Drug addiction can creep in quietly, blurring the line between needed treatment and harmful use. This overview explains what it is, common red flags, and safe steps toward recovery in New Jersey. Expect clear options for detox, medications, therapy, family support, and relapse prevention, with practical tools & safety tips patients can use.
Key Takeaways
- Medication care comes first: assess current prescriptions, check for tolerance or early refills, use DSM-5 SUD criteria, and review New Jersey’s PDMP (NJPMP). Screen for pain, anxiety, or sleep issues that may complicate recovery.
- Never stop benzodiazepines suddenly; taper slowly over weeks to months. Opioid use disorder can be treated with buprenorphine, methadone, or extended‑release naltrexone; add comfort meds like clonidine and hydroxyzine. Keep naloxone at home, coordinate all prescribers.
- Therapy and family matter: CBT, Motivational Interviewing, and Contingency Management support change. Include family sessions, CBT‑I for insomnia, trauma‑informed care, simple daily routines, plus secure storage & safe disposal of meds.
- Aftercare & safety: continue MAT & therapy, use non‑punitive urine testing, step down levels of care, and keep a clear return‑to‑use plan. Add regular check‑ins and driving precautions during early stabilization… small habits help.
Assessment and Diagnosis
Addiction Versus Physiological Dependence
Drug addiction is a pattern of compulsive use causing harm, loss of control, and continued use despite problems. Physiological dependence means the body adapts to a medication; if it stops suddenly, withdrawal occurs. Dependence can happen even with correct use.
Addiction includes behaviors like craving, escalating use, and using for reasons beyond a medical plan. For a fuller explanation of this distinction, see the difference between drug dependence and drug addiction.
At Rolling Hills Recovery Center in New Jersey, assessment separates expected physical dependence from a substance use disorder (SUD). This helps avoid undertreating pain or anxiety while still addressing risky use.
Main Prescription Drug Classes Involved
Most prescription-related SUD involves three groups:
- Opioids (e.g., oxycodone, hydrocodone, morphine, fentanyl)
- Benzodiazepines (e.g., alprazolam, clonazepam, lorazepam)
- Stimulants (e.g., amphetamine, methylphenidate)
Other medicines can also be misused (gabapentin, pregabalin, sedative-hypnotics), though less commonly.
Red Flags That Prompt Evaluation
Clinical red flags that suggest addiction rather than expected medical use:
- Tolerance (needing more for the same effect)
- Loss of control (taking more or longer than intended)
- Doctor shopping, early refill requests, or lost prescriptions
- Using a medication for reasons other than prescribed (e.g., to relax, sleep, improve mood)
- Withdrawal problems between doses
- Neglecting responsibilities, high-risk behavior (e.g., driving sedated), or legal issues
- Mixing medications or alcohol against medical advice
- Persistent use despite worsening health, relationships, or work
DSM‑5 SUD Criteria: How Diagnosis is Made
Diagnosis follows DSM‑5 criteria for SUD (mild, moderate, severe) based on 11 symptoms across impaired control, social impairment, risky use, and pharmacologic signs (tolerance/withdrawal).
The presence of tolerance or withdrawal alone, when a medication is taken as prescribed, does not equal SUD. Function, safety, and intent guide rating and treatment planning.
Screening Tools and Practical Steps
A structured approach improves accuracy and safety:
- Use brief screens:
- DAST‑10 for non-alcohol drug use
- Single-item questions (e.g., “How many times in the past year have you used an illegal drug or used a prescription medication for nonmedical reasons?”)
- Review the New Jersey Prescription Monitoring Program (NJPMP) to confirm controlled prescription history, doses, and prescribers.
- Medication reconciliation: list all prescriptions, over-the-counter products, supplements, and CBD. Verify dosing, indication, and duration.
- Identify co-occurring conditions: chronic pain, anxiety, trauma/PTSD, ADHD, insomnia, and depression. Consider withdrawal mimics (e.g., rebound insomnia from short-acting sedatives, opioid-induced hyperalgesia).
- Baseline safety checks: suicide risk screening, overdose risk (high opioid dose, concurrent benzodiazepines, respiratory disease), pregnancy status, and driving or safety-sensitive work.
