Fentanyl withdrawal can be intense, unpredictable, and longer than with other opioids. This overview explains what to expect, when supervised detox is safer, and how evidence-based medications and supports reduce risks and cravings. It also outlines practical steps New Jersey adults and families can take to prepare, stay safe, and move quickly into ongoing recovery.
Key Takeaways
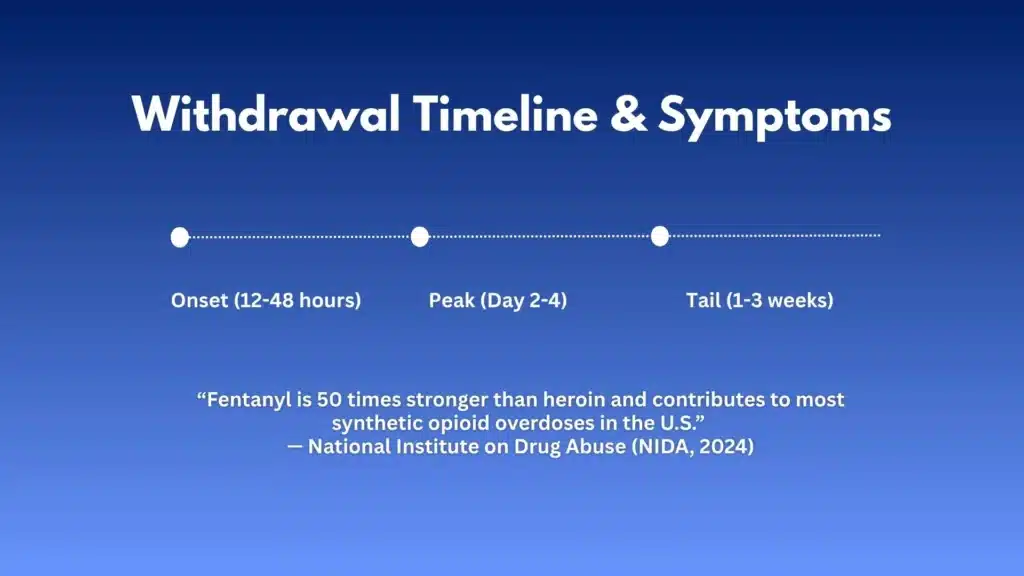
- Fentanyl withdrawal often starts 12–48 hours after the last use, peaks around days 2–4, and some symptoms like poor sleep and cravings can linger for a couple of weeks; its high potency and fat storage make symptoms spikier.
- Supervised detox is safer when pregnant, using benzos or xylazine, or with medical and mental health concerns; clinicians track severity with COWS and monitor vitals closely.
- Medications work: buprenorphine (standard start or micro‑induction) & methadone lower cravings and make symptoms manageable; comfort meds, fluids, and electrolytes support recovery.
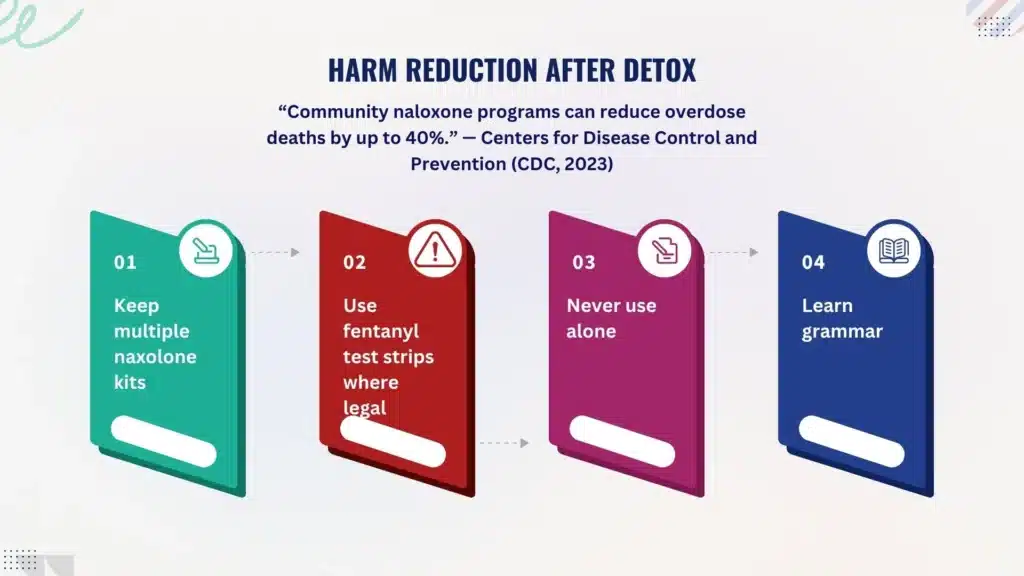
- Overdose risk climbs after detox because tolerance drops; keep naloxone on hand, avoid using alone, consider fentanyl test strips where legal, and move quickly into MOUD, therapy, and nutrition care.
