Choosing between Vyvanse and Adderall can feel confusing for adults, parents, and caregivers. A New Jersey clinician explains how these stimulants work, who may benefit, and what to expect, including dosing, side effects, misuse risks, and safe monitoring. The goal: practical, evidence-based insight that supports ADHD care while protecting health and recovery.
Key Takeaways
- Vyvanse and Adderall both treat ADHD; Vyvanse is a prodrug (lisdexamfetamine) with a smoother rise, and Adderall is mixed amphetamine salts. There is no one-to-one dose match, so choices hinge on symptom pattern, duration needs, and tolerability.
- Timing matters. Vyvanse starts in about 1–2 hours and may last 10–14 hours; Adderall IR works ~4–6 hours, XR about 10–12. Morning dosing, watch sleep and appetite, very acidic drinks can blunt the effect.
- Safety first: screen for heart risks, monitor BP & pulse, weight, anxiety, and sleep. Avoid MAOIs, store meds locked, never mix with alcohol or other stimulants; use New Jersey’s prescription monitoring for safer care.
- Track progress with simple tools (Vanderbilt, ASRS), pair meds with skills, routines, and school supports. When switching, start low, reassess in 1–2 weeks; adjust if there’s rebound or wear‑off late day.
Mechanism and Indications
What They Are and How They Work
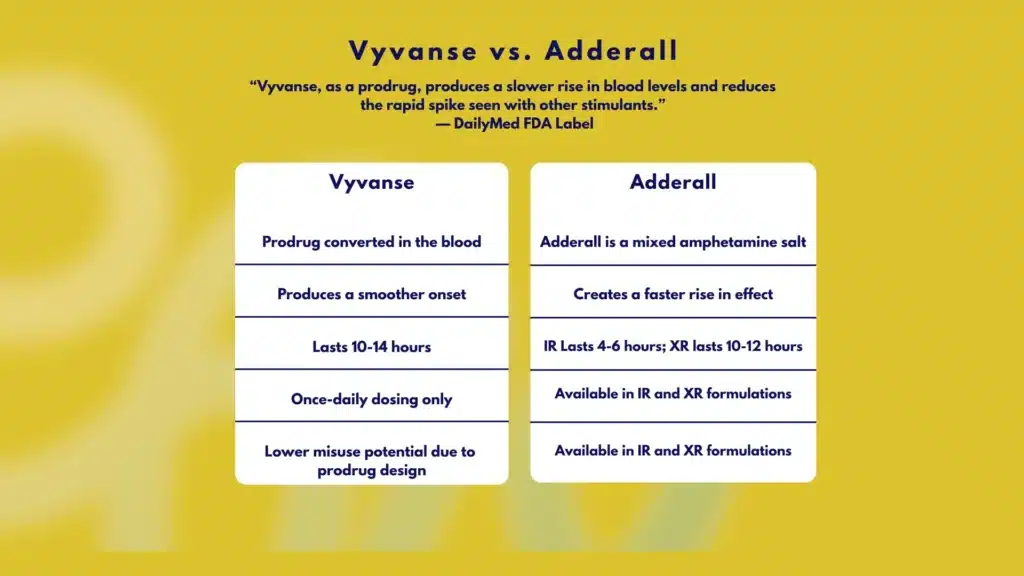
Vyvanse (lisdexamfetamine dimesylate) is a prodrug. After swallowing, it is converted in the blood, primarily inside red blood cells, into active dextroamphetamine. This built‑in step slows the rise in blood levels, which often produces a smoother onset and a lower “rush.” That can reduce the appeal of tampering (for example, crushing and insufflating) but does not eliminate misuse risk. See DailyMed: Vyvanse prescribing info.
Adderall is a mixed amphetamine salt (MAS), containing both dextroamphetamine and levoamphetamine. The IR tablets release medication quickly. The XR formulation uses beads that dissolve in two phases: an initial release, then a delayed pulse, to extend action across the day. See DailyMed: Adderall XR prescribing info.
Both medicines increase synaptic dopamine and norepinephrine, improving attention, impulse control, and working memory. Clinically, both are first‑line for ADHD in children, adolescents, and adults.
FDA‑Approved Uses
- ADHD: Vyvanse (ages 6+). Adderall IR (ages 3+ on label, though most clinicians start at 6+); Adderall XR (ages 6–17 and adults).
- Binge Eating Disorder (BED): Vyvanse is approved for adults with moderate to severe BED. Not approved for weight loss, and not indicated in obesity. Stimulants can be misused for weight control, an important safety topic during shared decision‑making.
