Teen substance use affects health, learning, and safety, and early action makes a real difference. From a medical standpoint, this overview explains how to spot risk, talk with teens, and connect with evidence-based care in New Jersey.
Expect clear steps, practical tools, and compassionate strategies that respect privacy while prioritizing safety for families and schools.
Key Takeaways
- Screen early and check safety first; use simple tools like CRAFFT or S2BI, and act fast if there’s overdose risk, severe withdrawal, or self-harm concerns.
- Match care to need: start with outpatient when safe, add skills-based therapy (CBT), family therapies, contingency management; use medications for opioid use disorder when indicated; support nicotine quit with counseling and NRT.
- Family & school involvement improves outcomes; respect privacy laws (HIPAA, 42 CFR Part 2, FERPA), but share essential safety info with consent when needed.
- Recovery is ongoing, harm reduction matters: keep naloxone at home, consider fentanyl test strips where legal; focus on sleep, nutrition, positive activities, and steady aftercare with check-ins.
Overview of Substance Abuse Treatment for Adolescents
Scope and Why it Matters
Teen substance use is common and treatable. Most teenagers who experiment do not develop a substance use disorder (SUD), yet early and regular use raises the risk of addiction, injury, legal problems, and mental health crises.
New data show counterfeit pills containing fentanyl have sharply increased overdose deaths among youth.
Evidence-based care, offered in a teen-centered way and paired with family involvement, saves lives and improves long-term health, school performance, and relationships.
Teen Brain Development and Why Treatment Looks Different for Youth
- The adolescent brain is still developing, especially the prefrontal cortex, which manages planning, impulse control, and risk evaluation, through the mid-20s.
- Dopamine and stress systems are more reactive in teens, which makes substances feel more rewarding and consequences seem distant.
- Treatment needs to be skills-focused (emotion regulation, problem solving), structured, and family-inclusive, with short feedback loops and positive reinforcement.
Common Substances Used by Teens
- Alcohol: most commonly used; binge patterns drive injury and accidents.
- Cannabis: more potent products (vapes, concentrates) increase anxiety, psychosis risk in vulnerable youth, and cognitive impacts.
- Nicotine and vaping: high-nicotine pods create rapid dependence; associated with mood symptoms and sleep problems.
- Opioids: prescription pills, heroin, and counterfeit tablets laced with fentanyl; overdose risk is high even at low exposures.
- Stimulants: nonmedical use of ADHD medications, cocaine, methamphetamine; risks include cardiac events and severe anxiety/paranoia.
- Other substances: benzodiazepines (often counterfeit), hallucinogens, nitrous oxide, OTC meds misused for intoxication.
Disparities and the New Jersey Context
- Access to youth-specific services varies by county. Communities of color and LGBTQ+ youth may face higher barriers and stigma.
- New Jersey has expanded harm-reduction and naloxone availability, and most counties connect school-based referrals to community treatment.
- Transportation, insurance navigation, and language access remain practical barriers; programs should proactively address these.
Confidentiality: 42 CFR Part 2, HIPAA, FERPA, and New Jersey Minor Consent
- 42 CFR Part 2 protects substance use treatment records more strictly than typical medical records. Disclosure generally requires written consent from the patient, with limited exceptions (medical emergency, mandated reporting, court order that meets Part 2 criteria, audits/research).
- HIPAA integrates with Part 2 but is less restrictive. For minors, whether parents can access records depends on state minor-consent laws and who consented to treatment.
- FERPA covers school records. Once information is in a school’s education record, FERPA applies (not HIPAA). School-based SBIRT programs should clarify which privacy law governs each record.
Minor consent in New Jersey (confirm locally, as policies can change):
- Under New Jersey statutes (e.g., N.J.S.A. 26:2B-7 et seq. and related provisions), many adolescents, commonly age 16 and older, may consent to their own evaluation and outpatient treatment for substance use without parental permission. Programs should document the minor’s consent and capacity to consent.
- When a minor consents, they typically control disclosure to parents under 42 CFR Part 2. Clinicians should encourage family involvement, but must honor youth privacy unless there is a serious and imminent threat to life or safety, an emergency, or a mandated reporting situation.