Detox for Fentanyl: Scope and Urgency
Fentanyl is an extremely potent synthetic opioid. Micrograms can move a person from euphoria to respiratory arrest.
Because fentanyl is highly lipophilic (it dissolves into body fat), it redistributes slowly and can “leak” back into the bloodstream over time.
That property, plus its analogs, helps explain why withdrawal can feel longer, spikier, and less predictable than heroin withdrawal. People may cycle through waves of discomfort even after several “clean” days.
Rolling Hills Recovery Center treats fentanyl use disorder with the same seriousness as other high-risk opioids, while adapting care for the unique challenges fentanyl brings.
A recent check of the literature turned up no new clinical standards that supersede established best practices, so the approach below leans on major guidelines from ASAM, SAMHSA, NIDA, and CDC.
Clinicians here combine those standards with practical, step-by-step care and monitoring.
Red flags that warrant supervised medical detox and not a do-it-yourself attempt:
- Pregnancy (any trimester), postpartum, or breastfeeding
- Polysubstance use, especially benzodiazepines, alcohol, or xylazine (tranquilizer)
- Severe dehydration, persistent vomiting/diarrhea, or inability to keep fluids down
- Chest pain, uncontrolled hypertension, fever, or confusion
- Suicidal thoughts, recent overdose, or no safe place to stay
People who smoke fentanyl frequently, or rotate between smoking and injecting, often report more erratic withdrawals. Fentanyl patches and long-acting analogs also delay and blur timing.
Withdrawal Timeline and Symptoms
What to Expect: Onset, Peak, and Tail
- Onset: 12–48 hours after last use, but patches, repeated high-dose exposure, or co-use with methadone can delay onset. Heavy daily smoking may trigger earlier symptoms, yet still create late waves due to redistribution.
- Peak: Day 2–4 for most, with autonomic symptoms (sweating, piloerection, lacrimation), GI upset, aches, restlessness, and severe cravings.
- Tail: Anxiety, low mood, poor sleep, fatigue, and intermittent cravings can last weeks. Sleep disruption can persist even with stabilized medication.
Core symptoms include rhinorrhea, yawning, gooseflesh, dilated pupils, abdominal cramping, nausea/vomiting, diarrhea, chills, bone/muscle pain, anxiety, irritability, and insomnia.
Some patients report hot–cold flushing cycles that feel “spiky” compared with heroin.
COWS Scoring and Clinical Triage
Clinicians use the Clinical Opiate Withdrawal Scale (COWS) to quantify severity. It scores 11 signs/symptoms (resting pulse, sweating, restlessness, pupil size, aches, runny nose/tearing, GI distress, tremor, yawning, anxiety/irritability, gooseflesh). Broadly:
- Mild: 5–12
- Moderate: 13–24
- Moderately severe: 25–36
- Severe: >36
COWS helps time buprenorphine or other interventions—especially when fentanyl’s lipophilicity makes onset less obvious.
Spontaneous vs Precipitated Withdrawal
- Spontaneous withdrawal: Occurs naturally as opioids wear off; timing varies with fentanyl.
- Precipitated withdrawal: Triggered if a partial agonist like buprenorphine displaces a high-potency, full agonist (like fentanyl) too early. Symptoms surge quickly: chills, cramping, diarrhea, anxiety, and hypertension. It’s not dangerous for most, but is intensely uncomfortable and can derail treatment if not anticipated and managed.
To reduce risk, Rolling Hills Recovery Center uses careful COWS-based timing or microdosing (Bernese method) strategies and close monitoring.
Risks to Watch For
Vomiting and diarrhea can cause dehydration, low potassium, and fainting. Autonomic instability may push heart rate and blood pressure higher than baseline. Strong cravings raise relapse risk. Re-exposure after even a short detox drops tolerance fast; this is when overdose risk spikes sharply.
Medical Detox Approaches
Choosing Inpatient vs Closely Monitored Outpatient
Inpatient or residential medical detox is preferred when any of the following apply: red flags above, severe COWS scores, limited support at home, pregnancy, or recent overdose.
