Substance abuse counseling in New Jersey helps adults move from crisis to stability with evidence-based care & compassionate support.
This overview explains what counseling involves, who it helps, and how licensed clinicians coordinate therapy, medications, and family involvement.
Readers will learn what to expect from assessment through aftercare, including safety planning & relapse prevention.
Key Takeaways
- Substance abuse counseling is most effective when it is personalized, evidence-based, and delivered by licensed clinicians; care starts with a thorough assessment and a clear plan that updates over time.
- Treatment uses proven methods like motivational interviewing and CBT, includes family support and trauma-informed care, tracks progress with simple measures, and protects privacy under HIPAA & 42 CFR Part 2.
- Medication with counseling can improve outcomes, such as buprenorphine or naltrexone for opioid use disorder; naltrexone or acamprosate for alcohol use disorder, used when clinically appropriate.
- Matching the right level of care matters: outpatient, intensive outpatient, partial hospitalization, or residential; begin aftercare planning early, with relapse prevention & safety planning from day one.
Foundations of Substance Abuse Counseling in New Jersey
What Substance Abuse Counseling is and Who it Helps
Substance abuse counseling is structured, goal‑directed therapy that helps people change their relationship with alcohol or drugs and rebuild health, relationships, and stability.
In New Jersey, licensed clinicians use evidence-based approaches to reduce harm, support recovery, and improve function, whether the person’s goal is safer use, moderation, or abstinence.
It serves adolescents, adults, older adults, and families. It also supports people using medications for opioid use disorder (MOUD) or alcohol use disorder (AUD), and those with co‑occurring mental health conditions.
Rolling Hills Recovery Center in New Jersey delivers counseling within a comprehensive program that combines proven therapies and holistic supports (for example, mindfulness and movement), across levels of care that match clinical need.
For an overview of options, see the center’s page on treatment for substance abuse in New Jersey.
Goals That Guide Care
- Stabilization: reduce withdrawal symptoms, cravings, acute risk, and medical or psychiatric instability; get a workable daily routine in place.
- Harm reduction: lower the risk of overdose, infections, legal problems, and family conflict; improve safety and quality of life even if abstinence is not the immediate goal.
- Relapse prevention: build skills, supports, and plans that make a return to heavy use less likely; respond early if slips happen.
These goals are consistent with well-supported guidance, such as the NIDA Principles of Effective Treatment, and shape how sessions are planned and paced.
Core Modalities and Why Licensure Matters
New Jersey clinicians rely on modalities backed by strong evidence:
- Motivational Interviewing (MI): a collaborative approach that strengthens the person’s own reasons and confidence to change. MI is often the early anchor because it lowers resistance and builds momentum.
- Cognitive Behavioral Therapy (CBT): identifies triggers, thoughts, and behaviors linked to use; teaches coping strategies, craving management, problem-solving, and emotion regulation.
- Contingency Management (CM): provides structured, immediate rewards for desired goals (negative drug screens, session attendance, medication adherence). CM has among the strongest effect sizes for stimulant and cannabis use disorders.
- Family systems work: includes CRAFT, multidimensional family therapy, and joint sessions that reduce blame, improve communication, and align boundaries and support.
Credentials matter in New Jersey. Substance use counseling should be provided or supervised by a Licensed Clinical Alcohol and Drug Counselor (LCADC) or by independently licensed clinicians with relevant training, such as Licensed Professional Counselors (LPC) and Licensed Clinical Social Workers (LCSW).
These licenses indicate advanced training, supervised experience, and accountability to a professional board. When medical management is indicated, care should involve prescribers experienced in addiction medicine or psychiatry.
The NIDA Principles of Effective Treatment emphasize individualized, evidence-based, and long‑enough treatment, and integration with medical and social services. Those principles guide care at Rolling Hills.

