Searching for “medical detox near me” often means withdrawal has started or safety is a concern. This overview explains when medically supervised detox is necessary, what happens day to day, and how to prepare. It outlines risks, timelines, medications & monitoring, insurance and costs, and the next steps that support long‑term recovery for adults and families.
Key Takeaways
- Choose medical detox for alcohol, benzodiazepines, opioids, or polysubstance use; call 911 for seizures, severe confusion, chest pain & trouble breathing, high fever, or pregnancy concerns.
- Expect licensed care with 24/7 nursing and physician oversight, frequent vitals, CIWA‑Ar or COWS scoring, comfort medicines, and FDA‑approved options like buprenorphine or methadone; timelines differ by substance.
- Check quality and safety: state licensure, Joint Commission accreditation, on‑site MAT, plans for co‑occurring mental health, suicide risk, clear costs and insurance verification; ask for a warm handoff to continuing care, no surprises.
- Prepare the basics: bring ID and a current medication list, arrange work leave & child care, plan transport; day to day includes hydration, nutrition, sleep support, brief counseling, and naloxone education when needed.
- Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches. Our team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
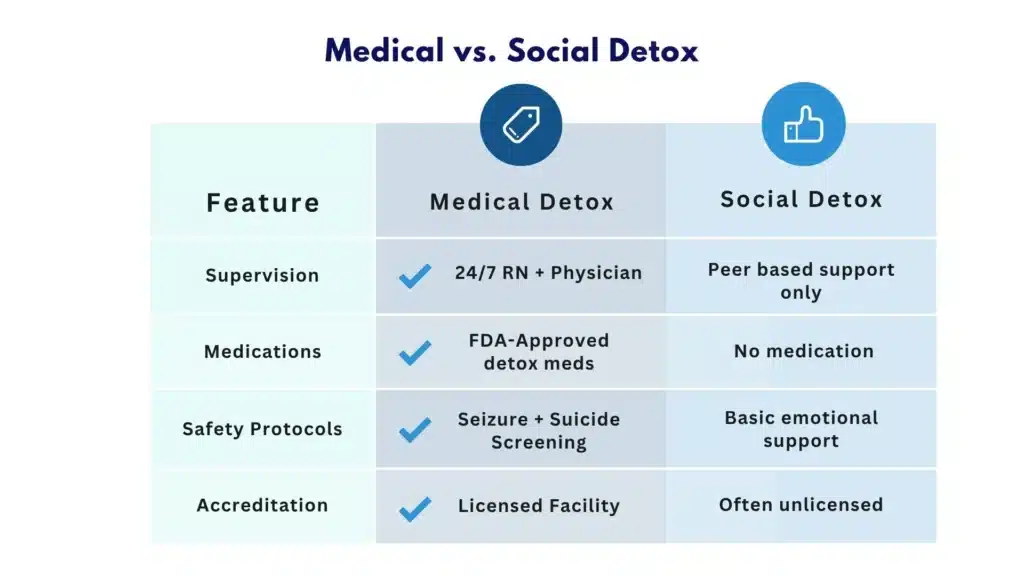
Defining “Medical Detox Near Me”: What it is vs Social Detox
Finding “medical detox near me” usually means looking for a licensed setting where withdrawal is managed with clinical monitoring, evidence-based medications, and supportive care around the clock. This differs from “social detox” (sometimes called non-medical or clinically managed withdrawal), where supportive counseling and monitoring occur without 24/7 nursing oversight or routine physician-directed medication.
Medical detox is recommended when withdrawal may be medically dangerous, or when symptoms are severe enough to derail recovery before it begins. It also serves as the on-ramp to ongoing treatment, stabilizing the body, reducing risk, and preparing for the next level of care.
Who Needs Medical Detox?
Medical detox is commonly indicated for:
- Alcohol use disorder: Risk of seizures and delirium tremens increases after heavy, sustained use.
- Benzodiazepine use disorder (e.g., alprazolam, clonazepam): Abrupt cessation can trigger seizures, agitation, and rebound anxiety.
- Opioid use disorder (e.g., heroin, fentanyl, oxycodone): While opioid withdrawal is rarely life-threatening, it can be extremely uncomfortable and high-risk for relapse; medications can stabilize quickly.