- Lab tests when indicated: urine drug screen for clinical care, not punishment; liver and kidney function; pregnancy test; EKG if QT risk (methadone or other QT-prolonging meds).
- Assess social determinants: housing, food, transportation, childcare, and legal issues. These factors affect treatment adherence and must be part of planning.
Evidence resources on risks and scope of prescription opioid use are available from NIDA: NIDA, Prescription Opioids.
Documenting a Clear Working Diagnosis
Clinicians document:
- Substance type(s), pattern, dose equivalents, and route
- DSM‑5 severity
- Co-occurring psychiatric and medical conditions
- Medications that increase risk (e.g., benzodiazepine + opioid)
- Readiness for change (Motivational Interviewing staging)
- Patient goals (pain relief, sleep, school/work function) to align treatment with what matters
Medical Detox and Medications
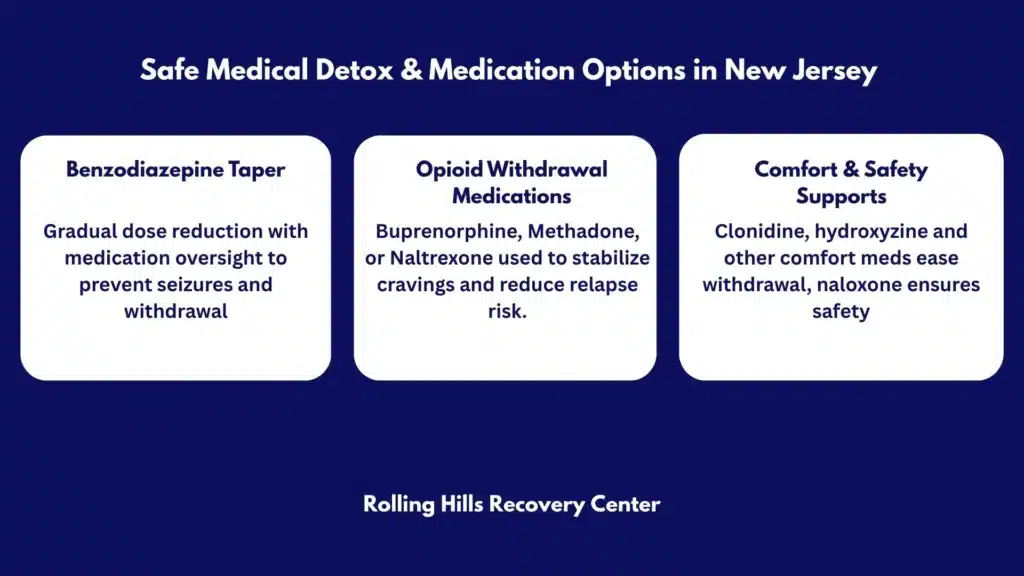
Benzodiazepine Tapers: Safe and Slow
Abrupt benzodiazepine discontinuation can cause seizures and severe withdrawal symptoms. A personalized taper is safer:
- Convert shorter-acting agents to longer-acting equivalents as needed (e.g., diazepam or clonazepam).
- Reduce the total daily dose by 5–10% every 2–4 weeks; pace can slow to monthly or longer at lower doses.
- Monitor for rebound anxiety, insomnia, tremor, and blood pressure changes.
- Non-benzodiazepine supports: CBT for anxiety and panic, CBT‑I for insomnia, SSRIs/SNRIs for anxiety disorders when indicated, hydroxyzine for short-term anxiety, and melatonin for sleep.
- Avoid concurrent alcohol, opioids, and other sedatives during taper.
- For long-term, high-dose use or seizure history, consider inpatient medical detox.
Practical tip:
- Create a written taper calendar with weekly dose targets.
- Offer a pill organizer and medication log to track actual use vs plan.
Opioid Withdrawal Management
Opioid withdrawal symptoms are uncomfortable but treatable. It is not life-threatening by itself, yet it raises relapse and overdose risk.
