Looking at 30-day rehabs in New Jersey? Here’s the hard truth: a month can stabilize you, start meds, and set a plan, but it won’t finish recovery. I audit programs by what’s provable: licensing, credentials, daily structure, and outcomes, not slogans. Expect blunt checklists, real tools, and clear next steps so you spend money and time smartly.
Key Takeaways
- 30 days = stabilization, not a cure. Start detox if needed, begin MAT, build structure; book step‑down (IOP/outpatient/peer support) before discharge; carry naloxone.
- Verify proof: NJ DMHAS license for the exact address and level, accreditation (The Joint Commission or CARF), and active clinician licenses. No documents = no deal… ok?
- Money first: confirm in‑network vs out‑of‑network, deductible and coinsurance; get an itemized Good Faith Estimate in writing, including labs & meds & UAs; know what’s extra (transport, family lodging).
- Outcomes matter: ask what they track, retention, appointments kept, MAT adherence, overdose education. Vague claims or “cure” talk = fail.
Scope and Definition of 30-Day Rehab in New Jersey
30-day rehab programs are a time-limited treatment episode that typically includes one or more levels of care: detox (if clinically indicated), residential or inpatient services, partial hospitalization (PHP), and intensive outpatient (IOP). In New Jersey, substance use treatment programs must be licensed by the Department of Human Services’ Division of Mental Health and Addiction Services (DMHAS). Accreditation by The Joint Commission or CARF is common but not a substitute for state licensure. Use both.
A 30-day episode can be configured in several ways:
- Detox, then residential/inpatient for the remainder.
- Residential/inpatient only (no detox needed).
- PHP followed by IOP if you’re medically stable.
- Combinations that include medication for opioid use disorder (MOUD) or alcohol use disorder (MAUD), therapy, family work, and discharge planning.
Programs like Rolling Hills Recovery Center in New Jersey combine evidence-based treatment with selected holistic options. That’s fine, if the clinical core is strong, licensed, and measurable.
What 30 Days Actually Covers (Levels of Care)

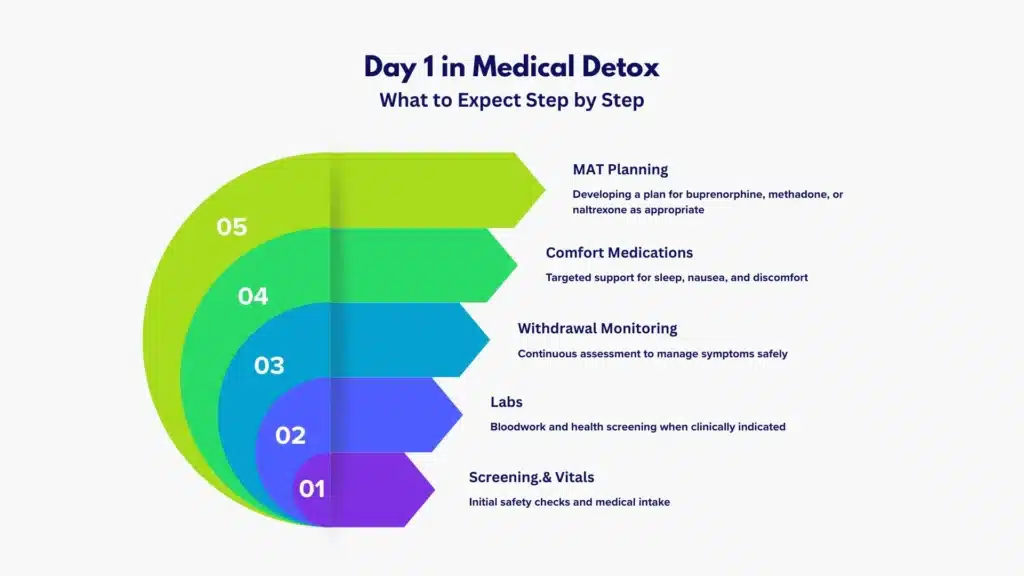
- Medical detox: 24/7 nursing and daily physician oversight to manage withdrawal safely. Alcohol, benzodiazepines, and opioids may require specific protocols. Detox is a short phase (commonly 3–10 days), not treatment completion.
- Residential/Inpatient: 24/7 support, structured therapy schedule, medication management, and relapse prevention in a live-in setting. Appropriate when you need stability or have failed lower levels of care.
- PHP (Partial Hospitalization Program): Typically 5 days per week, 5–6 hours/day (about 20–30 hours/week). No overnight stay; you return home or to recovery housing.