Patients with stable housing, moderate symptoms, and strong support may do well in closely monitored outpatient care if they have rapid access to MOUD and daily check-ins.
Buprenorphine Induction: Standard vs Microdosing
Buprenorphine is a first-line medication for opioid use disorder. It reduces cravings and withdrawal, lowers overdose risk, and supports long-term retention in care.
Fentanyl’s pharmacology makes induction trickier, so clinicians individualize the method.
Standard induction (typical when COWS ≥8–12)
- Confirm last use time, route, and any benzodiazepine or alcohol co-use.
- Wait until at least mild-moderate withdrawal (COWS 8–12+). For fentanyl, waiting until clear signs may reduce precipitated withdrawal risk.
- Start with a test dose (e.g., 2 mg). Reassess in 45–60 minutes. Titrate in 2–8 mg increments as needed, watching for relief of symptoms.
- Typical day 1 total ranges widely; fentanyl-exposed patients sometimes need higher day-1 dosing than those on heroin. Careful observation is essential.
- Day 2 onward: Adjust to control cravings and symptoms; many stabilize between 8–24 mg/day, but the dose is tailored to the patient.
Microdosing (Bernese method) to reduce precipitated withdrawal risk. This method introduces very small amounts of buprenorphine while the patient continues low, tapering amounts of full-agonist opioids. Over several days, buprenorphine slowly displaces fentanyl.
Example framework (for illustration; the clinician adjusts timing and doses):
- Day 1: 0.5 mg buprenorphine once or twice daily
- Day 2: 1 mg total split doses
- Day 3: 2 mg total
- Day 4: 4 mg total
- Day 5: 6–8 mg total; begin reducing full-agonist use
- Day 6–7: 8–12+ mg total; discontinue full-agonist opioids
Benefits: Lower risk of precipitated withdrawal and gentler symptom curve. Requirements: precise dosing, frequent check-ins, and clear instructions.
Managing precipitated withdrawal if it occurs
- Do not stop buprenorphine abruptly; dose up carefully under medical guidance to occupy receptors and settle symptoms.
- Add adjunctive medications (below) and hydration.
- Provide reassurance, precipitated withdrawal usually improves within hours as buprenorphine occupancy increases.
Methadone as a Stabilization Option
Methadone is a full opioid agonist with strong evidence for retention and overdose reduction. It is particularly helpful for patients who have not done well with buprenorphine or when severe fentanyl exposure makes induction difficult.
Key points:
- Must be dispensed by a certified opioid treatment program (OTP).
- Start low, go slow, especially with benzodiazepines, alcohol, or other sedatives on board.
- Daily supervised dosing early on; ECGs may be used in those with cardiac risk, prolonged QT history, or interacting medications.
- Effective for pregnancy, methadone and buprenorphine are both considered first-line MOUD in pregnancy.
Rolling Hills coordinates OTP access when methadone is the right fit, ensuring warm handoffs and transportation support if needed.
Adjunct Medications and Supportive Care
Adjuncts can reduce symptoms during induction and early stabilization:
- Clonidine or lofexidine for sweating, restlessness, and autonomic symptoms; monitor blood pressure.
- NSAIDs or acetaminophen for aches and cramping.
- Antiemetics (e.g., ondansetron) for nausea/vomiting.
- Loperamide is labeled for diarrhea; avoid misuse or high-dose use.
- Hydroxyzine for anxiety and sleep; avoid benzodiazepines unless clearly indicated and supervised.
- Sleep hygiene and, when appropriate, short-term non-benzodiazepine sleep aids.
Hydration and electrolytes. Fentanyl withdrawal can dehydrate patients quickly. Oral rehydration solutions, broths, and electrolyte packets help.
Check vitals, orthostatic blood pressure, and signs of dehydration (dry mouth, low urine output). Intravenous fluids are used when oral intake isn’t enough.
Pregnancy-safe protocols
- MOUD (methadone or buprenorphine) is recommended during pregnancy; medically supervised withdrawal is not preferred due to high relapse and overdose risk.
- Avoid medications with fetal risk; coordinate with obstetrics. Monitor fetal movement in later trimesters. Plan for neonatal opioid withdrawal management post-delivery with pediatric partners.
Monitoring vital signs includes nursing checks of heart rate, blood pressure, temperature, respiratory rate, and oxygen saturation. Some patients benefit from brief telemetry or more frequent checks during severe waves.