- Buprenorphine: partial agonist that relieves withdrawal and cravings; can start after moderate withdrawal begins (Clinical Opiate Withdrawal Scale, COWS ≥ 8–12). Micro-dosing (low-dose induction) allows overlap with full agonists to reduce discomfort.
- Methadone: full agonist started in certified programs; good for high tolerance, chronic pain, and when buprenorphine is not a fit.
- Extended-release naltrexone: opioid antagonist; start only after 7–10 days opioid-free. Best for highly motivated patients who prefer non-agonist therapy and have stable support.
- Symptom relief: clonidine (or lofexidine) for autonomic symptoms, NSAIDs or acetaminophen for aches, loperamide for diarrhea, ondansetron or prochlorperazine for nausea, hydroxyzine for anxiety, and sleep hygiene for insomnia.
Do not stop high-dose opioids abruptly without a plan. A measured taper or transition to medications for opioid use disorder (MOUD) is safer.
FDA-Approved Medications for OUD: Quick Comparison
| Medication | How it works | Setting | Pros | Considerations |
|---|---|---|---|---|
| Buprenorphine (SL films/tablets; monthly injection) | Partial agonist, high receptor affinity | Office-based & outpatient | Reduces cravings; ceiling effect lowers overdose risk; flexible dosing | Must start in mild–moderate withdrawal unless micro-dosing; interactions with sedatives |
| Methadone (daily clinic dosing) | Full agonist | Opioid Treatment Program | Strong for severe OUD and concurrent pain; structured support | QT prolongation risk; daily clinic attendance; sedation risk with benzos/alcohol |
| Extended-release naltrexone (monthly injection) | Antagonist blocks opioids | Office-based | Non-addictive; no withdrawal on stop | Requires full detox; relapse risk if missed; lower pain control |
Standards are outlined in the ASAM National Practice Guideline.
Adjunctive Supports and What to Avoid
- Adjuncts: clonidine or lofexidine, hydroxyzine, NSAIDs, antiemetics, and sleep supports (non-sedative first).
- Avoid: abrupt benzodiazepine cessation; rapid stimulant discontinuation when doses are high; mixing CNS depressants; starting naltrexone too early (precipitated withdrawal).
- Educate on overdose risk after a period of abstinence, as tolerance drops quickly. Provide naloxone and training.
For naloxone, fentanyl, and overdose data, see CDC Overdose Prevention.
Stimulant Use Considerations
No FDA-approved medications treat stimulant use disorder yet. Care focuses on:
- Gradual dose reduction if physiologically dependent
- Behavioral therapies (CBT, Contingency Management)
- Sleep regulation and nutrition
- Treating underlying ADHD or mood disorders with careful monitoring and non-stimulant options when appropriate
Coordinating Care and Rationalizing Polypharmacy
- Review all psychoactive meds; reduce duplication (e.g., two sedatives), choose the least risky options, and simplify regimens.
- Communicate with prescribers (primary care, pain, psychiatry) to align goals and taper schedules.
- Assess pain with multimodal strategies: physical therapy, non-opioid analgesics, interventional options, mindfulness, and pain reconditioning.
Behavioral Therapies and Family Involvement
Core, Evidence-Based Therapies

Rolling Hills Recovery Center uses therapies matched to each person’s goals and readiness:
- Cognitive Behavioral Therapy (CBT) for coping, cravings, and relapse triggers
- Motivational Interviewing to strengthen change talk and autonomy
- Contingency Management (CM) for reinforcing healthy behaviors (attendance, negative tests)
- Trauma-informed care for those with ACEs or PTSD
- Skills training: distress tolerance, emotion regulation, problem solving
Sessions can be individual, group, or family-based. Frequency is stepped up or down depending on risk.
Pain Reconditioning and Functional Restoration
Pain and addiction feed into one another. A practical approach includes:
- Reconceptualizing pain (hurt ≠ harm)
- Graded activity and pacing
- Breathing, relaxation, and mindfulness to downshift the nervous system
- Non-opioid meds when useful (acetaminophen, NSAIDs, SNRIs, gabapentin/pregabalin if appropriate)
- Sleep restoration and mood treatment to reduce pain intensity
Insomnia and Anxiety Treatment Without Overreliance on Sedatives
- CBT‑I for chronic insomnia
- Sleep hygiene steps: consistent schedule, dark cool room, limit late caffeine, screen curfew, reserve bed for sleep and intimacy
- Anxiety supports: CBT, exposure therapy, SSRIs/SNRIs or buspirone when indicated, exercise, and breathing practices
- Short-term, non-benzodiazepine adjuncts only if needed
Family Therapy and Reducing Stigma
Families often carry stress and confusion about prescription use. Useful steps:
- Family sessions that explain dependence vs addiction and safe use
- Boundaries and communication plans
- Encouraging nonjudgmental language and focusing on health, not blame
- Involving supportive partners or caregivers in medication safety and relapse prevention
Safety Planning and Secure Storage
- Lockboxes for controlled medications
- Count pills weekly; track refill dates; limit quantities when risk is high
- Never share prescriptions
- Create an overdose plan: who to call, where naloxone is kept, how to use it
- If children or teens are at home, secure storage is non-negotiable
Culturally Responsive Care
Treatment respects culture, faith, language, gender identity, and family roles. Assessment asks what recovery looks like in the person’s community and adapts care accordingly. Telehealth or bilingual services are offered when helpful.
Aftercare, Relapse Prevention, and Recovery Supports
Ongoing MAT and Therapy
Most people do best with continued medication-assisted treatment (MAT) like buprenorphine or methadone for months to years, paired with therapy. Stopping too soon raises relapse risk. Plans are individualized, and stability matters more than speed.
- Regular medication visits
- Therapy: CBT, MI, or CM, adjusted to need
- Medical follow-up for pain, sleep, mood, and other conditions
- Coordination with primary care and specialists
Urine Drug Testing Used Clinically, Not Punitively
- Purpose: inform care, verify adherence, detect unexpected substances that raise risk (e.g., fentanyl when not prescribed)
- Discuss results openly; adjust the plan rather than punish
- Confirmatory testing for unclear or unexpected screens
Gradual Step-Downs and Transitions
- From higher to lower levels of care as skills and stability grow: inpatient or residential → intensive outpatient program → standard outpatient → recovery check-ins
- If instability returns, step up intensity promptly; no shame & no delay
For integrated mental health and addiction care in the state, see our article on dual diagnosis treatment in NJ.
Return-to-Use Plans: A Clear Template
A written plan reduces harm and speeds recovery if a slip happens. A simple template:
- My early warning signs: thoughts, people, places, body cues
- My top 3 coping moves: leave the situation, call a support, grounding exercise
- My safety steps: do not use alone; carry naloxone; avoid mixing with alcohol or benzos
- Who I contact within 24 hours: clinician, sponsor/peer, trusted family member
- Medication plan: continue buprenorphine/methadone as prescribed; if missed doses, call clinic for same-day guidance
- Transportation plan: if impaired, no driving; rideshare or call support
- Reset appointment: date/time for a quick check-in within 72 hours
This plan is rehearsed during sessions and kept in wallet and phone notes.
Peer Support and Community Options
- SMART Recovery or other secular groups
- 12-Step meetings for those who prefer them
- Online meetings for mobility or time limits
- Family peer support options for loved ones
- Faith-based supports if aligned with values
Vocational and Academic Support
- Return-to-work or school planning with flexible schedules
- Documentation for employers or schools when needed (e.g., safety-sensitive roles, medication verification)
- Skills workshops: resume building, interview practice
Digital Check-Ins and Monitoring
- Weekly text or app prompts for craving/withdrawal ratings
- Mood and sleep tracking
- Telehealth booster sessions during high-risk stretches (holidays, anniversaries, postoperative periods)
Measuring Outcomes That Matter
Track simple, meaningful metrics:
- Craving intensity (0–10)
- Days of nonmedical use
- Function (work/school attendance, activity levels)
- Sleep hours and quality
- Pain interference score
- Medication adherence (percent of doses taken as planned)
If metrics slip, adjust quickly, dose changes, added therapy, or stepped-up support.
When Documentation is Needed
- Legal or driver’s license matters: provide verification of treatment participation and drug testing when appropriate
- Employment: safety notes for sedating medications; letters confirming stabilized MAT
- School: accommodation requests (testing times, reduced evening activities while tapering sedatives)
For care coordination or to explore programs, Rolling Hills Recovery Center offers evidence-based options. See an overview of the best addiction treatment in NJ.
Harm Reduction, Safety, and New Jersey Considerations
Naloxone: Everyone at Risk Should Have it
- Offer naloxone to anyone using opioids or mixing sedatives, and to their family.
- Teach recognition of overdose: unresponsiveness, slow or no breathing, blue lips.
- Practice the steps with the device in hand (spray or auto-injector).
- Store an extra kit in the home and car.
Fentanyl and Test Strip Education
- Fentanyl can be present in counterfeit pills and powders. Even small amounts can be deadly.
- Fentanyl test strips can reduce risk; follow instructions carefully, and remember a negative result is not a guarantee.
- New Jersey harm reduction programs provide education on test strip use; check current local availability and policies.

Medication Take-Back and Safe Disposal
Expired or unused medicines should not linger at home.
- Use DEA take-back events or authorized collection sites.
- If no take-back option: follow FDA recommendations for disposal; some high-risk opioids are on the FDA flush list.
- Remove personal info from bottles before discarding.
- FDA resource: Disposal of Unused Medicines.
Driving and Safety-Sensitive Work
- Do not drive or operate machinery when starting, increasing, or tapering sedating medications.
- If on buprenorphine or methadone and stable, many people can drive safely; decide individually and avoid other sedatives.
- Provide employer notes for temporary duty modifications if needed.
Pregnancy and Postpartum Care
- Opioid use disorder: methadone or buprenorphine are the standard of care in pregnancy; avoid withdrawal that can stress the fetus.
- Breastfeeding is often encouraged with MOUD, particularly buprenorphine/methadone; review case-by-case.
- Avoid benzodiazepine and alcohol co-use.
- Postpartum is a high-risk time for relapse; increase supports and consider home naloxone for the family.
- Coordinate with OB/GYN, pediatrics, and lactation services.
Pain Care Alternatives and Perioperative Planning
- Multimodal analgesia: acetaminophen, NSAIDs (if safe), regional anesthesia, nerve blocks, and nonpharmacologic strategies.
- For those on MOUD:
- Continue buprenorphine through procedures when possible; split dosing can aid pain control.
- If methadone-maintained, continue baseline dose and add short-acting opioids if necessary under supervision.
- Avoid unmanaged benzodiazepine additions; consider non-sedative anxiolytics.
- Communicate perioperative plans with surgical teams weeks in advance when possible.
New Jersey-Specific Resources and Considerations
- NJ Prescription Monitoring Program (NJPMP) checks should be routine when prescribing or evaluating controlled substances.
- DMHAS provides up-to-date public resources, harm reduction info, and behavioral health contacts: NJ DMHAS.
- Prescribing norms in New Jersey emphasize the lowest effective dose, the shortest duration, and avoiding high-risk combinations.
- Many pharmacies in NJ dispense naloxone without an individual prescription under standing orders; ask locally.
- For community data on overdose trends and fentanyl presence, review state dashboards and CDC reports.
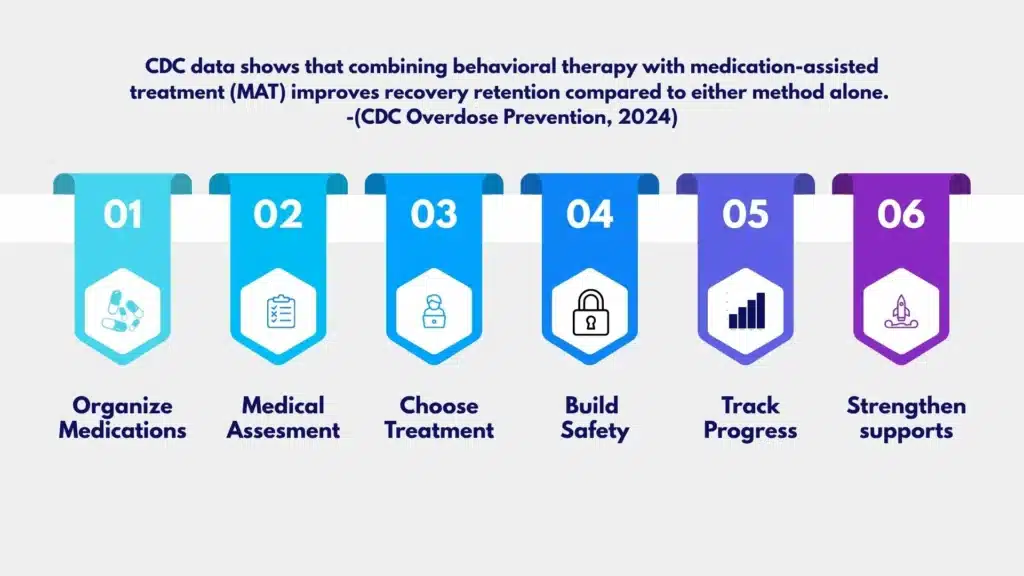
How to Get Started: Step-by-Step
Step 1: Organize Information Before the First Visit
- Make a list (photo ok) of every medication and supplement with dose and timing.
- Note allergies & past side effects.
- Write down top 3 goals (e.g., reduce cravings, sleep 7 hours, get back to work) and 3 worries.
Step 2: Expect a Thorough, Nonjudgmental Assessment
- Screening, DSM‑5 criteria review, and a focused physical exam
- Urine drug testing explained as a tool, not a test to pass
- NJPMP review and medication reconciliation
- Safety screen: suicide risk, overdose risk, driving
Step 3: Choose a Starting Path
- If withdrawal risk is high, begin medical detox or start MOUD
- Create a benzodiazepine taper calendar if needed
- Set therapy frequency and format (individual, group, family)
Step 4: Build Safety Into Daily Life
- Obtain naloxone and teach at least one support person
- Use a lockbox for medications and a weekly pill organizer
- Avoid mixing sedatives and alcohol; plan for rides if sedated
Step 5: Track Progress and Adjust
- Weekly self-check: cravings (0–10), sleep hours, pain interference (0–10), missed doses
- Share this log at visits; adjust doses or therapy as needed
- Schedule periodic medication reviews to reduce polypharmacy
Step 6: Strengthen Recovery Supports
- Pick at least one peer meeting format
- Identify two go-to coping skills for cravings
- Use digital reminders for dosing and appointments
Practical Tools and Templates
Medication and Safety Checklist
- Pill organizer and lockbox set up
- Medication list updated and shared with all prescribers
- Naloxone kits at home and in car; household trained
- No alcohol or benzo use with opioids or MOUD
- Safe storage out of reach of children and visitors
1‑Page Benzodiazepine Taper Calendar Template
- Top line: current daily dose and target monthly reduction (5–10%)
- Weekly boxes with new dose and time of day
- Side note: sleep and anxiety rating boxes (0–10) each day
- Space to record any missed or extra doses
- “Hold” rule: if symptoms ≥7/10 for 3 days, hold at current dose and call clinic
MOUD Start Worksheet
- Last opioid use time/date
- Withdrawal checklist (yawning, gooseflesh, sweating, runny nose, GI upset)
- COWS score estimate
- First dose plan (standard vs micro-induction)
- Follow-up contact method within 48–72 hours
Return-to-Use Rapid Response Card
- Warning signs → 3 coping moves → who to call → where naloxone is kept
- Transportation alternatives pre-loaded in app
- Appointment slot reserved weekly for urgent check-ins
How Rolling Hills Recovery Center Personalizes Care
- Evidence-based and holistic: MAT with buprenorphine or methadone coordination, plus CBT, MI, CM, trauma-informed therapy, and wellness practices (sleep, nutrition, movement).
- Integrated medical and behavioral care: anxiety, depression, PTSD, ADHD, pain, and insomnia addressed alongside addiction.
- Flexible levels of care: inpatient stabilization, intensive outpatient, and standard outpatient pathways, with telehealth options for New Jersey residents when appropriate.
- Family involvement: structured family sessions, education, and plans for home safety & medication storage.
- Continuous measurement: simple dashboards for cravings, function, and adherence to adapt the plan quickly.
For terminology, risks, and broader context on prescription opioids, review NIDA, Prescription Opioids. For safety and disposal, the FDA medicine disposal page is reliable. Standards for medication treatment are detailed in the ASAM National Practice Guideline. New Jersey state resources for behavioral health and harm reduction are available through DMHAS.
Conclusion
Recovery from prescription drugs is possible. It relies on clear assessment, safe detox and medications, therapy, family help, and steady aftercare. Watch for tolerance, lost control, early refills, seek help early. Use naloxone, lock meds, plan for triggers.
Frequently Asked Questions (FAQs)
What is Prescription Drug Addiction, and How is it Different From Dependence?
Prescription drug addiction is a pattern of compulsive use of medications such as opioids, benzodiazepines, or prescription stimulants despite harm. It involves loss of control, cravings, and continued use that affects health, work, or relationships.
Dependence is different: the body adapts to the drug, leading to tolerance and withdrawal, but not necessarily compulsive use. Both can occur together.
Clinicians evaluate drug addiction using symptom patterns (for example, escalating doses, risky use, inability to cut down) and check safety risks before changing any medication, especially in NJ where prescribing rules are set to protect patients.
What are Early Signs of Prescription Drug Addiction Families Should Notice?
Common early signs of prescription addiction include:
• Taking more than prescribed or taking it more often
• Running out early, frequent “lost” prescriptions, or urgent refill requests
• Cravings, preoccupation with dosing, secrecy
• Withdrawal symptoms between doses (sweats, shakiness, anxiety, body aches)
• Doctor shopping or mixing with alcohol or other drugs
If these show up, speak with the prescriber, do not change doses on your own. In New Jersey, clinicians also review the state monitoring program to spot unsafe patterns and reduce risk.
How is Prescription Drug Addiction Treated Safely?
Safe care for prescription drug addiction starts with a medical assessment, including current meds, mental health, pain, sleep, and overdose risk. Evidence-based treatments may include:
• Opioids: buprenorphine or methadone to stabilize, then ongoing recovery support; naltrexone for some after detox
• Benzodiazepines: slow, individualized taper; never abrupt stops due to seizure risk
• Stimulants: careful monitoring, behavioral therapies, and treatment for co-occurring ADHD if present
• Therapies: CBT & Motivational Interviewing, family involvement, relapse-prevention planning
• Safety: naloxone on hand for opioid risk, secure storage, and proper medication disposal
Care in New Jersey follows medical standards, with coordinated therapy and medication management to reduce harm and build steady recovery.
How Can Someone Support a Loved One with Prescription Drug Addiction Without Making it Worse?
Support starts with safety and compassion. Use calm, specific examples of concern, and ask about their goals. Practical steps:
• Encourage a medical evaluation before any dose changes
• Keep naloxone for opioid risk and learn how to use it
• Lock or count medications at home, avoid sharing pills
• Do not abruptly stop benzodiazepines; help arrange a supervised taper if needed
• Reduce triggers: alcohol, unsafe mixing, driving while sedated
• Offer to attend appointments, and follow up kindly
Small, steady changes matter. Prescription drug addiction is treatable, and pressure or blame usually backfires.
How Does Rolling Hills Recovery Center Help with Prescription Drug Addiction?
For prescription drug addiction, care may include detox placement, medication for opioid use disorder when indicated, careful benzodiazepine tapers, CBT & family therapy, mindfulness and nutrition, and coordinated aftercare. Treatment plans are tailored, with close monitoring, so progress is safe, realistic, and sustainable.
What are Prescription Opioids?: https://nida.nih.gov/publications/drugfacts/prescription-opioids
What is Buprenorphine?: https://www.samhsa.gov/substance-use/treatment/options/buprenorphine
What is Methadone?: https://www.samhsa.gov/substance-use/treatment/options/methadone
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