- IOP (Intensive Outpatient Program): Typically 3–5 days per week, 3 hours/day (about 9–15 hours/week). Step-down focus.
A typical 30-day path might be Detox (5–7 days) → Residential (14–21 days) → PHP/IOP (remainder). Or Residential (30 days) with strong discharge planning into IOP.
Comparative View of Levels of Care
| Level of Care | Typical Weekly Clinical Hours | Lodging Included | Medical Coverage | MAT/MOUD/MAUD | Best Use |
|---|---|---|---|---|---|
| Medical Detox (Inpatient) | Initiation is strongly indicated if the criteria are met | Yes | 24/7 nursing, daily MD/DO | Initiation is strongly indicated if criteria are met | Safe withdrawal, stabilization |
| Residential/Inpatient | 20–40+ therapy hours | Yes | MD/DO oversight; RN on site | Ongoing management | Early stabilization, co-occurring needs |
| PHP | ~20–30 | No | MD/DO at least weekly | Continuation or initiation | Step-down; high-intensity outpatient |
| IOP | ~9–15 | No | Medical as needed | Continuation | Step-down; maintenance, relapse prevention |
Core Evidence-Based Care You Should Expect
- Cognitive Behavioral Therapy (CBT)
- Contingency Management (CM), where appropriate
- Motivational Interviewing (MI)
- Medications for opioid use disorder (MOUD: buprenorphine, methadone, naltrexone)
- Medications for alcohol use disorder (MAUD: naltrexone, acamprosate, disulfiram when appropriate)
- Trauma-informed approaches; screening for co-occurring mental health disorders
- Overdose education and naloxone training prior to discharge

If any of these are missing without a clear clinical reason, downgrade the program’s credibility. Absence = failure.
Daily Structure (Example Schedule)
- 7:00 am: Wake-up, vitals if needed, medication pass
- 8:00 am: Breakfast, community meeting
- 9:00–10:30 am: Process group (CBT/MI focus)
- 10:45–12:00 pm: Skills group (relapse prevention, craving management)
- 12:00–1:00 pm: Lunch
- 1:00–2:00 pm: Individual therapy or case management
- 2:15–3:15 pm: Family session (scheduled, not daily)
- 3:30–4:30 pm: Wellness or meditation (holistic adjuncts)
- 5:30 pm: Dinner
- 7:00–8:00 pm: Peer support meeting (on-site or virtual)
- 9:00–10:00 pm: Evening wrap-up, quiet hours
Ask for the written daily and weekly program schedule. If they won’t send it, treat that as a red flag.
Family Contact and Boundaries
- Family involvement should be structured: consent forms, scheduled sessions, clear boundaries (no enabling, no transporting substances, call rules).
- Education for the family on CRAFT principles or similar is a plus.
- Reasonable but bounded contact (phone hours; no unscheduled visits).
- Consider a formal family program; you can explore options like a dedicated family support rehab in New Jersey for ongoing work.
What 30 Days Can and Cannot Accomplish
Can:
- Safely manage withdrawal, stabilize sleep, and nutrition.
- Initiate and stabilize on MAT when indicated.
- Start cognitive and behavioral skill-building.
- Diagnose co-occurring conditions and start medication.
- Build a step-down and aftercare plan with appointments booked.
Cannot:
- “Cure” a chronic condition. Substance use disorders are relapsing, remitting illnesses.
- Replace 6–12 months of continued care.
- Ensure job, housing, and social repair without deliberate post-discharge work.
If a program promises “full recovery” in 30 days without a step-down plan or MAT access, it’s marketing, not medicine.
Admissions and Verification Workflow (Step-by-Step)
- Eligibility call (same day)
- Provide substance use history, medical/psychiatric conditions, current meds, legal issues, and pregnancy status.
- Ask for same-day assessment availability.
- Clinical assessment and medical clearance
- Expect a DSM-5 diagnosis by a qualified clinician and an ASAM level-of-care placement decision.
- Medical screening: vitals, labs if detox indicated, pregnancy test for females of childbearing potential.
- If alcohol or benzodiazepines are involved, ask for the detox protocol and monitoring standard (CIWA/COWS, seizure precautions).
- Insurance verification and pre-authorization
- Confirm in-network vs out-of-network status in writing.
- Ask for estimated out-of-pocket costs by level of care.
- Require written confirmation if a single case agreement is used for out-of-network.
- Verify state licensure (New Jersey DMHAS)
- Request the facility’s NJ DMHAS license number and service types covered.