- Payment responsibilities and parental notification vary by setting and insurer. Always review current state law and payer policy; discuss this plainly with families and teens.
Safety and Risk Today: Overdose and Fentanyl Contamination

- Counterfeit pills that look like oxycodone, Percocet, or Xanax are frequently contaminated with fentanyl and/or xylazine. One pill can be lethal.
- Key safety steps for every teen using substances or at risk:
- Carry naloxone; teach family and friends how to use it.
- Avoid using alone; use small “test” amounts; do not mix opioids with benzodiazepines or alcohol.
- Use fentanyl test strips (legal in New Jersey) for powders and pills; not a guarantee of safety, but better than guessing.
- If opioid withdrawal or heavy alcohol use is present, assess for medically supervised withdrawal risks.
- Escalate immediately if there is suicidal ideation, psychosis, severe withdrawal, or medical instability.
Early Identification and Screening
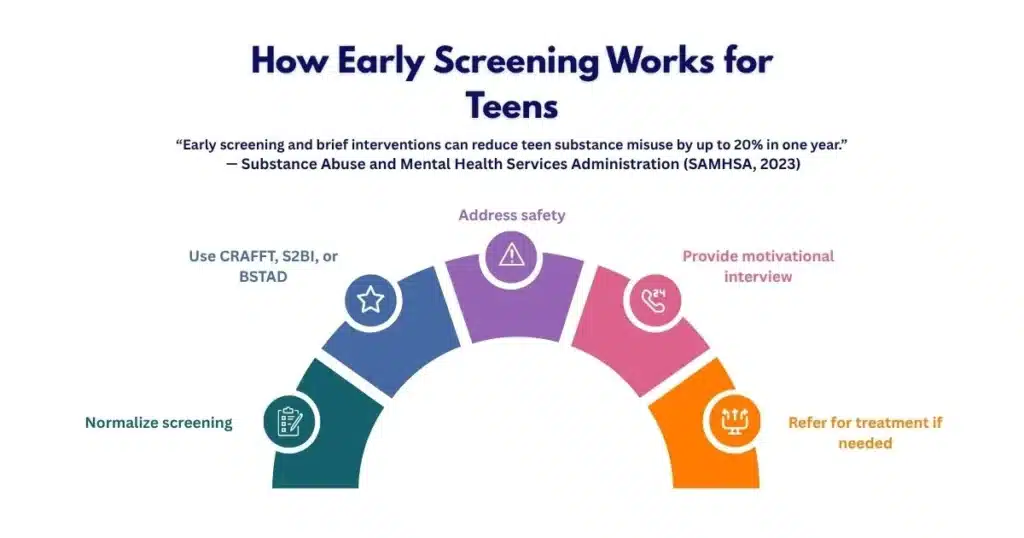
Routine Pediatric Screening with Validated Tools
Make screening a normal part of adolescent care in primary care, urgent care, school clinics, and mental health visits.
Validated tools:
- CRAFFT 2.1+N: brief, adolescent-specific; includes nicotine/vaping CRAFFT screening tool.
- S2BI: frequency-focused screening for tobacco, alcohol, and drugs.
- BSTAD: similar to S2BI, endorsed by NIDA.
How to implement (step by step):
- Normalize: “These questions are asked of everyone your age.” Offer private time without caregivers in the room.
- Use a validated tool: CRAFFT 2.1 or S2BI on paper, tablet, or patient portal.
- Score and stratify: no use, occasional use, risky use, probable SUD.
- Offer brief feedback using motivational interviewing (MI).
- Document results and plan; set a follow-up date.
- If high risk, initiate warm handoff to a teen-focused SUD clinician or program.
Brief Interventions Using Motivational Interviewing
A 5–10 minute MI conversation can reduce risky use:
- Ask permission: “Is it okay if we talk about your results?”
- Reflect and affirm: “You’ve handled a lot lately and still kept up with school.”
- Explore pros and cons: “What do you like about vaping? What’s not so great?”
- Elicit change talk: “On a scale of 0–10, how ready are you to cut down?”
- Set a small goal: “Would you try a two-week pause and see how you feel?”
- Arrange follow-up: “Let’s check in next month to see how it went.”