- Polysubstance use: Mixed substances (e.g., alcohol plus benzodiazepines; stimulants plus opioids) complicate withdrawal trajectories and require tailored protocols.
- High medical or psychiatric comorbidity: Chronic illnesses (e.g., COPD, diabetes), pregnancy, or serious mental health conditions (e.g., suicidality, psychosis) increase risk and complexity.
Red‑Flag Symptoms That Require Urgent Care (Call 911)
- Seizure, fainting, or unresponsiveness
- Severe confusion, agitation, or hallucinations
- Fever, chest pain, shortness of breath, or very high blood pressure
- Uncontrolled vomiting or diarrhea with signs of dehydration
- Thoughts of self-harm or harm to others
- Alcohol withdrawal with tremors progressing to confusion, or any history of withdrawal seizures
These symptoms warrant emergency evaluation, not a routine clinic visit.
Why Medically Supervised Withdrawal Reduces Complications and Prepares for Ongoing Treatment
- Active monitoring catches complications early (e.g., rising blood pressure, arrhythmias, severe agitation).
- FDA-approved medications for alcohol and opioid withdrawal reduce symptom burden, stabilize physiology, and lower the risk of early relapse.
- Structured assessments improve dosing precision and safety.
- Case management and discharge planning create a warm handoff to residential or outpatient care, improving engagement after detox.
- Trauma-informed, private care environments reduce distress, improve trust, and support attachment to treatment.
For individuals who feel ready to stop but can’t do it safely alone, practical supports and a safer medical pathway are available.
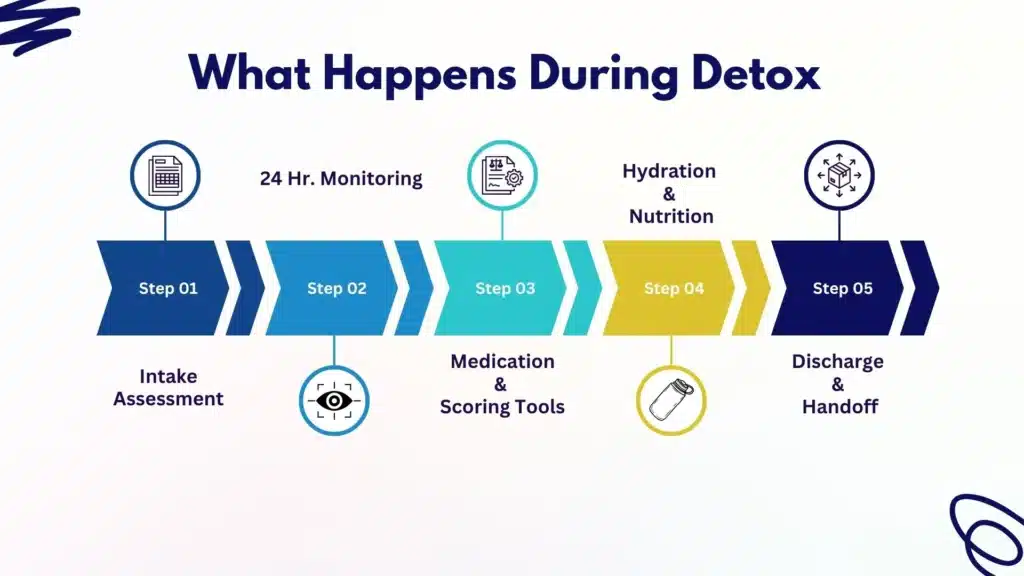
What Happens in Detox
Intake Assessment
A standard intake typically includes:
- Medical and psychiatric history, including past withdrawal severity and seizure history
- Substance use timeline (what, how much, how often, and last use)
- Physical exam and vital signs
- Urine drug screen and pregnancy test when relevant
- Baseline labs (e.g., CBC, CMP, liver enzymes, glucose, electrolytes; sometimes ECG)
- Medication reconciliation and allergy review
- Suicide risk and safety screening
This data drives individualized protocols.
Monitoring Tools Clinicians Use
- Alcohol withdrawal: CIWA‑Ar (Clinical Institute Withdrawal Assessment for Alcohol, revised). Scores guide benzodiazepine dosing and frequency.
- Opioid withdrawal: COWS (Clinical Opiate Withdrawal Scale). Scores inform when to start buprenorphine or adjust methadone.