- Narcolepsy: Adderall IR has an indication; Vyvanse does not.
Schedule and New Jersey Context
- Controlled substance status: Both are Schedule II under federal and New Jersey law. No refills are allowed; each prescription must be issued separately. Electronic prescribing is standard; prescribers should check the NJ Prescription Monitoring Program (NJPMP) before initiating or changing therapy.
- Diversion control: New Jersey clinicians are expected to assess misuse risk, secure informed consent, and document monitoring strategies.
- School coordination: For students, the prescriber can provide standardized school medication forms so the school nurse can administer doses, especially if an Adderall IR mid‑day dose is needed.
Onset, Duration and Dosing
Quick Comparison

| Feature | Vyvanse (lisdexamfetamine) | Adderall IR (mixed amphetamine salts) | Capsule can be opened and sprinkled on applesauce; do not chew the beads |
|---|---|---|---|
| Active moiety | Converts to dextroamphetamine (prodrug) | d- and l-amphetamine salts | d- and l-amphetamine salts in extended-release beads |
| Typical onset | ~1–2 hours | ~30–60 minutes | ~60 minutes |
| Typical duration | ~10–14 hours | ~4–6 hours | ~10–12 hours |
| Usual dosing | Once daily AM | 1–3 times daily | Once daily AM |
| FDA indications | ADHD (6+); BED (adults) | ADHD (3+); narcolepsy | ADHD (6–17 and adults) |
| Abuse‑deterrent features | Prodrug reduces rapid spikes | None specific | Bead XR; not abuse‑deterrent |
| Administration options | Capsule or chewable; capsule contents can be mixed in water, yogurt, or orange juice | Swallow tablet | Capsule can be opened and sprinkled on applesauce; do not chew beads |
Actual duration varies by person and dose; acidic foods or GI pH can shorten action for any amphetamine.
Dosing Basics and Titration
- Vyvanse: Once each morning. ADHD: start 20–30 mg daily; increase by 10–20 mg weekly; typical range 30–70 mg. BED: start 30 mg, titrate to 50–70 mg. The maximum label dose is 70 mg/day.
- Adderall IR: Start 5 mg once or twice daily; increase by 5 mg at weekly intervals; common total daily dose 10–40 mg split into 2–3 doses (morning and early afternoon; sometimes early evening is avoided due to insomnia). The label maximum commonly cited is 40 mg/day in ADHD.
- Adderall XR: Once daily in the morning. Children 6–12 years: start 10 mg; max labeled 30 mg/day. Adolescents 13–17: start 10 mg, may increase to 20 mg/day. Adults: recommended 20 mg/day; some patients require adjustments within label recommendations.
There is no reliable mg‑to‑mg equivalence between Vyvanse and Adderall. Cross‑titration uses clinical response, not a strict conversion factor. A practical starting point when switching from Adderall to Vyvanse is a once‑daily morning Vyvanse dose based on prior total daily amphetamine exposure, then adjust weekly. The reverse is similar: pick an initial Adderall dose that seems reasonable for symptom coverage, then titrate.
Administration Tips
- Morning dosing improves sleep. If insomnia emerges, move the dose earlier or reduce the dose.
- Avoid crushing XR beads or IR tablets. Vyvanse capsules can be opened and mixed; consume right away.
- Acidifying agents (vitamin C, fruit juices, and antacids that acidify urine) can reduce absorption and shorten the effect. Alkalinizing agents can increase levels.
- Encourage regular meals and hydration; stimulants can blunt appetite, and dehydration worsens headaches.
Generic Availability and Cost
- Lisdexamfetamine now has generics in the U.S., which has improved access, but shortages still occur.
- Adderall IR and XR have multiple generics. XR generics vary in release profiles from the brand for some patients.
- Insurance in NJ often requires prior authorization. Clinicians may provide documentation of impairment and previous trials. Pharmacy discount tools or manufacturer savings programs can help reduce costs.
Switching or co‑prescribing and NJPMP
When switching, checking the NJPMP protects against duplicate therapy and diversion. Co‑prescribing IR “booster” doses with Vyvanse or XR can be appropriate in the late afternoon for homework or shift work, but only with clear functional targets and careful monitoring.
Efficacy and Side Effects
Efficacy
Meta‑analyses and clinical experience show both Vyvanse and Adderall provide similar ADHD symptom reduction across age ranges when dosed correctly. The clinical choice often hinges on:
- Duration needed (school day vs entire workday and evening).
- Tolerability of side effects (anxiety, appetite loss).
- Misuse risk and family history.