Risk Triage During the Same Visit
- Screen for suicidality or self-harm (e.g., Columbia Suicide Severity Rating Scale).
- Assess withdrawal risk (alcohol, benzodiazepines, opioids) and medical/psychiatric instability.
- Evaluate violence risk, trauma exposure, and unsafe home environments.
- Decide level of care: routine outpatient vs. urgent referral to IOP/PHP/residential vs. emergency care.
Ethical Toxicology Testing
- Get assent from the teen and, when applicable, consent from the legal guardian; explain what will be tested and why.
- Use targeted panels aligned with the clinical picture; include fentanyl.
- Confirm unexpected positives with definitive testing (GC/MS or LC-MS).
- Avoid punitive use of results; focus on safety and treatment planning.
- Share results with caregivers only in line with 42 CFR Part 2 and state law.
Involving Caregivers While Honoring Adolescent Confidentiality
- Ask the teen what is okay to share; use “circles of confidentiality” to set boundaries.
- Encourage caregiver participation in skills training, even if details of use remain private.
- Revisit sharing agreements regularly; crises or safety risks may warrant broader disclosure consistent with law and ethics.
Evidence-Based Treatment
Match the Level of Care to Severity and Risk
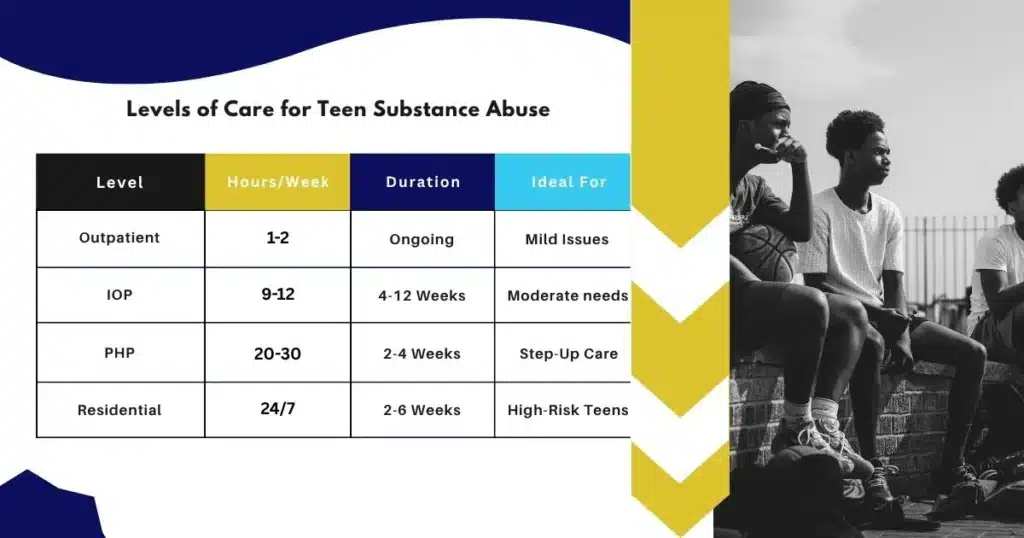
Consider function (school, family, safety), co-occurring conditions, withdrawal needs, and motivation.
A quick comparison of levels of care:
| Level of care | When it fits | Typical components | Teen-specific notes |
|---|---|---|---|
| Outpatient (1–2x/week) | Mild–moderate use, stable housing, school attendance | CBT, family sessions, MI, drug testing as agreed | Works well when family engages; add peer supports |
| Intensive Outpatient (IOP) | Moderate–severe use, failed outpatient alone | 9–12 hrs/wk group + individual + family, skills training | Evening hours help school continuity |
| Partial Hospitalization (PHP) | Severe symptoms, high relapse risk, but medically stable | 20–30 hrs/wk, daily structure, psychiatric care | Short-term stabilization; bridge to IOP/outpatient |
| Residential/Inpatient | Safety instability, repeated overdose, failed lower levels | 24/7 milieu, medical/psychiatric care | Use when clearly indicated; plan step-down early |
For teens with opioid use disorder, specialized care is often needed. Programs with experience in youth medications and family work achieve better outcomes. For New Jersey-focused help, see local opioid care options such as this overview of rehab for opioid use disorder.
