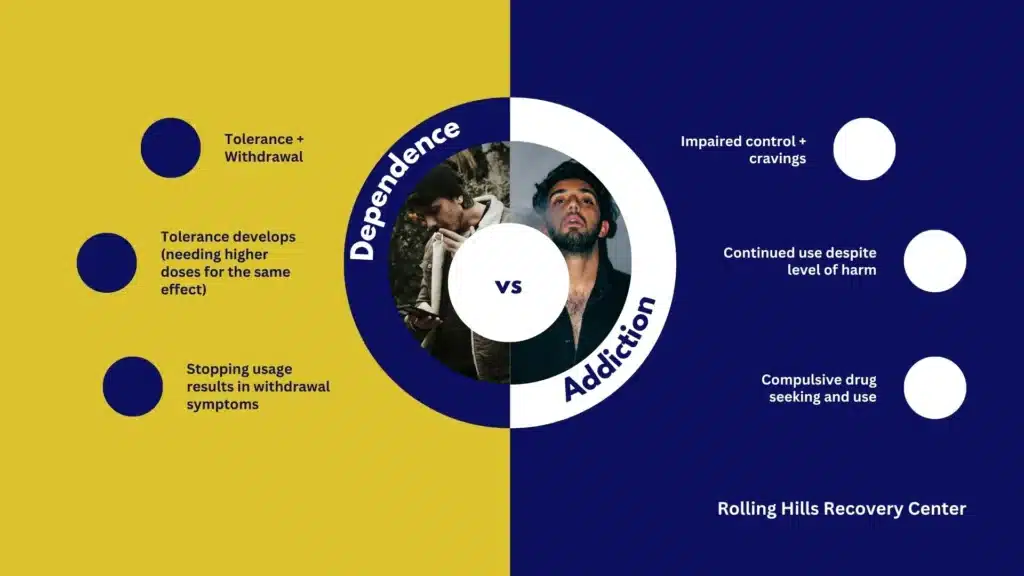
Understanding the difference between drug dependence and addiction helps families and patients make safer choices and find the right care.
From a clinical standpoint, these terms are related yet distinct: tolerance and withdrawal reflect physical dependence, while addiction involves impaired control, cravings, and continued use despite harm.
This overview explains signs, risks, & evidence-based help.
Key Takeaways
- Drug dependence is not the same as addiction; dependence involves tolerance and withdrawal, while addiction adds loss of control and continued use despite harm.
- Watch for early signs: strong cravings, needing more for the same effect, spending a lot of time using or recovering, mood, sleep, and appetite changes; risky use can creep in.
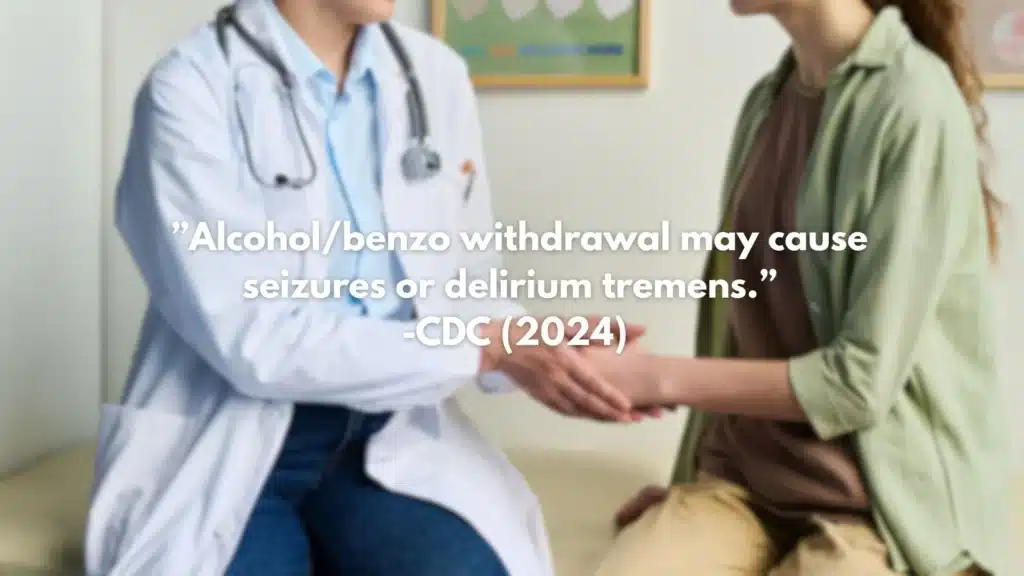
- Withdrawal safety matters. Alcohol and benzodiazepine withdrawal can be dangerous (seizures); opioid withdrawal is rarely life‑threatening but very hard. Use validated tools (CIWA‑Ar & COWS), and do not stop benzos suddenly.