- Patient preference for once‑daily vs flexible dosing.
For BED, only Vyvanse carries an FDA indication. Behavioral therapies and nutrition support remain core parts of care.
For a broad overview of ADHD and treatment options, see NIMH ADHD overview.
Common Adverse Effects and Monitoring
Expect and monitor:
- Decreased appetite, weight loss, and stomach upset.
- Insomnia or delayed sleep onset.
- Dry mouth, headache.
- Irritability, anxiety, jitteriness.
- Increased heart rate and blood pressure; palpitations.
- Occasionally, tics may worsen; they are often transient.
Monitoring plan:
- Baseline vitals (BP, HR), height, and weight; repeat at least every 3 months during titration, then periodically.
- Ask about sleep quality, appetite, mood, and new or worsening anxiety.
- In children, plot growth curves; consider medication holidays judiciously if growth falters, weighing risks and benefits.
Cardiovascular screening:
- Review personal/family history of structural heart disease, syncope, sudden death under 40, or arrhythmias.
- Perform a cardiac exam; obtain an EKG if history suggests risk or if symptoms arise during treatment. Referral to cardiology when in doubt.
Drug interactions and cautions:
- Do not use with MAOIs, or within 14 days of stopping an MAOI.
- Caution with other drugs that raise BP/HR (decongestants); some antidepressants (SSRIs/SNRIs) may increase side effects.
- Bupropion plus stimulants can increase seizure risk in predisposed patients.
- Acidifying agents may reduce the effect; alkalinizing agents may increase exposure.
- Alcohol can amplify stimulant effects and impair judgment, leading to avoidance.
Special populations:
- Pregnancy: weigh benefits vs risks. Stimulants can affect fetal growth; if continued, use the lowest effective dose and coordinate obstetric care. Behavioral therapy may be preferred when feasible.
- Lactation: amphetamines are excreted in breast milk; monitor the infant for irritability and weight gain if maternal therapy is necessary.
- Substance use disorders (SUD): higher misuse risk requires stricter boundaries, long‑acting options, pill counts, and frequent follow‑ups. Readers seeking clarity on physiological dependence versus addiction may find this resource helpful: drug dependence vs drug addiction.
Misuse, Diversion and Safety

Vyvanse and Adderall are Schedule II with real dependence and addiction potential. The prodrug design of Vyvanse may lower euphoria with non‑oral routes; however, diversion and misuse still occur. Research on prescription stimulant misuse patterns can be reviewed via NIDA: prescription stimulant misuse.
Rolling Hills Recovery Center treats stimulant addiction and co‑occurring disorders in New Jersey. In practice, safety rests on structure and support.
Safe handling and misuse‑prevention checklist:
- Store medication locked, not in a backpack or car. Track pill counts weekly.
- Use one pharmacy; avoid early refills, as lost prescriptions are warning signs.
- Do not share pills with friends or family. It is illegal and dangerous.
- Avoid mixing with alcohol, energy drinks, or other stimulants.
- For college students, consider a medication contract and pharmacy blister packs.
Red flags to discuss immediately:
- Taking extra doses “to catch up” or binging on weekends.
- Snorting or chewing XR beads; combining with alcohol.
- Escalating dose without prescriber direction.
- Doctor shopping; conflicting stories about lost pills.
Overdose or severe reaction, act fast:
- Symptoms: chest pain, severe agitation, confusion or hallucinations, vomiting, very high body temperature, strong pounding heartbeat, seizures, fainting.
- Call 911. If unsure, call Poison Control at 1‑800‑222‑1222 (U.S.). Cool the patient if hyperthermia is suspected; do not give additional stimulants or alcohol.
Support beyond medication:
- ADHD coaching, cognitive behavioral therapy, organizational tools, and school/work accommodations are key. Document accommodations via a 504 plan or IEP for students.
Choosing or Switching

Shared Decision‑Making in New Jersey
A careful, stepwise plan reduces risk and improves outcomes. Document:
- Specific goals tied to function (for example, complete homework before 7 pm three nights per week; cut careless errors on reports).
- Baseline vitals and weight; sleep patterns; diet.
- Baseline rating scales: Vanderbilt (child), SNAP‑IV (child), ASRS v1.1 or DSM‑5 Adult ADHD rating scale (adult). Keep copies in the chart.
Useful tools and templates:
- Weekly ADHD check‑in (self or parent/teacher): note morning focus, midday stamina, late‑day wear‑off, appetite, bedtime.
- 3‑column symptom tracker: time of day; helpful effects; side effects. Bring to each visit.