- Other structured tools: PAWSS (Prediction of Alcohol Withdrawal Severity Scale), sedation scales, and vitals trending to adjust treatment in real time.
24/7 Nursing Oversight and Physician Coverage
- Registered nurses check vitals regularly (often every 2–4 hours early on), administer medications, and watch for complications.
- Physicians or advanced practice providers round daily, adjust protocols, and address co-occurring medical issues.
- Escalation pathways exist for seizures, delirium tremens, severe hypertension, or suicidal ideation.
Comfort Meds vs FDA‑Approved Medications
- Opioids
-
- FDA-approved for opioid use disorder: buprenorphine (Suboxone, Subutex formulations), methadone, and naltrexone (after full detox).
-
- Buprenorphine and methadone reduce withdrawal and cravings; induction timing is critical to prevent precipitated withdrawal.
-
- Adjuncts: clonidine or lofexidine for autonomic symptoms; antiemetics; antidiarrheals; NSAIDs; sleep aids.
-
- Common misconceptions about Suboxone are clarified here: Can you get high on Suboxone?
-
- Alcohol
-
- First-line: benzodiazepines (e.g., diazepam, lorazepam) using symptom-triggered or fixed-dose schedules.
-
- Thiamine and folate to prevent Wernicke–Korsakoff; fluids and electrolytes as needed.
-
- Adjuncts: gabapentin, carbamazepine, beta-blockers, or alpha-2 agonists for specific symptoms when appropriate.
-
- Post-detox relapse prevention may include naltrexone, acamprosate, or disulfiram based on individual needs.
-
- Benzodiazepines
-
- Gradual taper (often using a longer-acting agent like diazepam) to minimize seizure risk; pace depends on history and risk factors.
-
- Stimulants (e.g., cocaine, methamphetamine)
-
- No FDA-approved withdrawal medication. Focus on sleep restoration, anxiety/depression support, nutrition, hydration, and close monitoring for suicidality or severe agitation. Some centers use off-label agents for symptom relief when clinically indicated.
-
Typical Timelines by Substance and Risk Overview
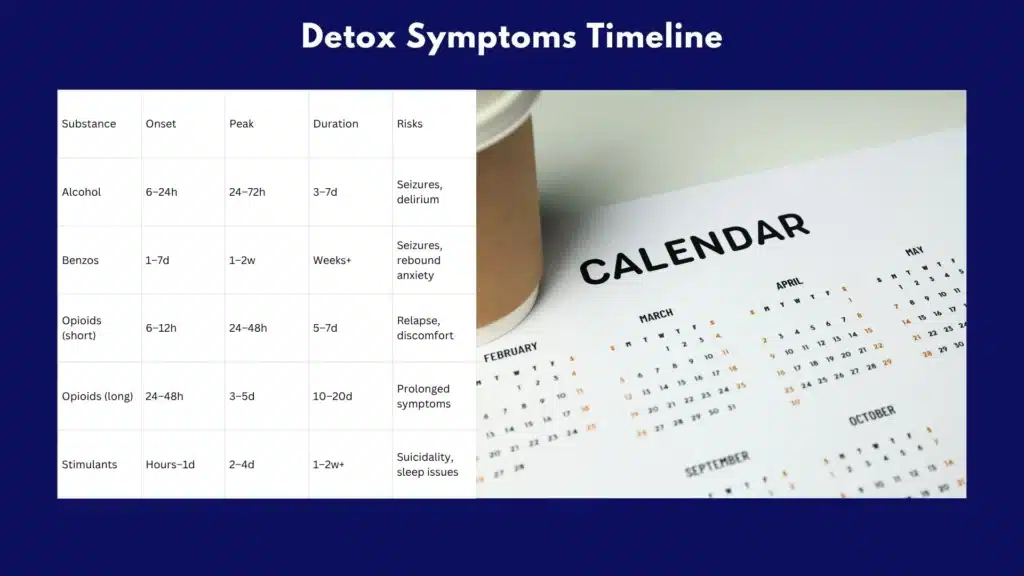
Detox timelines vary by dose, duration, co-occurring conditions, and polysubstance use. They are general expectations, not guarantees.