- Confirm with the New Jersey Division of Mental Health and Addiction Services directory or by contacting DMHAS. Keep a screenshot.
- Validate accreditation
- The Joint Commission (Quality Check) or CARF listing must match the facility name and address.
- No listing or expired accreditation? Proceed cautiously; licensure is mandatory regardless.
- Confirm clinician credentials
- Medical: MD/DO with addiction medicine (ABPM) or addiction psychiatry (ABPN) preferred.
- Therapy: LCSW, LPC, LMFT; addiction-specific credentials like LCADC.
- Nursing: RN coverage on relevant units; LPNs under RN supervision.
- Demand a written treatment plan with measurable goals
- Include diagnosis, level of care, therapy modalities, MAT plan, family engagement, and discharge criteria.
- Goals must be measurable: e.g., “Attend 3 IOP groups/week x 4 weeks; initiate buprenorphine; urine screens weekly; PHQ-9 reduction by X points.”
- Scrutinize medications and MAT
- Ask for the med management policy: Who prescribes? How often are visits? How is diversion prevented?
- Ensure availability of MOUD and MAUD; refusal to offer MAT is non-evidence-based.
- Testing and safety
- Urine drug testing policy (frequency, confirmation testing, cost).
- Overdose education and naloxone on discharge should be standard.
- Red flags
- Vague outcomes like “transformational healing.”
- Upsells to wellness or luxury services without clinical justification.
- No schedule, no staff roster, or reluctance to provide credentials.
- Pressure tactics: “Last bed” or “must pay now or lose your chance.”
Costs and Insurance Realities in New Jersey
- In-network vs out-of-network
- In-network: negotiated rates, lower out-of-pocket if deductibles met.
- Out-of-network: higher deductibles/coinsurance; you may face balance billing unless prohibited by plan.
- Deductibles, copays, and coinsurance
- Ask for your plan’s in-network and out-of-network deductibles separately.
- Clarify coinsurance percentage after deductible (e.g., 20%).
- Ask how costs differ by level of care (detox vs residential vs PHP vs IOP).
- NJ Medicaid (NJ FamilyCare)
- Many 30-day treatment services are covered with prior authorization.
- Verify that the facility accepts your Medicaid managed care organization (MCO). Not all do.
- Parity rights
- Under MHPAEA and NJ law, behavioral health benefits must be on par with medical/surgical benefits. If you face unusual denial or limits, request a written rationale citing plan criteria and ASAM placement guidelines.
- How to read an EOB (Explanation of Benefits)
- It’s not a bill. It shows the provider’s charge, allowed amount, plan payment, and your responsibility.
- Verify CPT/HCPCS codes align with the services you received.
- Compare EOBs with facility invoices. Dispute discrepancies in writing.
- What’s included vs billed separately
- Often included: group therapy, individual therapy, case management, room and board (residential).
- Often billed separately: labs (bloodwork), EKG, medications, urine toxicology (initial screens and confirmations), specialty consults.
- Transport and family lodging: typically not included. Get written estimates if the facility offers transport.
- Get the total cost estimate in writing
- Request a good-faith estimate by level of care, including probable ancillary charges (lab panels, UA confirmatory testing).
- Ask for the refund policy and the financial hardship policy.
- Practical note
- Detox for alcohol in New Jersey may require inpatient medical monitoring; find out information about New Jersey alcohol detox programs and confirm they accept your plan.
Outcomes and Aftercare That Matter
- How rehab success rates are actually tracked
- Retention and completion rates by level of care.
- MAT initiation and adherence at 30, 90, and 180 days.
- Linkage to continuing care within 7 days of discharge.
- Overdose education provided, and naloxone dispensed.
- Readmission rates within 30 and 90 days (context matters).
- 30-day limits
- The relapse risk window remains elevated post-detox and post-discharge. Expect a step-down plan before day 30, not an afterthought on day 30.
- Step-down plan (build it early)
- If your first 2–3 weeks are inpatient, transition to PHP or IOP with appointments set and transportation arranged.
- Peer recovery support (Certified Peer Recovery Specialists) to bridge gaps between levels.
- Outpatient psychiatry and therapy appointments confirmed (with dates).
- Recovery housing
- If home is high-risk, consider recovery housing vetted for safety (drug testing policy, curfews, visitor rules).
- Confirm alignment with your IOP/PHP schedule and MAT storage rules.
- Follow-up booked before discharge
- IOP/PHP start date, time, and address.
- Prescriber follow-up for buprenorphine, methadone clinic slot, or naltrexone injection date.