- Sleep log: bedtime, sleep latency, night awakenings, wake time, naps, caffeine.
A simple weekly check‑in template:
- Morning: focus, task completion, side effects (0–10 scale)
- Afternoon: focus, energy, appetite (0–10)
- Evening: rebound symptoms, mood, sleep readiness (0–10)
- Notes: missed doses, dietary changes, stressors
Starting Low and Titrating
- Begin with the lowest practical dose that covers morning classes or the first work block.
- Increase weekly until symptoms improve and side effects are acceptable. If side effects persist, step back one increment.
- For sleep issues, adjust timing; add a calming bedtime routine; reduce caffeine. If insomnia continues, consider a different agent or a shorter‑acting plan.
Evaluating Wear‑Off and Rebound
Ask specifically about:
- A sharp drop in focus around mid‑afternoon (may need XR instead of IR, or a small IR “booster”).
- Late‑day irritability, tearfulness, or restlessness (rebound). Consider a tiny IR dose earlier in the afternoon or switching to a smoother formulation like Vyvanse.
Co‑Occurring Conditions
- Anxiety disorders: stimulants can increase jitteriness; sometimes, lower doses with therapy are best. Nonstimulants may be considered if anxiety predominates.
- Tics: amphetamines can transiently increase tics in some, though many do fine. If tics worsen and are impairing, switch classes.
- SUD history: prefer once‑daily, long‑acting options; avoid surplus pills; schedule frequent visits; use NJPMP at each change. Rolling Hills Recovery Center can coordinate addiction care alongside ADHD treatment, keeping safety at the forefront.
How to Transition Between Vyvanse and Adderall
In most cases, no washout is needed when switching from one stimulant to another. The next morning, start the new medicine at a conservative dose. Do not overlap two amphetamine products unless specifically directed.
Step‑by‑step transition (example: Adderall XR to Vyvanse):
- Choose a weekday to switch; ensure no important exams or deadlines that day.
- Stop Adderall XR after the last scheduled dose.
- Next morning, start Vyvanse at 20–30 mg.
- Check vitals at home if possible; note appetite and focus every 3 hours on day 1–2.
- Adjust by 10–20 mg each week based on function and side effects.
- Consider adding a small Adderall IR “booster” only if afternoon coverage is still inadequate, and only after discussion with the prescriber.
- Reassess in 1–2 weeks; document goals met, tolerability, and any red flags.
- Prescriber checks NJPMP to verify the single prescriber/pharmacy and no duplication.
Reverse transition (Vyvanse to Adderall XR or IR) follows the same framework: stop Vyvanse one day, start Adderall the next morning at a modest dose, then titrate.
Coordinating Across Prescribers and Pharmacies
- Use one prescriber whenever possible; if a specialist is added, clarify who manages stimulants.
- Use one pharmacy; ask the pharmacist to note any supply changes (shortages) and communicate alternatives.
- Clinicians in NJ should check NJPMP at initiation and at each major change or early refill request.
- If treatment stalls, revisit the diagnosis. ADHD symptoms can overlap with sleep apnea, depression, trauma, thyroid problems, or substance use.
Practical Dosing Schedules By Need
- School day only: Adderall IR at 7:30 am and noon; or Adderall XR at 7:30 am.
- Work plus evening homework: Vyvanse at 6:30–7:30 am; consider a tiny IR booster at 4 pm if needed.
- Shift work: discuss off‑label timing; be vigilant about insomnia and nutrition.
Nutrition and Sleep During Treatment
- Breakfast with protein within one hour of dosing can blunt appetite suppression later. Pack a calorie‑dense lunch if appetite dips.
- Hydrate. Aim for water intake throughout the day; caffeine may worsen anxiety.
- Maintain sleep hygiene: consistent bedtime, dim screens at night, calming routine. If persistent insomnia, adjust dose timing or consider behavioral sleep strategies first.
When Stimulant Treatment is Not the Right Fit
If misuse risk grows or side effects are not manageable, pause and consider alternatives:
- Nonstimulants: atomoxetine, guanfacine ER, clonidine ER, or bupropion (off‑label).
- Psychotherapy and skills training while reassessing.
- For individuals noticing loss of control with stimulants or other substances, it may be time to talk with a specialist. This brief piece on the top 10 most addictive drugs offers helpful context for risk awareness.
Additional Clinical Notes
Documentation Essentials
- Diagnosis basis: history, impairment documentation, rating scales, collateral from school or workplace.
- Informed consent: risks, benefits, alternatives; Schedule II status; refill policy; NJPMP checks; safe storage plan.