Comparing MOUD Options in Fentanyl Detox and Beyond
| Feature | Buprenorphine | Methadone | Extended-release naltrexone |
|---|---|---|---|
| Mechanism | Partial agonist | Full agonist | Antagonist |
| Typical start | When in withdrawal (or microdosed) | OTP-based start | Only after full detox (7–10+ days opioid-free) |
| Overdose protection | Strong | Strong | Blocks opioids, but no agonist effect |
| Good for | Most patients, flexible settings | Those needing daily structure or who didn’t do well on buprenorphine | Highly motivated, stable patients post-detox |
| Special notes | Risk of precipitated withdrawal with fentanyl if started too early | QT monitoring in select patients; OTP access required | Hard to start after fentanyl due to protracted withdrawal |
Clinicians at Rolling Hills help patients choose based on history, goals, co-occurring conditions, and access.
Safety and Harm Reduction
Naloxone and Immediate Safety Steps
Everyone leaving drug or alcohol detox should have naloxone and know how to use it. Family and friends should be trained as well. Multiple kits are better than one.
The risk of a fentanyl overdose goes up after detox as tolerance drops quickly; a return to previous doses can be lethal.
Never use alone strategies:
- If someone has not committed to MOUD yet, encourage them never to use it alone. If legal in your area, use hotlines/apps designed for this purpose.
- Start with a small test dose. Have naloxone visible and reachable. Avoid mixing with alcohol or benzodiazepines.
Fentanyl test strips. Where legal, test strips can detect fentanyl in powders or pills, even in non-opioids. They are an additional layer of risk reduction, but not a guarantee.
Xylazine awareness: Xylazine is a non-opioid tranquilizer often mixed with fentanyl. It causes deep sedation, slow healing wounds, and may blunt the response to naloxone. In suspected xylazine exposure:
- Still give naloxone for the opioid component.
- Provide rescue breathing.
- Seek medical care for sedation and any skin injuries or ulcers.
CDC overdose prevention resources and local harm reduction services can help with supplies, education, and naloxone access.
Rolling Hills incorporates harm reduction education into every detox discharge plan because it saves lives, plain and simple.
Transition and Relapse Prevention
Moving from Detox to Ongoing Medications for OUD
Detox is the first step, not the destination. The strongest evidence for preventing relapse and overdose is ongoing MOUD.
- Buprenorphine: Continue daily dosing; some transition to long-acting injectable formulations once stable.
- Methadone: Maintain at the OTP with counseling and medical monitoring.
- Extended-release naltrexone: Requires full detox first; for some, this is practical after a structured inpatient course. Not ideal if cravings remain high or access to urgent care is limited.
Rolling Hills Recovery Center prioritizes same-day or next-day transitions from medical detox to MOUD-based treatment for fentanyl addiction to keep momentum and reduce risk.
Therapy, Skills, and Recovery Planning
Medication addresses physiology; behavior and environment require a plan.
- Cognitive behavioral therapy: Identify automatic thoughts and patterns that lead to use; rehearse new responses.
- Contingency management: Small rewards for meeting targets like negative screens or session attendance are effective and practical.
- Trauma-informed care: Many patients have trauma exposure; addressing it reduces triggers.
- Family support: Education and boundaries help everyone.
Triggers, Sleep, and Nutrition
Relapse risk is high when sleep, stress, and nutrition are off. A simple plan helps:
- Identify three top triggers (places, people, feelings).
- Build a 7-day routine: wake/sleep times, meals, movement, therapy, and recovery time.
- Keep quick, high-protein snacks on hand (string cheese, yogurt, nuts).
- Limit caffeine late afternoon; consider a wind-down routine: dim lights, shower, reading.
Insurance Verification and New Jersey Access Steps
Rolling Hills Recovery Center can verify insurance benefits quickly, coordinate transportation, and set up same-week admission for medical detox or MOUD initiation.
For people searching for medical detox in New Jersey, starting with a direct benefits check, a short clinical assessment, and scheduling an admission date reduces waiting and anxiety.
Individuals and families can explore options for treatment for substance abuse in NJ or request a referral for a medical detox near you.
The team maintains collaborations with OTPs, obstetrics, primary care, and wound care for xylazine-related injuries.
Practical Tools, Templates, and Step-by-Step Instructions
24-Hour Prep Checklist Before Admission or Induction
- Pack basics: photo ID, insurance card, current medication list, comfortable clothes, and a phone charger.