- Primary care appointment if needed.
- Community peer supports (AA/NA or secular alternatives) with first meetings identified.
- For inpatient step-down, programs like inpatient drug rehabs in New Jersey should lay out a written transition.
Action Checklist for “30 Day Rehab Centers in New Jersey”
- Use official directories
- Search SAMHSA Treatment Locator.
- Confirm state licensure via the NJ Division of Mental Health and Addiction Services.
- Confirm license numbers
- Collect facility DMHAS license number(s), service types, and expiration date. Screenshot and save.
- Validate accreditation
- Check the Joint Commission Quality Check listing or CARF. Names and addresses must match.
- Request program schedule
- Daily/weekly structure with clinical hours and staffing coverage.
- Get the staff roster with credentials
- MD/DO (addiction medicine or psychiatry), LCSW/LCADC, RN. Verify via state licensure lookups when possible.
- Medication management policy
- Who prescribes, frequency of visits, after-hours coverage, diversion controls.
- MAT availability and philosophy
- Do they offer buprenorphine, methadone coordination, and naltrexone? Is MAT available at every level of care?
- Urine testing policy
- Frequency, confirmatory testing, who pays, and how results inform treatment.
- Family involvement rules
- Session frequency, consent procedures, boundaries, and educational content.
- Discharge plan template
- Obtain a blank template before admission. It should show appointments, medications, safety planning, and crisis contacts.
- Keep a paper trail
- Save emails, credential screenshots, benefit checks, cost estimates, and EOBs. Date-stamp everything.
- Rolling Hills Recovery Center has created a helpful rehab guide where readers can compare programs, learn about costs, and choose the right level of care with confidence.
Useful Resources
- SAMHSA Treatment Locator: https://findtreatment.gov
- NJ Division of Mental Health and Addiction Services (DMHAS): https://www.nj.gov/humanservices/dmhas/
- The Joint Commission quality check: https://www.qualitycheck.org
- National Institute on Drug Abuse: https://nida.nih.gov
- AA meeting finder: https://www.aa.org/find-aa
- NA meeting search: https://www.na.org/meetingsearch
Rolling Hills Recovery Center: Where it Fits
Rolling Hills Recovery Center is a New Jersey drug and alcohol rehab that lists evidence-based care and holistic adjuncts. Anchor to what’s verifiable:
- Confirm DMHAS licensure and service types (detox, residential, PHP, IOP).
- Confirm accreditation (The Joint Commission or CARF).
- Confirm MAT availability and scope (buprenorphine, naltrexone; methadone coordination if not on site).
- Request schedule, staff roster with credentials, and sample discharge plan.
- Ask for outcomes data: retention, follow-up linkage, MAT adherence, overdose education rates. If the program provides documentation and allows you to verify, it aligns with the standard outlined here.
How to Assemble Your 30-Day Plan (Step-by-Step)
- Step 1: Clinical fit
- Determine if detox is needed (alcohol, benzos, heavy opioids). If yes, prioritize an inpatient medical detox and immediate stabilization.
- Step 2: Stabilize and map step-down
- While in detox or days 1–3 of residential, schedule post-acute levels of care (PHP/IOP), psychiatry, and peer support contacts.
- Step 3: MAT decision
- Discuss buprenorphine/methadone/naltrexone or MAUD options. Decide before discharge; do not delay.
- Step 4: Family alignment
- Schedule at least one family session to set boundaries, educate on overdose response, and align home support.
- Step 5: Housing
- If home is unsafe or unstable, set recovery housing with rules that support your step-down level.
- Step 6: Safety and monitoring
- Naloxone in hand, crisis plan written, urine testing schedule understood, transportation arranged for first 2 weeks post-discharge.
- Step 7: Cost control
- Lock in in-network providers when possible, request written estimates, and confirm coverage for labs and medications.
Practical Tools and Templates
- Verification email template
- “Please provide: NJ DMHAS license number(s), accreditation body and certificate, staff roster with credentials, program schedule, MAT policy, urine testing policy, and a blank discharge plan template. Thank you.”
- EOB review checklist
- Service dates, CPT/HCPCS codes, allowed amount, plan payment, patient responsibility, and duplicates flagged.
- Discharge plan essentials
- Appointments: IOP start date/time; prescriber follow-up; therapy/psychiatry; primary care.
- Medications: dosages, refill dates, pharmacy.
- Safety: naloxone access, crisis numbers, triggers, and coping plan.
- Supports: first three peer meetings and locations (AA/NA or alternatives).