- Treatment plan: goals, titration schedule, monitoring, and next follow‑up date.
- Education materials: provide FDA Medication Guides; link to DailyMed: Vyvanse and DailyMed: Adderall XR.
Special Scenarios Often Seen in New Jersey Practices
- College transitions: Plan for continuity of care, locked storage in dorms, and local pharmacy availability. Consider an on‑campus counseling referral and academic accommodations.
- Driving safety: Stimulants generally improve driving in ADHD; avoid driving during initial titration days or if feeling overstimulated.
- Athletics: Monitor hydration, heat risk, and heart rate; disclose stimulant use if governed by athletic bodies requiring therapeutic use exemptions.
When to Escalate Care
- Repeated early refills, dose escalation without guidance, or combining with alcohol/benzodiazepines signals a higher risk. Discuss a structured taper and evaluation for SUD. Rolling Hills Recovery Center integrates evidence‑based stimulant addiction treatment with psychiatric care, an approach that can stabilize both ADHD and substance use.
Patient Education Points That Stick
- It’s normal to fine‑tune dose and timing. A perfect day one is rare.
- Eat something early, even if small. Keep a protein snack for later.
- Tell the prescriber about new chest pain, fainting, severe anxiety, or persistent insomnia.
- Medication treats symptoms; skills make changes last. Pair both.
- Never share pills, ever. It’s not “helping,” it’s dangerous and illegal.
Evidence Anchors and Further Reading
- FDA labeling remains the definitive source for dosing, warnings, and administration: DailyMed: Vyvanse prescribing info; DailyMed: Adderall XR prescribing info.
- General ADHD education for families and adults: NIMH ADHD overview.
- Misuse and diversion prevention: NIDA: prescription stimulant misuse.
- Prescribers practicing in NJ should regularly access and use the NJ Prescription Monitoring Program to enhance safety across settings.
Conclusion
Bottom line: choose meds based on symptom relief, duration, and safety. Start low, monitor sleep & appetite, and guard against misuse. Then adjust.
Frequently Asked Questions (FAQs)
What is the Main Difference in How Vyvanse vs Adderall Works?
Vyvanse is a prodrug (lisdexamfetamine) that the body converts to dextroamphetamine, which gives a slower, smoother onset and a steady effect. Adderall contains mixed amphetamine salts (d- and l-amphetamine), so the onset is faster, and the effect can feel more immediate.
Both are stimulants for ADHD, and both are Schedule II. Vyvanse may be harder to misuse by crushing or injecting because it must be metabolized first. Either can work well when dosed and monitored carefully.
Vyvanse vs Adderall: Which Lasts Longer, and When Should it Be Taken?
Vyvanse is usually taken once daily in the morning; it starts in about 1–2 hours and can last 10–14 hours. Adderall comes in immediate-release (IR) and extended-release (XR) forms. IR starts in 30–60 minutes, lasts ~4–6 hours, and may need 2–3 doses; XR often lasts 10–12 hours. To reduce insomnia, avoid late-day doses. Food can slow the onset a bit, and very acidic drinks may blunt the effect, so timing meals & beverages helps.
Is Vyvanse vs Adderall Safer For Someone in Recovery From Substance Use?
Both have misuse and dependence risks. Vyvanse’s prodrug design can lower tampering risk, yet diversion still happens. In recovery, safety comes from structure: one prescriber, prescription monitoring, no early refills, secure storage, pill counts if needed, and clear goals. Watch for red flags like dose chasing, binging, or using with alcohol or other stimulants, don’t mix. Regular checks of sleep, appetite, heart rate, and blood pressure improve safety.
How Do You Switch Safely Between Vyvanse vs Adderall?
There is no milligram‑to‑milligram match between the two. A clinician will typically pause or use a brief washout day, then start low and go slow on the new medicine, adjusting weekly. Morning dosing is preferred. Track benefits and side effects (focus, irritability, wear‑off, appetite, sleep) and measure vitals. Avoid monoamine oxidase inhibitors, and alert the prescriber to pregnancy, heart disease, or tic history. Tight follow‑up in the first 1–2 weeks matters… a lot.
How Does Rolling Hills Recovery Center Help When Vyvanse vs Adderall Questions Overlap with Addiction Care in New Jersey?
When ADHD medication is part of the picture, the team collaborates with prescribing clinicians, supports safe use plans, monitors for misuse risk, and integrates therapy and relapse prevention. The focus is whole-person recovery, clear thinking, stable routines, and sustainable health.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