- Hydration plan: electrolyte packets, a reusable water bottle, and light snacks if permitted.
- Contact list: family/support numbers, pharmacy, primary care, and OTP (if applicable).
- Safety items: naloxone kit, medical alerts, and a list of allergies.
If starting outpatient buprenorphine, arrange a calm space, limit obligations for 48–72 hours, and have a plan for supportive check-ins.
Step-by-Step: Standard Buprenorphine Induction at Home with Telehealth Support
This is a general overview; the exact plan should be given by a licensed prescriber. For many fentanyl-exposed patients, a clinic-based start is safer, but when home induction is appropriate:
- Confirm the last fentanyl use and avoid additional opioid use. Avoid alcohol and benzodiazepines.
- Begin when COWS is at least mild to moderate (restlessness, yawning, dilated pupils, GI upset). This might take longer than expected with fentanyl.
- Take the first dose exactly as prescribed (often 2 mg). Set a timer for 45–60 minutes.
- Reassess: if symptoms persist and COWS remains elevated, take the next prescribed increment. Keep a simple log of time, dose, and symptoms.
- Stop titration for the day once symptoms are controlled (or at the maximum day-1 dose given by your prescriber). Communicate with your clinician.
- Day 2 and beyond: Take the total amount that controlled day-1 symptoms as a single morning dose or split dosing as directed. Discuss any cravings or sedation right away.
If precipitated withdrawal occurs, contact the prescriber immediately. Do not abandon the plan; timely additional doses and supportive meds usually resolve symptoms.
Step-by-Step: Microdosing (Bernese Approach) with Clinical Oversight
- The prescriber provides exact microdoses and a taper schedule for any remaining full-agonist opioid.
- Obtain a pill cutter or prescribe micro-tablets/films to allow accurate tiny doses.
- Day by day, add small buprenorphine doses while maintaining or gently tapering the full agonist.
- Increase buprenorphine and reduce the full agonist per plan until the full agonist is stopped.
- Monitor vitals, hydration, sleep, and cravings; adjust pace if symptoms rise.
This approach can be more comfortable with fentanyl and high-risk co-use patterns but requires tight coordination.
Hydration and Nutrition Template for the First Week
- Fluids: 2–3 liters/day if allowed medically; include oral rehydration solution if vomiting or diarrhea occurs.
- Meals: small, frequent, bland foods; add protein shakes if appetite is low.
- Electrolytes: potassium-rich foods (bananas, potatoes) unless restricted.
- Sleep: aim for consistent times; brief naps are okay early on, but avoid long daytime sleep if possible.
Putting it Together in New Jersey
A 7–10 day detox-to-stabilization flow might look like this:
- Days 1–2: Admission, vitals, labs as needed, hydration, COWS monitoring, start buprenorphine (standard or microdosing) or methadone coordination, adjunct meds for symptoms.
- Days 3–5: Dose optimization, counseling, family touchpoints, harm reduction education (naloxone, test strips, never use alone practices).
- Days 6–7: Finalize MOUD dosing, develop a recovery schedule, sleep plan, and nutrition plan; confirm aftercare appointments; introduce CBT and contingency strategies.
- Days 8–10: Transition to outpatient MOUD, IOP, or residential step-down; confirm transportation and prescriptions.
Safety Net After Discharge
Harm Reduction Steps to Keep in Place
- Keep multiple naloxone kits. Teach family and friends how to use them.
- Test anything that might be used with legal local fentanyl test strips.
- Avoid mixing with sedatives or alcohol.
- Have a check-in buddy daily for the first two weeks.
- If a slip happens, call fast, MOUD dose adjustments, and prompt support can prevent a spiral.
Early Warning Signs and What To Do
- Rising cravings, new insomnia, skipping meals, or isolating from supportive people.
- Contact the care team for a same-day check-in. Consider a dose increase, an added therapy visit, or contingency management reinforcement.
- If there’s a lapse, safety first: use smaller amounts, do not use alone, have naloxone nearby, and return to treatment immediately.
Rolling Hills Recovery Center works with patients and families to put a simple, written plan on the fridge, who to call, what to do, and where to go, so there is no guesswork in a crisis.
How Rolling Hills Recovery Center Supports Families

- Education: what MOUD is and is not; how to support without enabling.
- Family sessions: align expectations, set boundaries, and create accountability.
- Coordination: primary care, OB, mental health, and OTPs when methadone is chosen.