- Treatment works when care blends medicine and counseling, buprenorphine or methadone for opioid use disorder; naltrexone or acamprosate for alcohol; plus CBT, motivational interviewing, contingency management, naloxone, and fentanyl test strips; steady follow‑up helps.
What Drug Dependence Means vs Addiction (Substance Use Disorder)
Definitions That Matter in Care
- Dependence: the body adapts to a substance. Tolerance develops (needing more for the same effect), and stopping the drug triggers withdrawal. Dependence can occur with many medications used exactly as prescribed.
- Addiction (substance use disorder, SUD): a medical condition defined by impaired control, cravings, continued use despite harm, and functional problems. Dependence may be present, but addiction is about behavior and consequences as well as brain changes.
- Misuse: taking a medication differently than prescribed or using a substance in a way that increases risk, whether or not addiction is present.
A quick comparison to keep terms straight:
| Term | Core meaning | Key features | Withdrawal likely? |
|---|---|---|---|
| Dependence | Physiological adaptation to a drug | Tolerance, withdrawal: can be expected with long-term use | Often |
| Addiction (SUD) | Compulsive use despite harm | Loss of control, cravings, continued use despite problems | Common but not required |
| Misuse | Risky or non-prescribed use | Higher-than-prescribed doses, non-medical use | Possible |
Authoritative clinical overviews are available from the American Psychiatric Association’s DSM-5-TR description of substance use disorders and related withdrawal syndromes (see APA DSM-5-TR overview), and from the National Institute on Drug Abuse (NIDA).
- NIDA: https://nida.nih.gov
- APA DSM-5-TR overview: https://www.psychiatry.org/psychiatrists/practice/dsm
What’s Happening in the Brain: Neuroadaptation
With repeated exposure, the brain adjusts in reward, stress, and self-control circuits:
- Reward circuit (dopamine): over time, the same dose produces less reinforcement; cues begin to trigger craving.
- Stress systems (CRF, noradrenaline): withdrawal and negative mood states appear between doses, pushing continued use.
- Prefrontal control: planning and impulse control networks weaken, making it harder to resist urges.
These adaptations explain why someone may feel “normal” only when using and why stopping without support is so difficult. The World Health Organization offers a plain-language overview of substance dependence and harm reduction approaches: https://www.who.int/health-topics/substance-abuse
Physical vs Psychological Dependence
- Physical dependence: tolerance and predictable withdrawal symptoms (e.g., sweating, tremor, diarrhea, insomnia).
- Psychological dependence: cravings, anxiety, or low mood when not using, drug-related thoughts dominating mindshare.
Both can happen together. Management plans usually address both medications to stabilize physiology and therapies to build new coping skills.
Common Substances Linked to Dependence
- Prescription opioids: oxycodone, hydrocodone, morphine; illicit opioids include heroin and fentanyl.
- Benzodiazepines: alprazolam, clonazepam, diazepam, lorazepam.
- Stimulants: prescription (amphetamine, methylphenidate) and illicit (cocaine, methamphetamine).
- Alcohol and nicotine: highly prevalent and frequently co-occur.