| Substance | Onset of Withdrawal | Peak Symptoms | Typical Duration | Key Risks |
|---|---|---|---|---|
| Alcohol | 6–24 hours after last drink | 24–72 hours | 3–7 days | Seizures (12–48h), delirium tremens (48–96h) |
| Benzodiazepines | 1–7 days (shorter if short-acting) | 1–2 weeks | Weeks-months taper | Seizures, rebound anxiety, insomnia |
| Short-Acting Opioids (Heroin) | 6–12 hours | 24–48 hours | 5–7 days | Dehydration, relapse due to severe symptoms |
| Long-Acting Opioids (Methadone) | 24–48 hours | 3–5 days | 10–20+ days | Prolonged discomfort, relapse risk |
| Stimulants | Hours–1 day | 2–4 days (crash phase) | 1–2 weeks+ | Severe depression, suicidality, sleep disruption |
Alcohol and benzodiazepines carry the highest risk of seizures and delirium; these should always be managed medically.
Trauma‑Informed Care and Privacy
- Staff seek consent and explain each step before acting; autonomy is respected.
- Gentle, nonjudgmental communication reduces stress and helps manage symptoms.
- Private rooms or quiet spaces, gender-sensitive options, and confidentiality protections help people feel safe.

How to Evaluate Local Options
When an online search for “medical detox near me” turns up mixed results, lean on universal safety checkpoints and clear, verifiable standards.
Verify Licensure and Accreditation
- Confirm the program holds state licensure for the level of care offered.
- Ask if the facility is accredited by The Joint Commission or CARF. Accreditation indicates third‑party review of quality and safety.
Ask About Staffing, Ratios, and Coverage
- Are RNs on-site 24/7? What is the nurse-to-patient ratio on busy shifts?
- How often do licensed providers round, and is there on-call physician coverage at all times?
- What is the minimum observation frequency for CIWA‑Ar/COWS monitoring?
On‑Site MAT and Medication Protocols
- Can the facility start buprenorphine or methadone on-site for opioid use disorder? How do they prevent precipitated withdrawal?
- Do they use symptom-triggered benzodiazepine protocols for alcohol withdrawal?
- Are thiamine and folate standard for alcohol detox?
- What is the approach to benzodiazepine tapers?
- How are stimulants managed, including suicidality screening and sleep support?
Co‑Occurring Disorders and Suicide Risk Management
- Does the team include psychiatric providers? How are antidepressants, mood stabilizers, or ADHD medications coordinated?
- What is the pathway if a patient endorses suicidal thoughts during detox?
- Are there protocols for trauma, PTSD, or psychosis?
- For patients with ADHD, ask how they coordinate care to reduce relapse risk.
Infection Control and Family Updates
- Ask about infection prevention measures, isolation protocols when needed, and vaccination support if relevant (e.g., hepatitis A/B).
- Clarify how and when family or supporters receive updates, with consent.
Insurance Verification and Transparent Costs
- Will the center verify benefits before admission?
- What out-of-pocket costs should be expected? Are medications and labs included?
- If out-of-network, ask for a written estimate and options for payment plans.
Safe Handoff to the Next Level of Care
- How does the program coordinate transition to residential, partial hospitalization, intensive outpatient, or outpatient MAT?
- Is there a written discharge plan with medications in hand, scheduled appointments, and warm transfer?
- Does the facility provide naloxone and training at discharge for people with opioid use disorder?
Rolling Hills Recovery Center in New Jersey emphasizes evidence-based care, integrated mental health support, and warm handoffs to keep momentum after detox, whether stepping into residential or outpatient services that match clinical needs.
What to Expect Day to Day
Hydration, Nutrition, and Sleep Support
- Hydration with fluids and electrolytes is routine; IV fluids if clinically needed.
- Small, frequent meals to manage nausea and stabilize blood sugar.
- Sleep is often disrupted early; non-addictive sleep strategies and medications are used when appropriate.
Vital Signs and Monitoring
- Frequent vitals (every few hours early) to watch blood pressure, pulse, temperature, and oxygen saturation.
- CIWA‑Ar/COWS scoring is tied to medication dosing.
- Ongoing safety checks, especially at night and during peak risk windows.
Managing Cravings and Discomfort
- Timely dosing of comfort medications reduces muscle aches, nausea, diarrhea, sweating, chills, and restlessness.