Co-Occurring Mental Health Assessment
- Evaluate for depression, anxiety, PTSD/trauma, ADHD, bipolar spectrum, psychosis, eating disorders, and self-harm.
- Use standardized measures (e.g., PHQ-A, GAD-7, PSC-17, PTSD-RI).
- Coordinate care so one team leads an integrated plan. For integrated treatment of mental health and substance use together in New Jersey, review our article on dual diagnosis treatment.

Core Treatment Modalities
- Cognitive Behavioral Therapy (CBT): identifies triggers, thinking traps, and coping skills; includes functional analysis and relapse prevention.
- Family-based therapies:
- Multidimensional Family Therapy (MDFT): targets family communication, school engagement, and peer context.
- Functional Family Therapy (FFT): builds motivation, reduces conflict, and strengthens parenting practices.
- Contingency Management (CM): provides immediate, meaningful rewards for target behaviors (e.g., negative tests, session attendance).
- Dialectical Behavior Therapy (DBT) skills: emotion regulation, distress tolerance, interpersonal effectiveness for teens with self-harm or intense emotions.
- Trauma-focused care: TF-CBT or EMDR when trauma symptoms are present; sequence carefully with stabilization and safety.
- Holistic supports: sleep regulation, exercise, mindfulness, nutrition, and creative activities can improve mood and resilience when paired with evidence-based therapy.
Medications: When and How for Adolescents
Opioid use disorder (OUD):
- Buprenorphine/naloxone: generally appropriate for adolescents aged 16 and older under qualified prescribers; consider home induction with close follow-up; involve caregivers when possible.
- Methadone: available only through certified Opioid Treatment Programs; minors require specific federal OTP criteria and guardian consent per program policy.
- Extended-release naltrexone: typically used at age 18 and older; requires full detox before initiation.
Stimulant and cannabis use disorders:
- No FDA-approved medications for teen stimulant or cannabis use disorders; focus on CBT, CM, MDFT/FFT. Treat co-occurring ADHD appropriately with careful monitoring.
Alcohol use disorder:
- Psychosocial approaches are first-line. In select older adolescents, medications like naltrexone or acamprosate may be considered off-label by experienced clinicians, with informed consent.
Nicotine and vaping:
- Behavioral counseling is first-line (quit plan, triggers, texting programs).
- Nicotine replacement therapy (patch, gum, lozenge) can be considered with clinician oversight; FDA labeling for NRT under age 18 is limited, use shared decision-making, and careful monitoring.
- Digital supports: quitlines, text-to-quit programs, and app-based coaching.
Safety and monitoring with medications:
- Obtain consent/assent aligned with NJ law and Part 2/HIPAA rules.
- Start low, go slow; schedule weekly to biweekly check-ins early on.
- Coordinate with schools to support dosing schedules discreetly if needed.
Careful Monitoring and Culturally Responsive Care
- Collaborative care plan with the teen’s goals centered.
- Measurement-based care: track attendance, cravings, mood, sleep, and school functioning.
- Respect culture, language, and family values; offer interpreters and culturally matched peer supports when possible.
- Minimize barriers: transportation help, evening sessions, telehealth options, and flexible family scheduling.
Family, School, and Community Engagement
Caregiver Psychoeducation and Skills Training
Educate caregivers in short, repeated bursts:
- Substance basics: effects, overdose signs, withdrawal, and the realities of fentanyl in counterfeit pills.
- Communication skills: calm tone, reflective listening, clear expectations.
- Contingency management at home: consistent rewards and fair limits.
- Boundaries and safety: lock boxes for meds, safe storage of firearms and alcohol, and monitoring social media without surveillance tactics.
- Family routines: meals together, sleep hygiene, exercise, tech limits.
Simple caregiver action plan (template):
- What we will do this week: 1) Eat together 3 nights; 2) Curfew at 10pm Fri/Sat; 3) Reward: extra car time if plan followed.
- What we will say when conflict arises: “Let’s pause and try again in 10 minutes.”
- Who we call if safety changes: therapist, crisis line, 911 if imminent risk.