References:
- NIDA Principles of Effective Treatment: https://nida.nih.gov/sites/default/files/podat-3rdEd-508.pdf
How Counseling Works Session‑to‑Session
Intake: Biopsychosocial Assessment and ASAM-Informed Level of Care
The first visit is a structured conversation and screen. It typically includes:
- Substance use history (onset, patterns, attempts to quit, prior treatment).
- Psychiatric history, trauma exposure, and current symptoms.
- Medical history (pain, pregnancy status, infectious disease risks, withdrawal risks).
- Social determinants (housing, legal status, employment, childcare).
- Motivation and goals.
Clinicians often use brief validated tools to sharpen the clinical picture:
- ASSIST (WHO Alcohol, Smoking and Substance Involvement Screening Test) to identify risk severity across substances.
- PHQ‑9 for depressive symptoms.
- GAD‑7 for anxiety symptoms.
Data from the assessment informs ASAM Criteria placement decisions.
The ASAM Criteria consider six dimensions (intoxication/withdrawal, biomedical, emotional/behavioral/cognitive, readiness to change, relapse/continued use potential, recovery environment) to determine the safest, most effective level of care.
In practice, this may mean standard outpatient, intensive outpatient (IOP), partial hospitalization (PHP), residential, or medical detox when indicated.
References:
- ASAM Criteria overview: https://www.asam.org/asam-criteria/about
Individualized Plan and Frequency of Care
A person‑centered plan is then created. It lists specific, measurable goals, target symptoms, and services (e.g., individual CBT twice weekly, CM participation, family sessions every other week, mutual‑help engagement, and case management).
Frequency can range from weekly outpatient sessions up to nine or more hours per week in IOP, or 20+ hours in PHP. Plans flex as symptoms, risks, and goals change.
Simple planning template (use and update weekly):
- Top three goals for the next 14 days:
- Triggers I expect and my coping plan:
- Medications and refills needed:
- Family/support involvement this week:
- Appointments scheduled (therapy, medical, peer meetings):
- Barriers I foresee and backup plans:
Integrating Medications for OUD and AUD
Counseling is often more effective with FDA‑approved medications when indicated:
- OUD: buprenorphine, methadone, or extended‑release naltrexone reduces cravings and mortality. Counseling supports adherence, lifestyle stabilization, and return to valued roles.
- AUD: per the APA Clinical Practice Guideline, naltrexone (oral or extended‑release) and acamprosate are first‑line. Disulfiram may be considered for supervised patients who prefer it; topiramate and gabapentin have supportive evidence in specific cases. The prescriber and counselor coordinate, you get a unified plan with clear targets and side‑effect monitoring.
Reference:
- APA Clinical Practice Guideline for Alcohol Use Disorder: https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Clinical%20Practice%20Guidelines/Assembly/AUD-Practice-Guideline-Draft-2017.pdf
Family Involvement and Trauma‑Informed Care
Substance use affects, and is affected by, family systems. With consent, clinicians invite partners, parents, or other key supports for education, boundary setting, and communication practice.

For adolescents, family therapy is often a core component; New Jersey families can review options for substance abuse treatment for teens in NJ.
Trauma‑informed care acknowledges how adverse experiences shape current symptoms. Sessions prioritize safety, choice, collaboration, and empowerment.
If trauma symptoms are active, clinicians may add skills from Seeking Safety or introduce trauma‑focused work (after stabilization) when appropriate.
Confidentiality Under HIPAA and 42 CFR Part 2
Substance use treatment records have heightened protections.
HIPAA applies, and 42 CFR Part 2 adds additional privacy rules for programs that provide SUD diagnosis, treatment, or referral. Generally, written consent is needed to share information, with narrow exceptions for emergencies, mandated reporting, or court orders.
Clinicians explain consent options clearly. Teens have specific confidentiality rights in New Jersey; parents and guardians are engaged within those legal boundaries.
Tracking Progress: Validated Tools and Urine Toxicology
Measurement‑based care helps determine what is working. Counselors use:
- PHQ‑9 to monitor depressive symptom change.