Where Holistic Approaches Fit (Without Overruling Evidence)
- Acceptable as adjuncts: mindfulness, yoga, nutrition, light fitness, and massage. These support sleep and stress management.
- Not replacements for CBT/MI/MAT.
- Ensure holistic services do not eat into clinical hours. If the weekly schedule shows more wellness than therapy, that’s a problem.
Detox Specifics to Verify in New Jersey
- Alcohol/benzodiazepine protocols
- Ask if CIWA is used for alcohol and if seizure precautions are standard; if phenobarbital or benzodiazepine tapers are available.
- Opioid withdrawal management
- Buprenorphine induction protocols, comfort meds, and transition into maintenance rather than detox-only.
- Medical coverage
- RN 24/7, daily MD/DO rounds, and on-call coverage documented.
Family Engagement That Works
- Clear participation schedule and rules.
- Education on enabling vs support.
- Agreement on post-discharge rules: curfews, testing, financial boundaries, and emergency plan.
- Consider supplemental family-focused services if needed to stabilize the home environment.
Metrics You Should Ask Any NJ 30-Day Program To Show You
- Percentage initiating MAT when indicated.
- 7-day and 30-day post-discharge appointment adherence.
- Readmission rate context (by diagnosis and severity).
- Patient-reported outcomes (e.g., cravings scales) pre-/post-stay.
- Completion rates by level of care.
If they collect nothing, expect nothing.
Conclusion
30‑day NJ rehab stabilizes, starts meds, sets structure; it won’t finish recovery. Verify licenses, schedule, staff, costs & aftercare. Track outcomes, not slogans. Contact Rolling Hills Recovery Center.
Frequently Asked Questions (FAQs)
What Does a 30-Day Rehab in New Jersey Actually Include?
A credible 30-day rehab in New Jersey should start with a medical and psychosocial assessment, then, only if medically necessary, detox with 24/7 nursing and physician oversight.
Expect a structured daily schedule: individual therapy (CBT or MI), small‑group sessions, family contact with boundaries, medication management (including MAT for OUD & AUD when indicated), relapse‑prevention skills, and discharge planning with booked follow‑ups. If detox isn’t needed, you enter residential/inpatient or a PHP/IOP level matched to your needs.
Do not accept vague answers. Ask for the written daily schedule, staff roster with credentials (MD/DO, LCSW, LCADC, RN), and the program’s urine‑testing and medication policies. For treatment basics, see the principles outlined by NIDA and verify licensed programs via NJ DMHAS. Accreditation can be checked at The Joint Commission Quality Check.
Is 30 Days Enough for Recovery in New Jersey?
Short answer: It’s a solid start, not a finish. A 30-day rehab in New Jersey can stabilize you, start the right meds, and build a routine. But outcomes improve as treatment time extends. NIDA notes treatment under 90 days is of limited effectiveness for most; longer engagement yields better results (NIDA). Plan step‑downs (IOP, outpatient, peer recovery), book appointments before discharge, and get overdose education plus naloxone.
Use the SAMHSA Treatment Locator to map nearby step‑down services and confirm they accept your insurance. No plan, no progress.
How Do I Verify a 30-day Rehab in New Jersey is Legitimate and Safe?
Three checks, no exceptions:
1. License: Confirm active NJ DMHAS licensure for the exact address and level of care (NJ DMHAS).
2. Accreditation: Verify The Joint Commission or CARF in public databases (Quality Check).
3. Clinician credentials: Ask for names and licenses; look for MD/DO with addiction medicine or psychiatry, LCSW, LCADC, RN. You can validate physician board certification via the American Board of Preventive Medicine.
Demand a written treatment plan with measurable goals in the first 72 hours. Red flags: vague promises, no schedule, no outcomes tracked, pressure to prepay without itemized costs.
What Will I Pay For a 30-Day Rehab in New Jersey with Insurance?
It depends on in‑network vs out‑of‑network, your deductible and co‑insurance, and what’s bundled vs billed separately (labs, meds, UAs, transport). Get a written Good Faith Estimate and an itemized “what’s included.” Ask if pre‑authorization is required and who obtains it. If you have NJ Medicaid (NJ FamilyCare), verify covered levels of care and any co‑pays (NJ FamilyCare). You also have mental health and substance use parity rights; if coverage is denied, see MHPAEA guidance from the U.S. Department of Labor (DOL Parity).
Bottom line: no numbers in writing = don’t proceed. Costs vary, of course, but your total exposure should be clear before admission.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












