dose/time; checkboxes for each day; refill due date; pharmacy number; backup pharmacy noted; side effects; upcoming provider visits.
- Return-to-use plan template: early warning signs list; top five people you will contact in order; steps for safety (do not use alone, naloxone location); transportation plan; where to go for step-up care; which medications or strategies have worked before.
- Urine toxicology schedule guide: agree with your provider on random windows; track completed tests; if positive, note immediate steps, call provider, increase sessions, consider medication adjustments.
- Communication boundaries worksheet for family: “What I will do,” “What I won’t do,” “What I need,” and “How I will respond to slips.” Review in family sessions and revise as needed.
- New Jersey transportation options sheet: list local ride-share apps, NJ Transit routes relevant to your location, and the program address. Add a backup plan (friend, family, or program-arranged ride when available).
Key Facts and References for Claims and Quick Decisions
- Treatment duration: NIDA’s research-based principles emphasize adequate length, around ~90 days across the continuum, which is associated with better outcomes. Short “detox-only” episodes without follow-up have a high relapse risk.
- Placement decisions: The ASAM Criteria guide multidimensional assessment (withdrawal risk, medical/psychiatric needs, readiness, environment) to match the level of care and move patients up or down as risks change.
- Evidence-based practices: SAMHSA’s evidence-based practice resources support CBT, MI, CM, family therapy, and integrated treatment for co-occurring disorders as first-line approaches in rehab settings.
- Medications and outcomes: Medications for opioid use disorder (buprenorphine, methadone, naltrexone) reduce mortality and overdose risk and improve retention. For alcohol use disorder, naltrexone and acamprosate help reduce heavy drinking and maintain abstinence; disulfiram can be useful with adherence support.
- Harm reduction: The CDC’s overdose prevention materials recommend broad access to naloxone, mixing-risk education, and recognition of lowered tolerance after periods of abstinence. These measures save lives, even when abstinence is the goal.
- Objective monitoring: Regular urine toxicology, attendance tracking, and standardized symptom scales help providers measure progress and adjust care early, which prevents crises.
- Family involvement: Structured family therapy and clear boundary-setting improve outcomes and reduce relapse-linked conflict at home; this is especially important for adolescents and young adults.
- Care coordination: Strong transitions, warm handoffs to outpatient care, medication continuity, planned step-downs, and reducing the risk window after discharge. Continuous care is safer than episodic care.
Rolling Hills Recovery Center’s approach in New Jersey follows these same principles. Care is individualized, evidence-based, and supported by holistic practices. The team works to remove barriers, insurance questions, transportation, and scheduling, so patients can focus on the work that matters most.
Conclusion
Recovery from substance use is possible. Key points: match care level to need, use therapy & meds together, and start aftercare early. Begin with an assessment, verify your benefits, and set goals.
Frequently Asked Questions (FAQs)
What is Rehab for Substance Abuse, and Who is it For?
Rehab for substance abuse is structured, medical, and behavioral care that helps a person stop harmful use, stabilize health, and build skills for long-term recovery. It’s recommended when substance use disrupts daily life, creates safety risks, or causes withdrawal.
A clinician assesses medical needs, mental health, and environment to match someone to the right level of care, detox, residential, partial hospitalization, intensive outpatient, or standard outpatient. Early help is best, but it’s never too late.
How Long Does Rehab for Substance Abuse Take, and What Should Someone Expect?
Length varies by need: detox often lasts 3–7 days, residential care may run 2–6 weeks, and outpatient care can extend for several months. Many do best with about 90 days of total engagement across levels.
Expect a full assessment, a tailored plan, therapy & medication when indicated, family involvement, relapse prevention, and steady step-down to less intensive care as stability improves.
Care is adjusted if cravings, withdrawal, or stress spike, because recovery isn’t a straight line.
What Treatments Are Used in Rehab for Substance Abuse?
Programs combine evidence-based therapies, cognitive behavioral therapy, motivational interviewing, contingency management, family therapy, and, when appropriate, FDA‑approved medications, for opioid use disorder that can include buprenorphine or methadone; for alcohol use disorder, naltrexone or acamprosate.
Medication plus counseling improves retention & reduces relapse. Trauma-informed care, sleep support, nutrition, mindfulness, and exercise round out whole-person treatment.
How Do I Start Rehab for Substance Abuse: Insurance and Admission?
Start with a confidential call for a brief screening. Bring any meds list and past records if available; if not, that’s okay. Insurance benefits can be verified quickly, and parity laws help protect access.
Admission may include same-day or next-day options depending on medical stability. To begin now, contact the admissions team at Rolling Hills Recovery Center.
They can review coverage, arrange transportation when needed, and set an intake time… without the runaround.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