- GAD‑7 to track anxiety.
- ASSIST to reassess substance involvement.
- Risk screens, as needed, such as the Columbia‑Suicide Severity Rating Scale (C‑SSRS).
Urine toxicology is used when clinically indicated, never as punishment. Results are discussed openly in session to adjust plans (for example, intensifying CM, revisiting triggers, or coordinating medication changes).
Rolling Hills may also use session attendance, medication adherence, craving ratings, and functional measures (work, school, sleep) to guide care. Small shifts count; the goal is steady forward movement.
Levels of Care and Coordinated Support
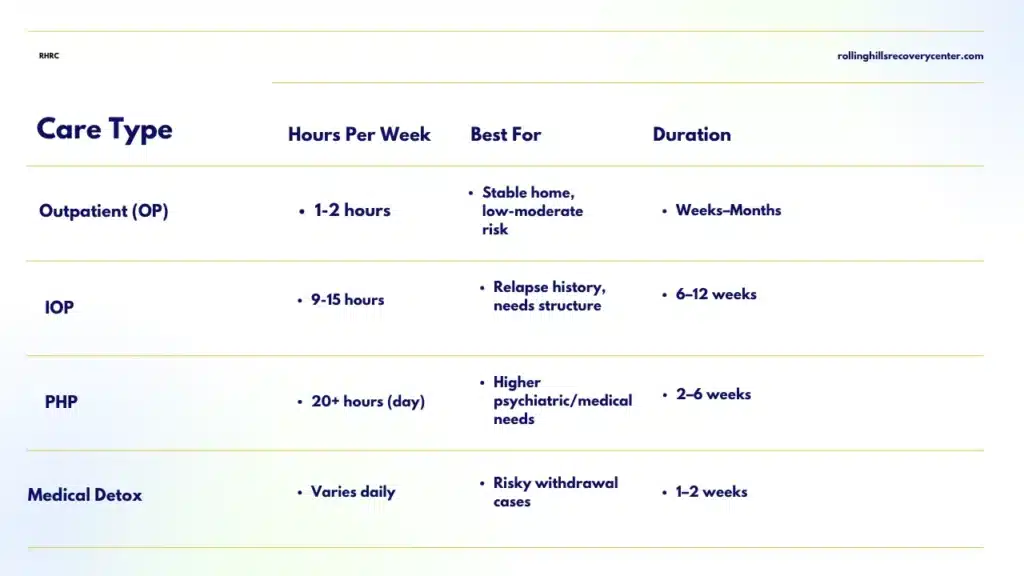
Levels of Care at a Glance
The right intensity is as important as the right therapy. Below is a simplified comparison aligned with the ASAM framework.
| Level of care | Typical intensity | Good fit when | Usual duration |
|---|---|---|---|
| Outpatient (OP) | 1–2 therapy sessions/week; medication visits as needed | Stable housing, low‑to‑moderate risk, able to practice skills between sessions | Weeks to months; step‑down or maintenance |
| Intensive Outpatient (IOP) | 9–15 hours/week group + individual | Moderate risk, repeated relapses, co‑occurring symptoms; needs structure but can live at home | 6–12 weeks on average |
| Partial Hospitalization (PHP) | 20+ hours/week, day program | Higher medical/psychiatric needs, significant functional impairment; step‑down from inpatient | 2–6 weeks on average |
| Residential/Inpatient | 24/7 structured care, medical oversight as needed | Safety concerns, severe withdrawal risk, unstable environment, or failed lower levels | Variable; often 2–6 weeks, then step‑down |
| Medical Detox | Short‑term stabilization for withdrawal | Risky alcohol, benzodiazepine, or opioid withdrawal | Days to 1–2 weeks before ongoing care |
| Telehealth adjuncts | Secure video sessions, remote monitoring, digital CBT | Transportation or childcare barriers; rural access; adjunct to OP/IOP | Ongoing as appropriate |
Rolling Hills coordinates across these levels so transitions feel seamless rather than abrupt.