For fast facts on addictive potential across drug classes, see the educational page on the most addictive drugs.
Polysubstance Patterns and Fentanyl Contamination
In New Jersey and nationally, fentanyl has spread beyond heroin into counterfeit pills and powder supplies (including stimulants). People may not know what they are taking. This raises overdose risk and complicates withdrawal. CDC’s Overdose Prevention resources explain current trends and safety practices: https://www.cdc.gov/overdose-prevention/index.html.
MedlinePlus provides FDA-sourced monographs for specific medicines, side effects, and interactions: https://medlineplus.gov/druginformation.html
Causes and Risk Factors
Biology and Family History
- Genetics: heritable risk explains a significant portion of vulnerability to SUDs.
- Early exposure: adolescent brain development is still underway; reward systems are more reactive while control systems mature later.
- Sex and hormonal factors: can influence patterns of use, sensitivity, and withdrawal.
Mental Health and Trauma
- Co-occurring disorders: depression, anxiety, PTSD, ADHD, and bipolar disorder commonly intersect with substance use.
- Trauma and chronic stress: increase risk of initiation, escalation, and relapse.
- Pain conditions: both acute and chronic pain can increase exposure to opioids and sedatives; untreated pain can drive misuse.
Medicines and Medical Prescribing
- Long-term prescriptions (opioids, benzodiazepines, stimulants) raise dependence risk, even when taken as directed. This does not imply wrongdoing.
- Rapid dose escalations and high-potency agents add to risk.
Social and Environmental Factors
- Social determinants: unstable housing, unemployment, legal stress, and lack of transportation limit access to safer care.
- Social networks: availability, peer use, and norms strongly shape risk and recovery.
- Health care access: insurance gaps and limited providers trained in addiction medicine can delay treatment.
For those in New Jersey, fentanyl-adulterated supplies and intermittent access to prescribed medications (e.g., when prescribers stop abruptly) create hazardous swings; patients deserve a compassionate, planned approach. Stigma reduction matters: use person-first language (“person with opioid use disorder,” not “addict”) to support dignity and care engagement.
Signs and Symptoms
Behavioral Signs
- Strong cravings
- Taking more or longer than intended
- Unsuccessful attempts to cut down
- Significant time spent obtaining, using, or recovering
- Role impairment at work, school, or home
- Continued use despite health, relationship, or legal problems
- Using in hazardous situations (e.g., driving)
NIDA and DSM-5-TR emphasize that these features, persisting over 12 months, define SUD severity.
Physical Signs
- Pupillary changes: opioids often cause pinpoint pupils; stimulants may dilate.
- GI issues: constipation with opioids; nausea or abdominal cramps during withdrawal.
- Sleep problems: insomnia, fragmented sleep, or hypersomnia post-binge.
- Weight changes, dental issues (e.g., with methamphetamine), skin infections from injection or picking.
- Sexual dysfunction, menstrual irregularities.
Withdrawal Clusters to Recognize
- Opioid withdrawal: anxiety, muscle aches, yawning, watery eyes, runny nose, sweating, gooseflesh, abdominal cramping, diarrhea, vomiting, dilated pupils, poor sleep.
- Sedative-hypnotic (benzodiazepines, alcohol) withdrawal: tremor, sweating, agitation, anxiety, insomnia, perceptual changes; in severe cases, seizures, delirium, medical emergency.
- Stimulant withdrawal: depressed mood, fatigue, hypersomnia or insomnia, increased appetite, psychomotor slowing, anhedonia, intense craving.
Red Flags
- Escalating dose, using sooner than scheduled, or multiple prescribers (“doctor shopping”)
- Using alone, recent overdose, or mixing opioids with benzodiazepines and alcohol
- Notable life consequences that keep worsening despite attempts to stop
Assessment and Diagnosis
DSM-5-TR Criteria and Severity
Substance use disorder is diagnosed when at least 2 of the 11 criteria are present within 12 months; severity is based on count:
- Mild: 2–3 criteria
- Moderate: 4–5 criteria
- Severe: 6 or more criteria
Severity informs the level of care and treatment plan. DSM-5-TR also defines substance-specific intoxication and withdrawal syndromes that guide safety decisions.
Brief Screening Tools: What to Use and How
- ASSIST (WHO Alcohol, Smoking and Substance Involvement Screening Test): good for multiple drugs.
- Steps: administer 8 questions; score per substance; brief feedback; offer referral if moderate/high risk.
- Tool info: https://www.who.int/publications/i/item/978924159938-2
- DAST-10 (Drug Abuse Screening Test-10): quick screen for drugs other than alcohol.
- Steps: 10 yes/no items; 1–2 mild, 3–5 moderate, 6–8 substantial, 9–10 severe concerns; discuss results.
- AUDIT (Alcohol Use Disorders Identification Test) or AUDIT-C:
- Steps: score; discuss low-risk limits; plan next steps based on risk.
Brief administration tips:
- Normalize: “These questions are routine for everyone.”
- Ask matter-of-factly and without judgment.
- Share scores and what they mean in simple language.
- Use a 3-step brief intervention: Raise concern, Elicit change talk, Offer options.
Urine Drug Testing: Use and Limits
Helpful for:
- Baseline assessment and monitoring safety
- Confirming recent exposure when history is unclear
- Identifying unexpected fentanyl or benzodiazepine exposure
Limitations:
- False positives and negatives occur; immunoassays are screening tools, not confirmation
- Detection windows vary by drug, dose, and metabolism
- Results never replace a good clinical conversation
Confirm unexpected results with specific assays when needed. Use testing collaboratively, explain the purpose, and obtain consent.
Differential Diagnosis to Keep in Mind
- Anxiety disorders or panic mimicking stimulant effects
- Chronic pain syndromes and hyperalgesia from opioid exposure
- Thyroid or adrenal issues affecting energy, mood, or sleep
- Primary sleep disorders
- Seizure risk unrelated to substance use
A careful history, exam, and targeted labs help separate substance effects from other conditions.
Safety Triage for Withdrawal and Detox
- Alcohol/benzodiazepine risk: use CIWA-Ar to rate alcohol withdrawal; high scores, history of severe withdrawal, or comorbid illness require medical detox.
- Opioid withdrawal: use COWS to stage severity; moderate withdrawal (COWS ≥ 8–12) is the typical threshold for starting buprenorphine.
- Criteria for higher level of care: pregnancy, severe comorbid medical conditions, unstable psychiatric symptoms, seizures or delirium risk, lack of safe support at home.
If there is any concern for complicated withdrawal, arrange medically supervised stabilization.
Informed Consent and Confidentiality Basics
- Explain diagnosis, benefits, and risks of treatments, and alternatives.
- Review privacy protections (42 CFR Part 2 and HIPAA) for substance use treatment information.
- Obtain written consent before sharing information, except in specific emergencies allowed by law.
- For adolescents, discuss state-specific consent rules and family involvement.
Evidence-Based Care and Recovery
Rolling Hills Recovery Center in New Jersey provides evidence-based treatment and complementary holistic supports. The approach is patient-centered, practical, and integrated with medical and mental health care.
Medications for Opioid Use Disorder (OUD)
- Buprenorphine (Suboxone and similar):
- Partial opioid agonist that reduces craving and withdrawal; lowers overdose risk.
- Start when in moderate withdrawal (COWS ≥ 8–12) to avoid precipitated withdrawal.
- Office-based prescribing: strong retention benefits.
- Methadone:
- Full agonist dispensed in accredited opioid treatment programs.
- Best for those with high tolerance, prior buprenorphine non-response, or when structure is helpful.
- Extended-release naltrexone:
- Opioid antagonist given monthly after full detox (7–10 days opioid-free).
- Useful for motivated individuals who prefer non-agonist therapy.