- Craving management includes medication (e.g., buprenorphine, methadone, naltrexone for OUD; anti-craving meds post-alcohol detox), coping skills, and environmental support (quiet spaces, hydration, nutrition).
- Gentle movement, breathing exercises, and brief mindfulness practices are often encouraged as simple, pragmatic tools.
Brief Counseling, Case Management, and Education
- Short educational sessions cover what to expect physically, how medications work, and relapse prevention basics.
- Case managers assess housing, transportation, and benefits, and then coordinate the next level of care.
- Family involvement is offered with consent, focusing on safety, expectations, and support.
Discharge Planning, Warm Transfer, Transportation, and Harm Reduction
- Written discharge instructions summarize medications, dosing, side effects, and warning signs requiring urgent care.
- Follow-up appointments are scheduled before discharge; the receiving program is contacted directly for a warm transfer.
- Transportation help is arranged when needed to avoid gaps in care.
- Harm reduction supplies, including naloxone for opioid overdose reversal, are provided when indicated. See CDC’s naloxone information at https://www.cdc.gov/stop-overdose/caring/naloxone.html?CDC_AAref_Val=https://www.cdc.gov/stopoverdose/naloxone/index.html
Practical Prep and Next Steps
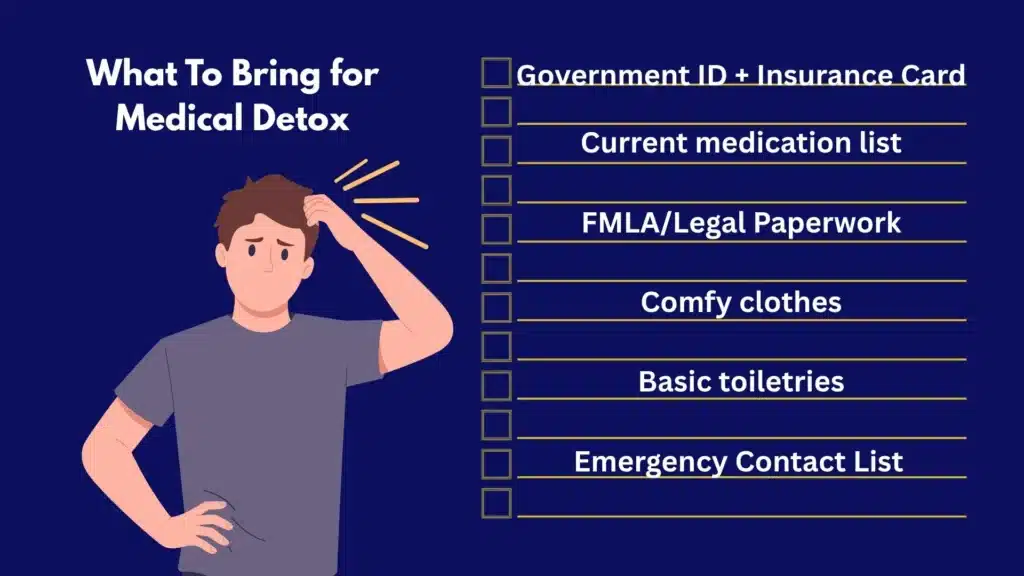
What to Bring
- Government ID and insurance card
- List of current medications, doses, and prescriber information
- Names and phone numbers for emergency contact(s) and primary care or specialists
- Comfortable clothing, simple toiletries (non-alcohol-based where possible), and a phone charger
- Glasses, hearing aids, or mobility devices, if used
- Legal documents or FMLA paperwork if employment leave is needed
Template: Medication list
- Medication name
- Dose and how often
- Purpose
- Prescriber name and phone
- Last dose taken, date/time
- Allergies
What Not to Bring
- Alcohol, drugs, vape devices (if not allowed), or paraphernalia
- Weapons, large amounts of cash, or valuables
- Unapproved supplements or herbal products
- Opened liquids or perishable food
- Smart devices that record audio/video (check program rules)
Arranging Leave From Work and Child Care
- Ask a clinician for a treatment letter supporting medical leave; FMLA may apply for eligible employees.
- Identify a backup caregiver for children or dependents for at least 5–7 days; plan for a longer window if benzodiazepine or methadone tapers are expected.
- Secure pet care and any necessary medication arrangements.
Insurance Benefits Confirmation
- Call the number on your insurance card and ask:
-
- Is medical detox covered under my plan? Is pre-authorization required?
-
- Which facilities in my area are in-network for detox?
-
- What are my deductible, co-pay, and out-of-pocket maximums?
-
- Are medications (e.g., buprenorphine, methadone) covered during and after detox?
-
- Request a reference number for the call and note the representative’s name.
Quick script:
- “I’m seeking information about coverage for medically supervised withdrawal management. Can you verify in-network facilities, pre-authorization needs, and my expected out-of-pocket costs? Please provide a call reference number.”
Questions to Ask on the First Call to a Detox Program
- Admission
-
- How soon can an assessment occur? Do you accept walk-ins or only appointments?
-
- What labs and screenings are required before admission?
-
- Safety and staffing
-
- Are RNs on site 24/7? What are staffing ratios?
-
- How often are vitals and CIWA‑Ar/COWS scores obtained?
-
- Who prescribes medications on nights and weekends?
-
- Medications
-
- Can you start buprenorphine or methadone? Do you offer naltrexone after detox?
-
- What is your benzodiazepine protocol for alcohol and benzo withdrawal?
-
- Co-occurring care
-
- Can psychiatric medications be started or continued during detox?
-
- How do you handle severe anxiety, depression, ADHD, or trauma symptoms?
-
- Discharge and aftercare
-
- How do you coordinate the next level of care? Do you schedule follow-up before discharge?
-
- Will I leave with medications in hand and naloxone if I have opioid use disorder?
-
- Logistics and costs
-
- What is the expected length of stay for my substances?
-
- Can you verify my insurance and provide a cost estimate?
-
“For individuals with moderate to severe substance misuse, medical detox is a necessity, not an option.
For certain substances, like alcohol and benzodiazepines, major health, even fatal, consequences could arise from abruptly stopping use on your own.
With opiate use, withdrawal can be so incredibly painful, thus precipitating the cycle of relapse. In either case, medical detox begins the process of clearing toxins out of the body, safely and more comfortably.”
Laura Riley, LCADC | Clinical Director at Rolling Hills Recovery Center
Contingency Plan if Symptoms Escalate Before Admission
- If severe confusion, seizures, hallucinations, chest pain, fever, or uncontrolled vomiting occur, call 911 immediately.
- If heavy alcohol or benzodiazepine use is ongoing and stopping abruptly feels unsafe, request emergency evaluation rather than waiting at home.
- Tell the emergency team exactly what and when substances were used; bring medication lists and any prior discharge paperwork.
Evidence Resources to Share with Loved Ones
- NIDA DrugFacts on treatment approaches: https://nida.nih.gov/publications/drugfacts/treatment-approaches-drug-addiction
- NIAAA overview of alcohol use disorder: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder
- ASAM Levels of Care (what each level means): https://www.asam.org/asam-criteria/about
These resources can help families understand why detox is just the first step and how ongoing care supports lasting change.
Helpful Tools and Simple Templates
- Withdrawal tracking
-
- Record time since last use, symptoms (0–10 scale), fluids taken, and any medications used before arrival. This helps clinicians.
-
- Packing checklist
-
- ID, insurance card, meds list, contacts, clothes, toiletries, charger, glasses/hearing aids, and necessary paperwork.
-
- Phone script for family
-
- “We’re seeking a safe medical detox with 24/7 nursing and physician coverage. Does your program provide on-site MAT, use CIWA‑Ar/COWS, and coordinate a warm handoff to ongoing care? Can you verify insurance today and give us the expected length of stay and costs?”
-
- Safety contacts sheet
-
- One emergency contact and one transportation backup. Include phone numbers and availability.
-
How Rolling Hills Recovery Center Fits Into Next Steps
- Emphasis on evidence-based care and holistic supports helps maintain gains from detox.
- Coordination with local detox programs allows for timely warm transfers into residential or outpatient services tailored to clinical needs.
- Education and family involvement aim to reduce relapse risk and improve continuity.
Conclusion
Medical detox works best when it’s timely, safe, and linked to follow-up care. Remember: recognize urgent symptoms, expect 24/7 monitoring with appropriate meds, and verify licensure & insurance.
Next steps: call, confirm benefits, arrange transport. Ready to begin?
Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches, and our team helps people overcome substance abuse and achieve lasting results.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