Collaboration with Primary Care, Psychiatry, and Recovery Supports
Care is stronger when team‑based. Counselors (with consent) collaborate with:
- Primary care, for medical issues (liver health, cardiovascular risks, pain management, vaccinations).
- Psychiatry, for medication evaluation, especially with depression, anxiety, bipolar disorder, ADHD, or PTSD; dosing and interactions are reviewed jointly.
- Peer and community supports, such as mutual‑help meetings, SMART Recovery, recovery coaching, sober living, and vocational services.
When stimulant use, for example, methamphetamine, is involved, contingency management and intensive skills training often require closer psychiatric input for mood or sleep regulation.
For a broader picture of how clinics coordinate these services, see the center’s page on the role of substance abuse clinics.
Overdose Education and Naloxone Access
New Jersey continues to face overdose risks, especially with fentanyl. Counseling includes quick, practical training:
- Recognize overdose signs (unresponsiveness, slow or no breathing, blue lips).
- Call 911, give rescue breaths, and administer naloxone; keep it accessible. Friends and family should carry it, too.
- Avoid using alone; test doses; know Good Samaritan protections; consider fentanyl test strips where legal.
Clinicians help clients and families obtain naloxone (pharmacies, community distribution) and practice steps. This is harm reduction and lifesaving.
Safety Planning for Suicidality or High‑Risk Use
A written safety plan is routine when risk is identified. Keep it short, specific, and easy to find.
- Personal warning signs I notice first.
- Internal coping strategies I can try immediately (walking, ice water, grounding).
- People and places that help me ride out the urge.
- Professionals and crisis numbers I will call (988, local mobile crisis, clinic line).
- Steps to make my environment safer (lockboxes, limit supply, avoid using alone).
- One reason I want to stay safe today.
Clinicians revisit the plan often; if risk increases, the level of care increases, too.
Co‑Occurring Disorders: Screening and Referral
Co‑occurring mental health conditions are common. SAMHSA TIP 42 outlines integrated treatment: coordinated or unified care teams, stage‑wise interventions, and attention to both disorders over time.
At Rolling Hills, routine screens (PHQ‑9, GAD‑7, clinical interview) identify needs early.
When specialized services are needed, psychotherapy for PTSD, ADHD evaluation, or medication management, the counselor arranges referrals and co‑manages care so nothing is lost between providers.
Reference:
- SAMHSA TIP 42: https://library.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-02-01_004.pdf
Getting Started in New Jersey and Choosing Quality Care
A Step‑by‑Step Way to Begin
- Confirm insurance benefits and network status. Ask about outpatient, IOP, PHP, medication coverage, prior authorizations, and copays.
- Verify licensure. Look for LCADC, LPC, LCSW, LMFT, or physicians with addiction certification. Confirm supervision and access to prescribers when needed.
- Ask about ASAM level‑of‑care capability and referral pathways. You want a program that matches intensity to your needs and can step up or down smoothly.
- Review evidence‑based practices used (MI, CBT, CM, family therapy) and how cultural humility and trauma-informed care are built into sessions.
- Check outcomes and measurement. Programs should use validated tools (PHQ‑9, GAD‑7, ASSIST), track function, and adjust care based on data.
- Understand confidentiality policies (HIPAA and 42 CFR Part 2) and how family involvement works with written consent.
- Explore family programming and aftercare planning. Ask how relapse is handled, non‑punitively, with rapid re‑engagement.
If you’re evaluating care for an adolescent, confirm that family therapy is integrated, school coordination is available when useful, and adolescent‑specific groups are offered.
What to Expect in the First 30–90 Days
Weeks 1–2
- Intake, labs if medically indicated, medications started when appropriate (e.g., buprenorphine, naltrexone).
- Orientation to counseling, expectations, and emergency contacts. Begin motivational work and early CBT skills (urge surfing, stimulus control).
- Safety planning and overdose education with naloxone.