School Coordination: SBIRT, 504/IEP Supports
- With teen consent, collaborate with school counselors and nurses.
- SBIRT in schools can identify risk early and link to care.
- Academic accommodations:
- 504 Plan for attendance flexibility, test timing, and quiet spaces.
- IEP when learning differences or mental health conditions affect education.
- Re-entry after treatment: plan for missed work, reduced load initially, and a trusted staff contact.
Peer Recovery, Positive Activities, Sleep, and Nutrition
- Encourage pro-recovery peers and mentoring groups; community service or clubs help replace high-risk time.
- Prioritize sleep (8–10 hours), regular meals, hydration, and daily movement; these improve mood and cut cravings.
- Provide options beyond saying “no”: structured hobbies, part-time jobs, faith communities, or arts.
Harm Reduction at Home
- Naloxone: keep at home and in backpacks; train every adult and teen in the household.
- Fentanyl test strips: legal in New Jersey; teach correct use and interpretation with caution about false negatives.
- Safe-use education: never use alone, avoid mixing depressants, test a small amount first, call 911 for any breathing problems.
- Secure storage: lock up medications, alcohol, and cannabis products.
Aftercare and Relapse Prevention

Continuing Care Planning Starts on Day One
- Set a 6–12 month continuing-care arc even if initial treatment is brief.
- Establish recovery routines:
- Weekly therapy or check-ins that taper with progress.
- Peer support groups suitable for teens.
- Daily structure: school, study, physical activity, and a wind-down routine at night.
Step-by-step discharge-to-aftercare handoff:
- Identify a continuing-care clinician before discharge.
- Schedule the first two appointments in advance.
- Create a transportation plan and a primary contact person.
- Share a concise treatment summary (with youth consent).
- Confirm how to refill medications and who to call for side effects.
- Book a follow-up with the primary care clinician.
Harm Reduction and Periodic Check-Ins
- Normalize ups and downs; slips are data, not failure.
- Incorporate skills refreshers: urge surfing, alternative coping plans, crisis scripts.
- Encourage periodic check-ins even after sustained improvement (monthly or quarterly).
Urine Drug Testing with Consent
- Use collaborative, scheduled, or random testing with clear purpose.
- Share results as agreed; emphasize safety, not punishment.
- Limit panels to likely exposures and confirm positives definitively.
Crisis Planning and Transitions to Young Adult Services
- Crisis plan elements:
- Early warning signs unique to the teen.
- What the teen wants others to do (and not do) during a crisis.
- Phone numbers for prescriber, therapist, caregivers, and 24/7 resources.
- Transition planning around ages 17–19:
- Review consent laws as the teen becomes a legal adult.
- Hand off to adult providers who are youth-friendly.
- Support education or vocational goals and independent living skills.
Metrics to Track Outcomes
- Abstinence or reduced use days (self-report + tests).
- School attendance and grades.
- Functioning at home and with peers.
- Depression/anxiety/PTSD symptom scales.
- Crisis events: ER visits, overdoses, self-harm.
- Engagement: session attendance, medication adherence.
Programs should share outcomes transparently and use them to improve care. For families still deciding if a higher level of support is needed, reviewing topics like the most addictive substances can help frame risk discussions thoughtfully; this educational piece may be helpful: Top 10 most addictive drugs in the world.
Helpful Tools and Resources For Clinicians and Families
Clinical tools and workflows:
- Screening workflow (adapt for your setting):
- Private time with adolescent
- CRAFFT 2.1+N or S2BI completion
- MI-based feedback
- Risk triage (suicide, withdrawal, psychosis)
- Family involvement, planning, and safety steps
- Document and schedule follow-up
- Urgent safety checklist:
- Naloxone training and kit today
- Fentanyl test strips access and education
- Medication safety: lock box; reconcile meds at home
- Remove or secure firearms and substances
- Crisis contacts in phone; location sharing during acute risk
- Family session template:
- Set shared goals
- Communication skill practice
- Home CM plan with small, consistent rewards
- Review school plan and attendance
- Plan for the next week’s obstacles
External resources:
- NIDA adolescent resources for parents and educators: NIDA adolescent resources
- American Academy of Pediatrics substance use prevention and care: AAP substance use and prevention
- SAMHSA Evidence-Based Practices Resource Center: SAMHSA Evidence-Based Practices Resource Center
- CDC Youth Risk Behavior data and trends: CDC Youth Risk Behavior data
- CRAFFT validated adolescent screening tool and materials: CRAFFT screening tool
How to get started this week:
- If you are a clinician:
- Add CRAFFT 2.1 to your adolescent intake packet.