NIDA has detailed, clinician-friendly summaries on OUD medications: https://nida.nih.gov/publications
Step-by-step buprenorphine start (simplified):
- Confirm OUD diagnosis and recent use.
- Check COWS score and last opioid time.
- Provide patient education; obtain consent.
- Start 2–4 mg buprenorphine; reassess in 1–2 hours.
- Titrate in small steps until comfortable (often 8–16 mg/day).
- Schedule close follow-up; add counseling and recovery supports.
Medications for Alcohol Use Disorder (AUD)
- Naltrexone (oral or extended-release injection): reduces heavy drinking days; check liver function; avoid if using opioids.
- Acamprosate: supports abstinence by stabilizing glutamate; renally cleared, safe with liver disease.
- Disulfiram: aversive therapy; requires high motivation and monitoring; avoid if cognitive impairment or unreliable follow-up.
Clinical overviews: https://www.niaaa.nih.gov and MedlinePlus medication monographs.
Behavioral Therapies That Work

- Cognitive behavioral therapy (CBT): identifies patterns, builds coping, and relapse-prevention skills.
- Motivational interviewing (MI): strengthens intrinsic motivation and aligns treatment with patient goals.
- Contingency management (CM): uses tangible rewards for objective recovery targets (e.g., negative tests, attendance).
- Family involvement: CRAFT and family therapy improve outcomes; align boundaries, reduce conflict, and build support.
At Rolling Hills Recovery Center, therapy selection is matched to individual goals, readiness for change, and co-occurring conditions. Trauma-informed care and culturally responsive practices are standard.
Harm Reduction and Overdose Planning

- Naloxone: carry at all times if using opioids or living with someone who does.
- Fentanyl test strips: check drug supply when abstinence isn’t possible; reduces overdose risk.
- Don’t use alone: use buddy systems or call lines; stagger use.
- Avoid mixing: especially opioids with benzodiazepines and alcohol.
- Start low, go slow: potency varies, especially with street-sold pills and powders.
Overdose response steps:
- Try to wake the person; call 911.
- Give naloxone (spray or injection); repeat every 2–3 minutes if needed.
- Rescue breathing if not breathing; then chest compressions if no pulse and trained.
- Stay until help arrives.
New Jersey’s Good Samaritan law generally protects people who seek medical help during an overdose from certain charges. Calling 911 saves lives.
Relapse Prevention and Aftercare Planning
- Identify high-risk situations: HALT (hungry, angry, lonely, tired) and locations or people tied to prior use.
- Build a coping menu: urge surfing, brief breathing practice, delay-and-distraction, call a support person, take a walk.
- Medication adherence: schedule reminders; keep a 7-day pill organizer.
- Recovery supports: mutual-help meetings, peer recovery coaches, faith communities, sober activities.
A simple 48-hour recovery plan template:
- Triggers I might encounter in the next 2 days
- My first response (skill to use)
- Backup plan (person to call)
- Medication times and refills needed
- Sleep and meal plan
- One rewarding, sober activity each day
Wellness Foundations That Make a Difference
- Sleep: target a consistent schedule; wind-down routine; limit late caffeine and screens.
- Nutrition: regular meals with protein, fiber, and fluids; consider a multivitamin early in recovery.
- Exercise: even 10–20 minutes of walking daily improves mood and sleep.
- Medical care: vaccines, wound care, STI testing, and pain management plans that avoid high-risk prescribing.
- Mental health: therapy and, when indicated, medications for depression, anxiety, ADHD, or PTSD.
WHO resources on brief interventions and health system supports for substance use are useful for both patients and caregivers: https://www.who.int/teams/mental-health-and-substance-use
Legal Protections and Practical Help in New Jersey
- NJ Good Samaritan Law: encourages calling 911 in overdoses by offering certain legal protections.
- Parity laws: mental health and substance use benefits must be comparable to medical/surgical benefits under federal law.
- Insurance navigation: many plans cover medication treatment and counseling. See local plan details and verify benefits.
For help understanding coverage, review insurance coverage for drug rehab in NJ.