Weeks 3–6
- Skills training deepens: trigger mapping, coping plans, sleep, and nutrition routines. If in IOP, daily or near‑daily skills practice occurs.
- Family or supportive partner sessions begin. Boundaries and communication work reduce friction at home.
- Measurement‑based check‑ins: PHQ‑9 and GAD‑7 repeated; medication adherence reviewed; urine toxicology as clinically indicated.
- For teens, school coordination and parent coaching take form (consistent rules, rewards for progress).
Weeks 7–12
- Review goals and outcomes. Adjust intensity (step down from IOP to OP, or step up if risk rises).
- Add relapse prevention plans: high‑risk situations, personal warning signs, recovery routines, and a plan for rapid response.
- Aftercare is set up: ongoing therapy cadence, peer supports, medical follow‑ups, and contingency management targets if used.
A realistic timeline balances ambition with sustainability. Some people stabilize quickly; others need months of steady work. That’s normal. The NIDA Principles note that an adequate duration strongly predicts outcomes, and care should be adapted, not abandoned, if progress is slow.
Relapse Management and Continuing Care
Return to use is a signal to adjust the plan, not a failure. The response is practical:
- Brief analysis of what happened (where, with whom, what feelings or events came first).
- Immediate safety steps (naloxone access, supervise detox if needed).
- Rapid treatment adjustment:
- Increase session frequency or level of care.
- Consider medication changes (e.g., restart or adjust buprenorphine; consider extended‑release naltrexone for AUD if appropriate).
- Intensify CM and cue‑exposure planning.
- Strengthen supports: schedule daily check‑ins, involve a trusted person, and add structured activities.
Continuing care keeps gains. A typical maintenance plan includes:
- Ongoing therapy (weekly, then biweekly) focused on goals broader than abstinence, relationships, work/school, health, and joy.
- Periodic measurement (PHQ‑9, GAD‑7, ASSIST) and brief urine toxicology when clinically indicated.
- Regular medication visits (monthly to quarterly) and labs when required (e.g., liver function with naltrexone).
- Rehearsed relapse prevention scripts for upcoming stressors (holidays, anniversaries, job changes).
A simple weekly progress check‑in (5–10 minutes) improves accountability:
- Craving rating (0–10):
- Any use? What led up to it?
- Sleep average hours:
- Mood snapshot (best day/worst day):
- One thing I’m proud of:
- One thing I will work on this week:
- Appointments I kept; any I missed (why; what’s the fix):
Measuring Meaningful Outcomes Beyond Abstinence
Abstinence can be a goal, but it is not the only outcome that matters. Good programs, and payers increasingly, look at broader markers of health and function:
- Engagement: session attendance, timely follow‑through on referrals, and medication adherence.
- Safety: overdose reversals available, naloxone carried, fewer ED visits or legal issues.
- Mental health: changes in PHQ‑9 and GAD‑7 scores; fewer panic or depressive episodes.
- Function: school or work attendance and performance; childcare stability; reliable transportation.
- Life quality: sleep, nutrition, physical activity, social connection, and sense of purpose.
Meaningful change is improvement across several of these, sustained. The ASAM Criteria and NIDA Principles both emphasize individualized targets and enough treatment duration.
The APA AUD guideline highlights that combining counseling with first‑line medications increases the chance of achieving those broader outcomes for alcohol use disorder.
Practical Tools
A Brief Harm‑Reduction and Overdose Checklist
- Get naloxone for yourself and for family or roommates; learn how to use it. Many NJ pharmacies provide it without a prescription.
- Avoid mixing opioids with benzodiazepines or alcohol when possible; if these are prescribed, coordinate prescribers and use the lowest effective doses.
- Use with someone present or use phone‑based “never use alone” supports; start with a test dose; consider fentanyl test strips where legal.
- Keep a written safety plan and rehearse steps with a trusted person.
How Rolling Hills Recovery Center Aligns Care in New Jersey
The program integrates motivational interviewing, CBT, contingency management, and family systems therapy with medication management for OUD and AUD when indicated.