- Build a 10-minute MI script and a one-page safety handout with naloxone info.
- Identify a teen-capable prescriber for buprenorphine and a referral path for IOP/PHP.
- Clarify with your compliance team how 42 CFR Part 2 and NJ minor-consent laws determine information sharing in your setting.
- If you are a caregiver:
- Ask your teen’s clinician to screen for substance use privately.
- Bring naloxone home; learn how to use it and store it visibly.
- Start a small, specific home CM plan (e.g., rewards for keeping curfew and attending sessions).
- Connect with school counselors to discuss 504/IEP options respectfully and privately.
Families can speak with a clinician to discuss options, from outpatient therapy to more structured services, and how to weave in ongoing school and family routines.
Conclusion
Early, honest screening, safety planning, and family & school support make teen care work. Protect privacy; use proven therapies and meds; keep naloxone handy. Small steps add up; recovery takes time.
Frequently Asked Questions (FAQs)
What is Substance Abuse Treatment for Teens, and How to Get Help in NJ?
health at home, in school, and socially. Care usually includes a full assessment, a safety plan, therapy that fits the teen’s needs, and family involvement.
How to get help now:
• Start with a calm talk; ask what they’re using, how often, and any safety risks.
• Arrange a confidential assessment with a qualified clinician. A pediatrician or licensed counselor can start screening quickly.
• If there’s danger (overdose signs, severe withdrawal, suicidal thoughts), seek emergency care right away.
• Ask about evidence-based therapies used in substance abuse treatment, like cognitive behavioral therapy, family-based therapy, contingency management, and skills training.
• For opioid use, ask about medications for opioid use disorder when appropriate, plus a naloxone rescue kit at home.
Rolling Hills Recovery Center in New Jersey can coordinate a compassionate, confidential next step so families don’t have to navigate this alone.
What Signs Suggest a Teen May Need Substance Abuse Treatment?
Look for a cluster of changes over weeks, not just one rough day:
• Sudden drop in grades or skipping school
• Mood swings, irritability, or anxiety that won’t let up
• New friend group, secrecy, staying out late
• Smell of alcohol or cannabis; vaping gear, pill fragments, missing cash
• Sleep problems, appetite changes, or unexplained injuries
• Risky use: binge drinking, mixing pills, driving after using
If several of these show up, it’s time to ask about substance use and consider treatment. A quick screening and a respectful conversation can prevent bigger problems.
What Happens First During Treatment for Teenagers?
The first phase focuses on clarity and safety:
• Intake and assessment: substance use history, mental health, medical review, school status, and family supports
• Safety planning: overdose risk, self-harm screening, cravings, and triggers
• Medical stabilization: manage withdrawal if needed, address sleep, nutrition, and any acute issues
• Match level of care: outpatient, intensive outpatient (IOP), partial hospitalization (PHP), or residential, only when clearly indicated
• Start therapy: skills-based CBT, family therapy, contingency management; trauma-informed care when needed
• Caregiver involvement: set communication rules, roles, and simple home routines that support recovery
This is how treatment builds momentum early: practical steps, clear goals, and frequent check-ins.
Is Addiction Treatment for Teenagers Confidential in New Jersey?
In general, health information is protected by privacy laws (including HIPAA) and special rules for substance use records (often called 42 CFR Part 2). Programs explain what can be shared, with whom, and why, before treatment starts.
For teenagers, consent and parental involvement can depend on state law, the setting, and clinical safety needs. Most programs encourage caregiver participation because it helps outcomes, yet still protect sensitive details. Teens should know:
• What stays private vs. what must be shared for safety
• How consent for drug testing works
• That treatment aims to build trust and reduce harm, not punish
When in doubt, ask the care team to walk through confidentiality in plain language, no surprises.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