How to Start Care Now: Step-by-Step
- Safety first
- If there is risk of severe alcohol or benzodiazepine withdrawal (history of seizures, delirium, or heavy daily use), seek medical care or call 911.
- Obtain naloxone if opioids are involved. Many NJ pharmacies and community programs provide it without a personal prescription.
- Brief self-check
- Use the AUDIT-C or DAST-10 online to understand your risk level.
- Write down substances used, amounts, and last use. Bring this list to your appointment.
- Reach out
- Contact a licensed program or medical provider trained in addiction. Ask about buprenorphine/methadone for OUD and naltrexone/acamprosate/disulfiram for AUD.
- Confirm that care includes therapy options and care coordination for mental health.
- Prepare for the first visit
- List current medications and allergies.
- Note past treatments that were helpful or not, including side effects.
- Identify one to two goals for the next two weeks (e.g., “sleep at least 6 hours,” “start buprenorphine,” “attend two therapy sessions”).
- Build a support net
- Tell one trusted person about your plan.
- Add at least one recovery-support activity to your calendar this week.
- Keep up momentum
- Set phone reminders for medications and appointments.
- Celebrate small wins, 48 hours matter, then one week, then one month.
Practical Tools You Can Use Today
- Craving card (wallet-size)
- “If craving hits, I will: 1) Breathe 3x slowly; 2) Text/call [name]; 3) Walk for 10 minutes; 4) Eat a snack; 5) Review why I chose recovery.”
- Medication tracker
- Columns for dose, time taken, refill date, and side effects. Bring to appointments.
- Support map
- List three people, two places, and one activity that help you feel steady. Keep it on your phone.
- Overdose safety checklist (for opioid risk)
- Carry naloxone; don’t use alone; test dose; avoid mixing; call 911 if in doubt.
When Life Feels Stuck
Feeling unable to stop despite the best intentions is common and treatable. See this practical resource on getting unstuck: Are drugs and alcohol making life unmanageable?
Conclusion
Drug dependence is treatable, not a personal failing. Remember: know how dependence differs from addiction, watch for cravings and loss of control, and seek safe withdrawal plus ongoing therapy for mind & body.
If you are in New Jersey and exploring a structured, evidence-based program with integrated medical and behavioral care, Rolling Hills Recovery Center offers a coordinated path forward, built around your goals and safety.
Frequently Asked Questions (FAQs)
What is Drug Dependence?
Drug dependence is a medical condition where the body adapts to a substance, leading to tolerance (needing more to get the same effect) and withdrawal symptoms when use is cut back or stopped.
It reflects brain and body changes, not a lack of willpower. Dependence can develop with prescription medicines or illicit drugs.
How is Drug Dependence Different from Addiction?
Drug dependence involves tolerance and withdrawal. Addiction (a substance use disorder) adds loss of control, intense cravings, and continued use despite harm at home, work, or school.
A person can have dependence without addiction (for example, long-term prescribed opioids), addiction without strong physical dependence, or both together. Knowing the difference helps tailor care.
What Are Early Signs of Drug Dependence to Watch For?
Common early signs include:
• Needing higher doses for the same relief
• Feeling unwell between doses (shakes, nausea, sweats, anxiety)
• Spending more time getting or recovering from the drug
• Sleep changes, mood swings, or falling behind on daily tasks
• Trying to cut down but not being able to
Red flags that need urgent care: severe vomiting, confusion, chest pain, seizures, or thoughts of self-harm.
Is it Safe to Stop “Cold Turkey”?
It depends on the substance. Opioid withdrawal is very uncomfortable but usually not life-threatening; medical support makes it safer and more tolerable.
Benzodiazepine and alcohol withdrawal can be dangerous and even life-threatening; never stop these suddenly without medical supervision. Stimulant withdrawal often brings fatigue, low mood, and cravings.
If unsure, pause... and contact a clinician or go to urgent care for safety.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