- Insurance navigation: same-day benefits checks, prior authorizations, and scheduling.
Frequently Asked Clinical Questions
How Long Does Fentanyl Withdrawal Last?
Acute symptoms often peak by days 2–4 but may arrive late and come in waves. Sleep, mood, and energy can lag for weeks, which is why pairing detox with MOUD and sleep/nutrition support makes a big difference.
Can Buprenorphine Be Started if I Used Fentanyl Yesterday?
Maybe, but it depends on the signs of withdrawal and the approach. Starting too early can precipitate withdrawal. Microdosing strategies allow earlier starts with less risk, but they require careful dosing and close contact with a prescriber.
Is Methadone Better for Fentanyl?
Neither medication is “better” for everyone. Methadone can be more forgiving for very heavy fentanyl exposure or when people struggle with buprenorphine. Buprenorphine is flexible and widely available in office-based settings. The right choice is individual.
Can I Take Clonidine on My Own?
Clonidine lowers blood pressure and heart rate, so it should be used with medical guidance. The team will monitor vitals and adjust doses to symptom control while avoiding hypotension.
References and Further Reading
National Institute on Drug Abuse (NIDA) on fentanyl: https://nida.nih.gov/research-topics/fentanyl
ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: https://www.asam.org/quality-care/clinical-guidelines/npg
SAMHSA TIP 63 – Medications for Opioid Use Disorder: https://www.samhsa.gov/resource/ebp/tip-63-medications-opioid-use-disorder
These resources anchor the medical recommendations and safety practices outlined above and are the standards followed by the clinical team at Rolling Hills Recovery Center.
Conclusion
Safe fentanyl detox means medical support, symptom relief, and a fast plan for aftercare. Key takeaways: seek supervision when risks are present; medications lower cravings & relapse; move quickly into ongoing treatment and supports. Simple, not easy.
Frequently Asked Questions (FAQs)
What is Detox for Fentanyl and How Does it Work?
Detox for fentanyl is a medically supervised process that helps the body clear fentanyl while managing withdrawal.
Because fentanyl is very potent and stored in fatty tissue, symptoms can start later and last longer than with some other opioids.
Clinicians monitor vitals, treat dehydration, ease pain and nausea, and begin medication for opioid use disorder when appropriate.
The main goals in detox for fentanyl are safety, symptom relief, and a smooth start to ongoing treatment, not just “toughing it out.”
How Long Does Detox for Fentanyl Take, and What Symptoms Should Be Expected?
Most people feel early withdrawal within 12–48 hours after the last use, with symptoms peaking around days 2–4. With fentanyl, anxiety, poor sleep, and cravings can linger for 1–3 weeks.
Common symptoms during detox for fentanyl include chills, sweating, muscle and bone aches, stomach cramps, nausea or vomiting, diarrhea, gooseflesh, dilated pupils, fast heartbeat, and restlessness.
The care team often uses the COWS scale to track severity and adjust treatment. It’s uncomfortable, yes, but treatable and time-limited.
Which Medicines Are Used in Detox for Fentanyl, and Are They Safe?
During detox for fentanyl, evidence-based medicines reduce withdrawal and lower relapse risk:
• Buprenorphine (Suboxone/Subutex) can start once moderate withdrawal is present; some patients benefit from “microdosing” (Bernese method) to lower the chance of precipitated withdrawal with fentanyl.
• Methadone is another effective option for stabilization, especially for those with high tolerance or complex histories.
• Adjuncts like clonidine or lofexidine for sweats and anxiety, NSAIDs for body aches, loperamide for diarrhea, ondansetron for nausea, and hydroxyzine for sleep can help. These medications are safe when prescribed and monitored by a trained clinician. In pregnancy, methadone or buprenorphine is preferred and considered safe. Detox for fentanyl should always include overdose education and naloxone at discharge.
Is At‑Home Detox for Fentanyl Safe?
At-home detox for fentanyl is risky. Fentanyl can cause prolonged, spiking withdrawal and dehydration; there’s also danger from hidden benzodiazepines or xylazine in the supply.
Supervised care is strongly advised if there’s a pregnancy, heart or lung disease, polysubstance use, a history of severe withdrawal, seizures, suicidal thoughts, or no reliable support at home.
Suppose someone still attempts home detox for fentanyl. In that case, they need daily medical check-ins, plenty of fluids with electrolytes, and a clear plan to start buprenorphine & ongoing care fast, but the safer choice is clinical supervision.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