Licensed LCADCs, LPCs, LACs, and medical providers collaborate under ASAM‑informed placement decisions.
Telehealth enhances access; on‑site and community resources support continuity. Care is trauma‑informed and culturally humble.
Progress is tracked using validated tools, and urine toxicology is used when helpful, not punitively. Discharge planning starts early, with aftercare mapped out before step‑down.
For those comparing clinics, Rolling Hills encourages asking specific questions about licensure, evidence‑based practices, measurement, family programming, and aftercare.
If a prior experience felt too short or too generic, it is reasonable to expect more: a tailored plan, longer engagement when needed, and a team that adjusts quickly when life changes.
That is the point of measurement‑based, team‑based care.
Conclusion
Recovery starts with clear steps, assessment, a tailored plan, steady therapy, and family support. Key takeaways: choose licensed, evidence-based care; track progress & plan for safety. Ready to begin?
Frequently Asked Questions (FAQs)
What is Substance Abuse Counseling, and How Does it Help?
Substance abuse counseling is a structured, evidence‑based therapy that helps a person change their relationship with alcohol & drugs.
A licensed clinician assesses symptoms, sets clear goals, and uses proven methods, motivational interviewing, cognitive behavioral therapy, contingency management, and family work to reduce harm, support abstinence or safer use, and prevent relapse.
In New Jersey, substance abuse counseling also screens for co‑occurring mental health conditions, integrates medications when appropriate, and builds a practical plan for real‑life stress, sleep, work, and family.
It’s confidential and focused on steady progress, not quick fixes.
What Happens During the First Substance Abuse Counseling Session?
The first session focuses on a biopsychosocial assessment: history of alcohol and drug use, medical and mental health, family supports, and safety risks.
The clinician then recommends an ASAM‑informed level of care (standard outpatient, intensive outpatient, or higher) and drafts an initial treatment plan with short, realistic targets.
Expect a conversation about confidentiality under HIPAA and 42 CFR Part 2, informed consent, and how progress will be measured.
Simple screening tools may be used, like the PHQ‑9 for mood and the GAD‑7 for anxiety, and, if relevant, targeted urine testing. Questions are welcome; it should feel collaborative & respectful.
Does Substance Abuse Counseling Include Medications?
It can. For opioid use disorder, counseling can be paired with medication such as buprenorphine or extended‑release naltrexone.
For alcohol use disorder, options include naltrexone, acamprosate, or disulfiram when clinically appropriate.
Medication plus substance abuse counseling often improves retention and outcomes compared with either alone.
The clinician reviews benefits, side effects, and a monitoring plan; medications are combined with skills practice, craving management, and relapse‑prevention work.
If a medicine is not a fit, care continues with therapy and recovery supports; no one loses care.
How Long Does Substance Abuse Counseling Take, and How Often Are Sessions?
Frequency depends on clinical need. Many start with weekly 50‑minute sessions in outpatient care; some benefit from intensive outpatient (IOP) at 3–5 days per week for a few hours per day, then step down.
Duration varies, often 12–24 weeks for a core phase, followed by less frequent maintenance visits. Progress is reviewed regularly and the plan is adjusted; goals include fewer cravings, safer behaviors, improved mood & sleep, stronger family communication, and sustained functional gains at work or school.
Recovery is not linear, so lapses are addressed promptly without shame.
How Does Rolling Hills Recovery Center Deliver Substance Abuse Counseling in New Jersey?
Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence‑based substance abuse counseling and holistic approaches.
Their experienced team, licensed counselors, medical providers, and recovery specialists use therapies like CBT and motivational interviewing, alongside mind-body supports such as stress reduction and family engagement.
Care is individualized, trauma‑informed, and coordinated with primary care or psychiatry when needed.
They measure outcomes, plan aftercare early, and stay focused on lasting results, helping individuals overcome substance abuse and build a stable life.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts