Alcohol detox in New Jersey can be safe, effective, & compassionate when done with medical oversight. This overview explains who needs supervised detox, what symptoms to expect, when to go to the ER, and how care teams reduce risks with thiamine, monitoring, and proven medicines, plus what happens next with recovery planning & supportive therapies.
Key Takeaways
- Medical detox is the safest choice for daily heavy alcohol use, a past seizure or delirium tremens, pregnancy, age 60+, or significant heart, lung, or liver disease; do not quit suddenly at home
- Typical withdrawal looks like this: 6–24 hours tremor, anxiety, sweating; 24–48 hours higher pulse and seizure risk; 48–96 hours risk of delirium. Call 911 for severe confusion, repeated vomiting, chest pain, or a seizure
- In supervised care, teams use thiamine before glucose, CIWA-Ar scoring to titrate benzodiazepines, fluids & electrolytes, nutrition, anti-nausea meds, and sleep support, targeting safety without over-sedation
- Planning helps: confirm New Jersey licensure and insurance benefits, bring a current meds list, arrange a ride; begin relapse-prevention early with naltrexone, acamprosate, or disulfiram, plus therapy and peer supports
Scope and Urgency of New Jersey Alcohol Detox
Alcohol withdrawal can become a medical emergency. In New Jersey, timely, supervised detox is essential to reduce the risk of seizures, delirium tremens (DTs), falls, and metabolic complications.
Evidence-based protocols used across NJ align with consensus standards from ASAM, NIAAA, and NCBI resources; safer outcomes depend on early assessment, correct medications, and close monitoring.
Who often needs medically supervised alcohol detox:
- People drinking daily or near-daily who have morning shakes, sweats, or “eye-opener” drinks
- Anyone with prior alcohol withdrawal complications (seizures, hallucinations, or DTs)
- Heavy use with other sedatives (benzodiazepines, barbiturates), opioids, or stimulants
- Older adults, those with chronic liver disease, diabetes, heart disease, or head injury
- Pregnant patients with withdrawal risks of materno-fetal instability must be medically managed
- Individuals unable to maintain hydration or who live alone without reliable support
Typical withdrawal timeline (can vary by person, last drink, liver function, and co-use):
- 6–24 hours: Tremor, anxiety, nausea, insomnia, sweating, palpitations, mild hypertension
- 24–48 hours: Worsening tremor, vomiting, hallucinosis, alcohol withdrawal seizures may occur
- 48–96 hours: Delirium tremens (confusion, agitation, autonomic instability, fever), highest risk window
Red flags requiring immediate ED transport or 911:
- Seizure or fainting
- New confusion, disorientation, severe agitation, or hallucinations
- Repetitive vomiting or blood in vomit
- Chest pain, shortness of breath, fever >101°F, or oxygen saturation <92%
- Uncontrolled tremor, inability to keep fluids down, or signs of dehydration
- Heart rate >120 bpm or systolic BP >180 mmHg or <90 mmHg
- Severe headache, new weakness, or head injury after a fall
- Pregnancy with any moderate to severe withdrawal signs
Why supervised detox in NJ matters:
- Thiamine must be given before glucose to reduce the risk of Wernicke encephalopathy. Vitamin repletion is a standard of care, not optional.
- Baseline labs aid safety and dosing: CMP with electrolytes (including magnesium), glucose, renal function, liver panel, CBC, pregnancy test when relevant, blood alcohol level, urine toxicology; ECG when tachycardia, electrolyte issues, or cardiac history.
- CIWA‑Ar scoring helps titrate benzodiazepines to symptoms. Symptom-triggered dosing generally reduces over-sedation, medication use, and length of stay compared with fixed schedules, though fixed dosing is appropriate in specific situations.
- Co-occurring conditions require modified plans: pregnancy, polysubstance use, benzodiazepine dependence, chronic pain, liver impairment, and psychiatric comorbidity (e.g., depression with suicidality) change risk and medication choices.
- Ambulatory patients still need daily assessment, reliable transport, safe housing, and access to rapid escalation if symptoms worsen.
Consensus standards emphasize patient safety, frequent monitoring, and connection to ongoing care over “white-knuckling” through withdrawal at home.
Choosing the Right New Jersey Level of Care
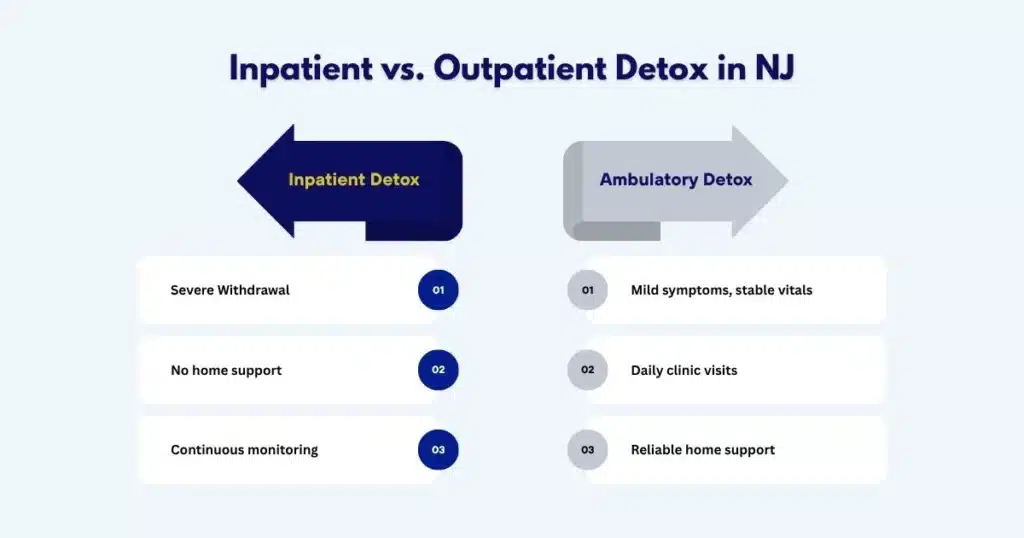
Inpatient vs Ambulatory Withdrawal Management (ASAM-Aligned)
Choosing the right setting centers on safety risks, supports at home, medical/psychiatric needs, and history of severe withdrawal. The ASAM Criteria are used statewide to make these determinations.
| Feature | Inpatient Withdrawal Management | Ambulatory (Outpatient) Withdrawal Management |
|---|---|---|
| Who it fits | History of severe withdrawal, seizures, DTs; significant medical/psychiatric comorbidity; pregnancy; polysubstance sedation; unstable vitals; no safe home supports | Mild-to-moderate withdrawal, reliable support person, stable vitals, no major comorbidity, able to attend daily visits |
| Monitoring | Continuous nursing, vitals every 2–4 hours, rapid response capability | Daily visits or more frequent check-ins, vitals checks, on-call escalation |
| Medications | Symptom-triggered benzodiazepines with IV/IM options; adjuncts as needed | Oral medications, symptom-triggered or fixed dosing under close supervision |
| Labs/Imaging | Rapid full workup on site | Labs drawn at intake and as clinically indicated |
| Advantages | Highest safety; rapid stabilization; easier hydration & nutrition support | Less disruption to home/work; lower cost; appropriate for lower risk patients |
When uncertainty exists, favor the higher level of care, especially if the person lives alone, has limited transportation, or a history suggesting complicated withdrawal.
For those seeking a licensed medical detox in New Jersey, learn about local, physician-led options through this resource: Medical detox near me.
Safety Screens that Suggest Higher Acuity
- Past withdrawal seizure(s) or delirium tremens
- Heavy use with benzodiazepines or other sedatives
- Unstable vitals (HR >120, SBP >180 or <90, temp >101°F), oxygen saturation <92%
- Acute medical conditions (GI bleed, pancreatitis, pneumonia, trauma, pregnancy complications)
- Liver disease with decompensation (jaundice, ascites, encephalopathy)
- Suicidality or psychosis
- Poor social support or inability to hydrate at home
Verifying NJ Licensure, Patient Rights, and Quality
- Confirm the facility is licensed or certified by the NJ Department of Human Services Division of Mental Health and Addiction Services (DMHAS). See consumer resources, complaint processes, and standards at the NJ DHS/DMHAS website.
- Ask to see patient rights documentation, informed consent forms, and privacy policies.
- Clarify after-hours medical coverage and how emergencies are handled.
- Confirm staff credentials (physician board certification in addiction medicine/psychiatry, nursing licenses, counselors with CADC/LADC). Check New Jersey licensure databases when in doubt.
Insurance Basics and Privacy
- Call your insurer for pre-authorization requirements. Ask about deductibles, copays, and any out-of-network benefits.
- Confirm whether the facility can submit authorizations and provide utilization review updates.
- HIPAA protects health information; ask how your data is used and stored. If you want family updates, sign releases in writing.
- For work or school leave, request documentation supporting a medical necessity detox stay, ideally prepared at admission.
Core Medications and Dosing Strategies
- Benzodiazepines are first-line: diazepam or lorazepam are commonly used. Diazepam has rapid CNS penetration and a long half-life; lorazepam is preferred when liver disease is present or in older adults due to more predictable metabolism.
- Symptom-triggered dosing uses CIWA‑Ar assessments to guide each dose. This often results in fewer total doses, less over-sedation, and shorter stays.
- Fixed-dose schedules may be used when CIWA‑Ar scoring isn’t feasible or when there’s significant benzodiazepine tolerance, with careful adjustments.
- Adjuncts:
- Gabapentin: supports anxiety/sleep and may reduce cravings; avoid when severe renal impairment.
- Clonidine: helps autonomic symptoms (tachycardia, hypertension); not a substitute for benzodiazepines.
- Antiemetics (ondansetron), antidiarrheals, acetaminophen for headache/fever; avoid NSAIDs if gastritis/bleeding risk.
- Antipsychotics (e.g., haloperidol) may be used short-term for severe agitation/hallucinations, with caution and ECG monitoring.
- Vitamin and electrolyte repletion:
- Thiamine IV or IM before any glucose-containing fluids; then oral thiamine daily.
- Folate and multivitamins.
- Magnesium and phosphate repletion as indicated.
- Fluids and nutrition:
- Oral rehydration when able; IV fluids if dehydrated or vomiting persists.
- High-protein snacks, complex carbs, and a gentle reintroduction of meals.
Rolling Hills Recovery Center uses evidence-based protocols in combination with holistic supports, nutrition, sleep hygiene, and stress-reduction to keep treatment safe and person-centered.
What to Expect During Detox
Admission and Day 1: Intake, Labs, and a Clear Plan
Typical steps, whether inpatient or ambulatory:
- Intake assessment: alcohol history (quantity, frequency, last drink), past withdrawal severity, prior treatments, medications, allergies, medical and psychiatric history, pregnancy status when applicable.
- Physical exam and safety checks: hydration status, signs of head injury, vitals, tremor assessment.
- Labs: CBC, CMP with electrolytes (including magnesium), LFTs, glucose, renal function, urinalysis; urine tox screen; blood alcohol level; pregnancy test; ECG when indicated.
- Thiamine before any glucose-containing fluids, then begin the vitamin regimen.
- CIWA‑Ar scoring is scheduled at regular intervals.
- Initial medication dosing based on symptoms, medical history, and risk.
Frequency of monitoring:
- Vitals at least every 2–4 hours early on; more often if symptoms are moderate to severe.
- Nursing checks for orientation, agitation, and hydration status.
- Daily medical rounds to adjust medications and address complications early.
Managing Symptoms: Hydration, Rest, and Right-Sized Sedation
- Hydration: Frequent sips of electrolyte solutions. IV fluids if oral intake is poor.
- Nausea/vomiting: Antiemetics relieve distress, help retain fluids and meds.
- Sleep: Non-benzodiazepine sleep strategies first; avoid over-sedation: dim lights, earplugs, structured sleep window.
- Anxiety and agitation: CIWA‑Ar–guided benzodiazepine dosing. Avoid stacking sedatives; use adjuncts cautiously.
- Pain and headache: Acetaminophen preferred unless there’s liver impairment, then dose carefully or choose alternatives.
- Nutrition: Small, regular meals; thiamine and multivitamins; magnesium as needed.
Harm-reduction steps embedded in detox:
- Education on overdose and interactions (e.g., never combine alcohol with sedatives).
- Safer-use counseling for patients not ready for abstinence, while still supporting recovery choices.
- Naloxone education if there’s any opioid co-use in the household.
Family involvement:
- With signed permission, families receive periodic updates and guidance on how to support recovery, manage boundaries, and recognize red flags. For structured family offerings in NJ, see our article New Jersey family support rehab.
Course and Complications: the First 3–7 Days

- Days 1–2: Most patients experience peak tremor, anxiety, and insomnia. Seizure risk rises through 48 hours.
- Days 2–4: DT risk window. Agitation, confusion, severe hypertension, and fever are monitored closely. Rapid escalation protocols are in place.
- Days 4–7: Symptoms taper; sleep normalizes; appetite improves. Begin relapse-prevention planning and therapy engagement in earnest.
Complications surveilled:
- Electrolyte disturbances (low magnesium, potassium, or phosphate)
- Dehydration and acute kidney injury
- Arrhythmias in vulnerable hearts
- Wernicke encephalopathy (confusion, ataxia, eye findings)
- Aspiration pneumonia, falls, or head injury
- Suicidal thinking—screen daily
Early discharge planning from day 1:
- Identify step-down level (residential, partial hospitalization, intensive outpatient, or standard outpatient).
- Start paperwork for insurance authorizations.
- Select relapse-prevention pharmacotherapy and schedule follow-up.
For patients stepping down to outpatient therapy after detox, explore local, flexible options at outpatient alcohol rehab centers in NJ.
Preparation and Aftercare
What to Pack and How to Arrive

- Personal ID, insurance card, medication list, and pharmacy info
- Names and contacts for primary care and mental health providers
- Comfortable, layered clothing; slip-on shoes; basic toiletries (fragrance-free if possible)
- Glasses, hearing aids, CPAP machine if applicable
- Phone charger and a short list of supportive contacts
- Leave paperwork: FMLA forms, employer letter templates, school notes, and a calendar with key obligations to reschedule
Transportation and logistics:
- Arrange a reliable ride both to and from detox; avoid driving yourself.
- Bring a list of emergency contacts and preferred hospitals.
Simple tools and templates to make it easier:
- Detox readiness checklist: last drink time, typical daily intake, prior withdrawals, medical conditions, meds, allergies, emergency contacts.
- Questions-to-ask template: licensure status, physician coverage, CIWA‑Ar use, thiamine protocol, average length of stay, visitor policy, aftercare planning.
- Wallet card with 911 red flags and local emergency numbers. Keep it visible.
Safety Planning for Ambulatory Detox
- Identify a support person who can stay with you overnight for at least the first 2–3 nights.
- Secure alcohol and sedatives in the home, or remove them entirely.
- Post vital thresholds for escalation (e.g., HR >120, SBP >180, severe confusion).
- Pre-arrange transportation to the clinic and to emergency care if required.
- Use a hydration plan (e.g., 8 oz electrolyte drink every hour while awake) and keep light snacks at bedside.
Stepping Into Ongoing Treatment After Detox
Medications for relapse prevention (FDA-approved):
- Naltrexone (oral daily or monthly injection): reduces heavy drinking days; check liver function and ensure no concurrent opioids.
- Acamprosate: supports abstinence; dose-adjust in renal impairment; taken three times daily.
- Disulfiram: aversive agent; must avoid any alcohol exposure; requires high motivation and monitoring.
Psychotherapies that work:
- Cognitive Behavioral Therapy (CBT) to change thinking patterns that drive drinking
- Motivational Interviewing to strengthen commitment and resolve ambivalence
- Trauma-informed therapies, when indicated, coordinate with mental health
Recovery supports that complement, not replace, clinical care:
- Mutual-help groups (AA, SMART Recovery, LifeRing), recovery coaching, and faith-based supports if desired
- Family education and boundary-setting workshops
- Wellness practices: sleep regularity, nutrition, exercise, mindfulness
Rolling Hills Recovery Center integrates evidence-based therapies with holistic supports, nutrition guidance, light movement, and stress management to build sustainable recovery after detox. Care plans are personalized, practical, and aligned with each person’s goals and their treatment for alcohol use disorder.
Legal and Local Considerations in New Jersey
Consumer Protections and Verifying Compliance
- Licensing and oversight: Detox and rehab programs in NJ operate under the NJ Department of Human Services, Division of Mental Health and Addiction Services (DMHAS). Consumers can review standards, file complaints, and find public information on facility status through DMHAS publications.
- Credential checks: Verify physicians through the NJ Board of Medical Examiners; nurses via the NJ Board of Nursing; counselors via the NJ Division of Consumer Affairs (CADC/LADC). National Provider Identifier (NPI) records can add transparency.
- Patient rights: Ask for a written copy covering informed consent, grievance processes, visitation, privacy, and discharge planning. Confirm translation services if needed.
When to Call 911 in NJ
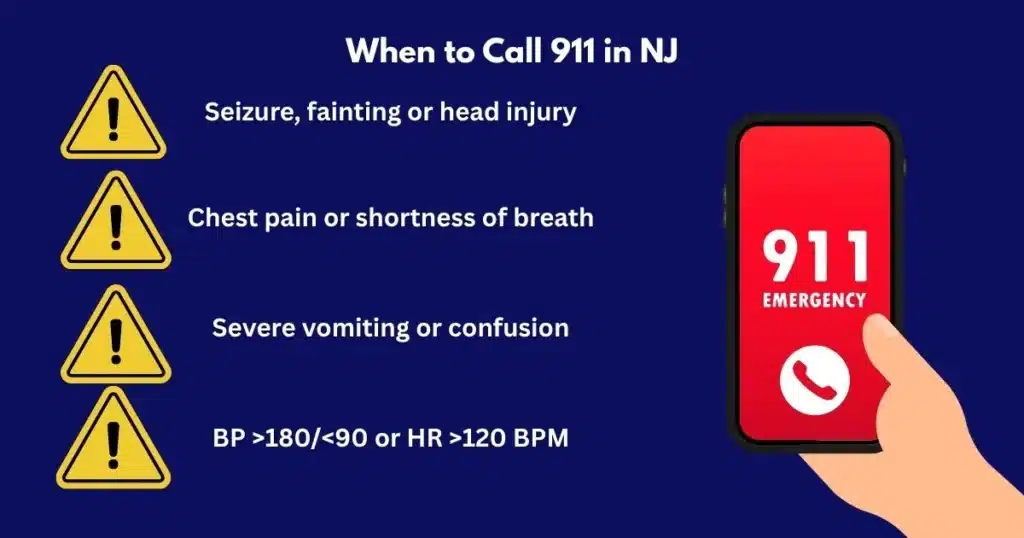
Call immediately if any of the following occur during detox:
- Seizure, loss of consciousness, or severe head injury from a fall
- Confusion, hallucinations, or extreme agitation
- Severe chest pain, breathing difficulty, oxygen saturation <92%
- Repetitive vomiting, signs of dehydration (minimal urine, dizziness), fever >101°F
- Blood pressure emergencies: SBP >180 or <90; HR >120 that doesn’t respond to rest
- Pregnant individuals with moderate to severe symptoms
If unsure, err on the side of calling; paramedics can assess and transport safely.
Confidentiality and Documentation
- HIPAA protections apply; release of information requires your written consent. Shared information is typically limited to what is necessary for your care or as required by law.
- Work or school notes: Ask at admission for expected length of stay and any activity restrictions. Facilities can provide return-to-work or school documentation that protects privacy while certifying medical need.
- Legal issues: If detox intersects with court obligations or probation, coordinate documentation early to avoid missed appearances. Obtain signed releases as needed.
Step-by-Step: Getting Started with New Jersey Alcohol Detox Today
- Decide on setting using safety cues:
- Any prior seizure, DTs, or unstable vitals? Choose inpatient.
- Stable vitals, mild to moderate symptoms, and a safe home with support? Consider ambulatory with daily monitoring.
- Verify licensing and coverage:
- Confirm NJ DMHAS-recognized status and staff credentials.
- Call your insurer, confirm pre-authorization, and costs.
- Prepare for admission:
- Pack essentials, list medications & allergies, line up a ride.
- Write last drink time and average intake; bring prior medical records if available.
- On arrival:
- Expect labs, vitals, CIWA‑Ar setup, and thiamine administration.
- Review the plan for symptom-triggered versus fixed-dose benzodiazepines; ask about adjuncts and vitamins.
- Monitor and adjust:
- Vitals every 2–4 hours in the early phase. Report any worsening.
- Hydrate, eat small meals, practice sleep hygiene, and accept help.
- Begin aftercare planning now:
- Discuss naltrexone, acamprosate, or disulfiram.
- Schedule therapy and support groups; plan transportation and childcare.
- Confirm follow-up:
- Book appointments before discharge (primary care, medication management, therapy).
- Plan a safety check-in with a trusted support the first week home.
Quick Decision-Check Template
- Medical red flags present (seizure history, DTs, unstable vitals, pregnancy)? If yes → inpatient.
- Safe, sober supports at home for 3–4 nights? If no → consider inpatient or residential.
- Able to attend daily clinic visits and call for help if symptoms worsen? If no → higher level of care.
- Insurance verified and transportation arranged? If no → resolve before starting.
Keep it simple: Safety first, no guesswork.
Helpful References
- ASAM: Alcohol Withdrawal Management (levels of care, dosing strategies, CIWA‑Ar use)
- NIAAA Core Resource on Alcohol (assessment and treatment basics)
- NCBI Bookshelf: Alcohol Withdrawal Syndrome (pathophysiology and CIWA‑Ar context)
- FDA: Medications for Alcohol Dependence (approved meds and safety)
- NJ Department of Human Services, Division of Mental Health and Addiction Services (state standards, consumer rights)
Conclusion
Detox in New Jersey works best with safe, supervised care. Key points: know red flags, choose the right setting, start relapse prevention, and aftercare early. Next steps: ask questions, verify benefits, arrange a ride, and pack the basics.
Frequently Asked Questions (FAQs)
Who Should Consider New Jersey Alcohol Detox with Medical Supervision?
People at higher risk benefit most from supervised New Jersey alcohol detox. This includes those who drink heavily daily, have a past seizure or delirium tremens, are pregnant, are 60+, or live with heart, lung, or liver disease.
Also at risk: polysubstance use (alcohol plus benzodiazepines or opioids), history of severe withdrawal, very high blood pressure, or limited support at home.
Medical oversight helps manage symptoms, prevents complications, and supports safer hydration & nutrition during the first critical days.
What Symptoms and Timeline are Common in Alcohol Detox?
In alcohol detox, mild symptoms often start 6–12 hours after the last drink: tremor, anxiety, sweating, nausea & poor sleep.
Moderate symptoms can appear by 12–48 hours: high pulse, high blood pressure, vomiting, marked tremor, and sometimes seizures.
Severe symptoms such as confusion, hallucinations, or delirium tremens tend to peak at 48–96 hours. Most stabilize by day 3–5. If symptoms escalate fast or feel “out of control”… urgent evaluation is advised.
Is Alcohol Detox Covered by Insurance, and How Should Someone Prepare?
Many plans cover New Jersey alcohol detox when it is medically necessary. Steps that help:
Call the member services number to confirm detox benefits and any preauthorization
Have photo ID, insurance card, and a list of medications and allergies
Arrange a safe ride; do not drive yourself
Pack light: comfy clothes, phone charger, essential toiletries
Share recent medical records if available (heart, liver, or seizure history)
Secure home responsibilities (work note, pet care), it eases stress and improves follow‑through
If coverage is unclear, ask for a benefits check and an estimate of out-of-pocket costs before admission.
When is Emergency Care Needed During Alcohol Detox?
During alcohol detox, call 911 or go to the ER for any of the following:
Seizure, severe confusion, or agitation that won’t settle
Fever, chest pain, trouble breathing, fainting
Uncontrolled vomiting, blood in vomit or stools
Hallucinations, very high blood pressure, or a heart rate above 120 at rest
Worsening symptoms despite taking prescribed meds
If unsure, err on the side of safety. Rapid treatment lowers the risk of serious harm.
Author
-

Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -

Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts











