Choosing the best rehab in NJ should center on safety, evidence-based care, and real medical oversight. This section clarifies levels of care, what to look for (CBT, MAT, psychiatry), insurance & cost basics, and early steps. Patients and families can use these criteria to make informed decisions and start recovery with confidence.

Key Takeaways
- Safety and evidence come first: CBT, DBT, motivational therapies, contingency management, plus MAT for opioid or alcohol use disorder.
- Verify NJ DMHAS license and Joint Commission or CARF accreditation; ask about psychiatry & co-occurring mental health, trauma-informed care, family work, and outcomes.
- Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches; its team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
- Match level of care to current need, detox, residential, PHP, IOP, or outpatient, and plan aftercare from day one; include naloxone and relapse-prevention skills.
- Understand costs and coverage: confirm benefits, prior authorization, and any copays; request clear pricing, payment options, and work-leave paperwork when needed.
Defining “Best” Addiction Treatment in New Jersey
What “Evidence‑Based” Actually Looks Like

Programs that consistently help people stabilize and stay in recovery use evidence-based treatments with strong research support. In New Jersey, the gold standard includes:
- Cognitive Behavioral Therapy (CBT) to identify triggers, build coping skills, and change high‑risk patterns
- Dialectical Behavior Therapy (DBT) skills for distress tolerance, emotion regulation, and interpersonal effectiveness
- Contingency Management (CM) to reinforce recovery behaviors through structured incentives
- Motivational Interviewing is woven throughout care to strengthen engagement and resolve ambivalence
- Medication‑Assisted Treatment (MAT) for opioid and alcohol use disorders: methadone, buprenorphine & naltrexone
Rolling Hills Recovery Center emphasizes these modalities, pairing them with holistic practices like structured movement and mindfulness. For many, adding safe physical activity improves mood and sleep; see how exercise in recovery can complement therapy.
State Licensure and Third‑Party Accreditation
- New Jersey licensure: Programs should be licensed by the New Jersey Division of Mental Health and Addiction Services (DMHAS). Verify licensure and find program types on the DMHAS website: DMHAS
- Independent accreditation: Look for The Joint Commission or CARF accreditation. Both review safety, quality improvement, and care standards
These are not just badges. They indicate ongoing audits, clinical standards, and patient safety policies are in place.
Robust Medical Oversight
Medical leadership matters. High‑quality programs have:
- 24/7 nursing on detox and residential units
- Physicians with addiction medicine or addiction psychiatry experience
- Clear protocols for withdrawal management (including CIWA/COWS monitoring)
- On‑site or promptly available psychiatry
- Medication reconciliation, lab screening, and chronic disease management
Rolling Hills Recovery Center leverages a team approach, including physicians, APNs, licensed therapists, and case managers, so patients are medically safe while therapies progress.
Co‑Occurring Mental Health and Trauma‑Informed Care
Substance use often intersects with depression, anxiety, PTSD, ADHD, bipolar spectrum symptoms, and other conditions.
Best‑in‑class programs:
- Screen and treat co‑occurring disorders
- Use trauma‑informed practices (safety first, choice, collaboration, and empowerment)
- Provide psychiatric evaluation and ongoing medication management
- Run specialized tracks where needed (e.g., ADHD plus stimulant misuse).
Family Involvement

Families benefit from clear communication and coaching. Strong programs:
- Offer family education on substance use, boundaries, and relapse warning signs
- Schedule regular updates and family sessions
- Provide resources for family self‑care and support
Timely Access, Outcomes, and Aftercare Strength
Quality programs:
- Maintain low waitlists or rapid‑access slots
- Track outcomes (e.g., patient‑reported recovery progress, readmissions) to improve care
- Build durable aftercare: step‑downs, alumni support, relapse prevention plans, care coordination, and primary care handoffs
Rolling Hills centers continuing care around individualized relapse prevention, recovery coaching, and linkage to community supports to bridge the first risky months after discharge.
Harm Reduction and Naloxone in New Jersey
New Jersey supports harm reduction. Essentials:
- Naloxone (Narcan) is available statewide under a standing order. Pharmacists can dispense without an individual prescription, often at low or no cost
- Syringe access and safe‑use education reduce infections and overdose deaths
- Fentanyl contamination is common; talk with clinicians about test strips and safer‑use education for loved ones not yet ready for treatment
For broad science on effective treatments and medications, see NIDA treatment resources.
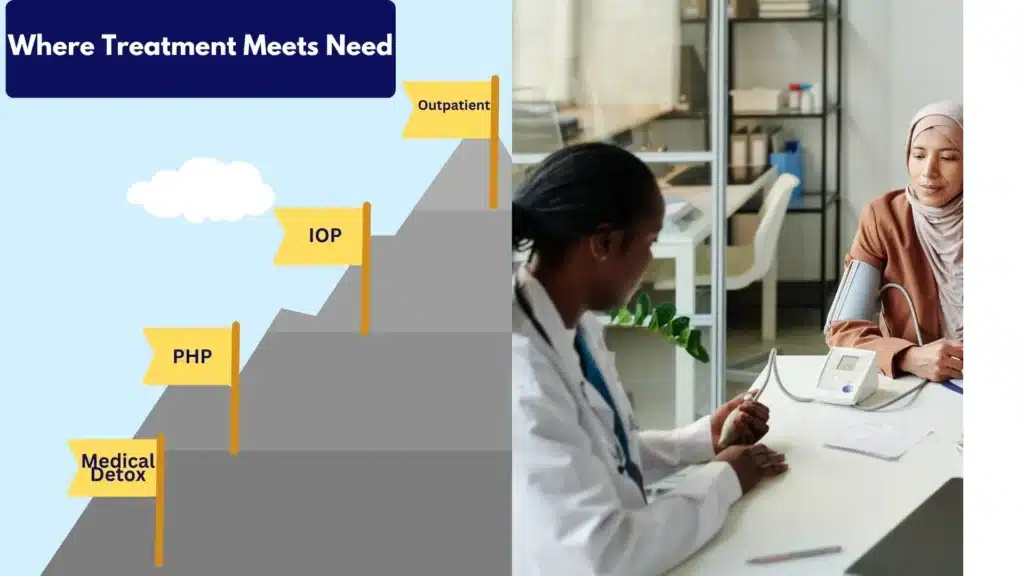
Levels of Care in New Jersey to Compare
Different levels of care match different needs. A quick comparison:
| Level of Care | Setting | Typical Duration | Structure (hrs/wk) | Ideal For | MAT Available |
|---|---|---|---|---|---|
| Medical Detox | Inpatient medical unit | 3–7 days | 24/7 | Moderate–severe withdrawal risk; medical monitoring needed | Yes (all) |
| Residential/Inpatient | 24/7 facility | 2–6 weeks (varies) | 40+ | High relapse risk, unstable housing, need for intensive structure | Yes |
| Partial Hospitalization (PHP) | Outpatient day program | 2–4 weeks | 20–30 | Step‑down from inpatient or step‑up from IOP; daily structure | Yes |
| Intensive Outpatient (IOP) | Outpatient | 4–12 weeks | 9–15 | Moderate support needed while living at home | Yes |
| Standard Outpatient (OP) | Clinic/telehealth | Ongoing | 1–6 | Maintenance care, relapse prevention, therapy | Yes |
| MAT Programs | Clinic/office | Ongoing | Varies | Opioid or alcohol use disorder with medication support | Yes |
Below is what each means in practice.
Medical Detox
- Medical detox in New Jersey offers supervised withdrawal from alcohol, opioids, benzodiazepines, and other substances
- Medications tailored to withdrawal severity (e.g., buprenorphine for opioids; benzodiazepines for alcohol/benzo withdrawal; adjuncts for comfort)
- Vital‑sign monitoring, hydration, nutritional support, and sleep management
- Transition planning to residential, PHP, or IOP starts immediately
Residential/Inpatient
- 24/7 structured environment with daily groups, individual therapy, and family programming
- Useful when home is unstable or triggers are overwhelming
- On‑site nursing and physician coverage; psychiatry to stabilize co‑occurring symptoms
- Skill building: coping, DBT skills, relapse prevention, sober social routines
Partial Hospitalization Program (PHP)
- Full‑day programming 5–6 days/week with medical and psychiatric oversight
- Ideal for those ready to step down from inpatient or who need a robust alternative to hospitalization
- Intensive therapy, MAT management, case management, and family engagement
Intensive Outpatient Program (IOP)
- Intensive Outpatient Programs (IOP) in NJ typically operate 3–4 days/week, usually 3 hours/day, plus individual sessions
- Focus on relapse prevention, trigger management, coping skills, and ongoing MAT
- Fits with work or school schedules; virtual options may exist where appropriate
Standard Outpatient
- Weekly or biweekly therapy, peer support, and medication management
- Good for maintenance, early recovery stabilization, or long‑term support
MAT: Methadone, Buprenorphine, and Naltrexone
- Methadone: Dispensed at federally certified Opioid Treatment Programs (OTPs). Strong evidence for reducing mortality and improving retention
- Buprenorphine: Office‑based or clinic‑based. The federal X‑waiver was removed, expanding access. Typically combined with naloxone in sublingual form
- Naltrexone: Monthly injection or daily oral; requires full detoxification from opioids first; also indicated for alcohol use disorder
All three medications reduce relapse risk when combined with counseling and recovery supports.
Recovery Support and Relapse Prevention
- Aftercare planning: appointment handoffs, medication refills, mutual‑help linkages, recovery coaching
- Skills refreshers: urge surfing, refusal skills, crisis plans, sober‑social routines
- Family education and boundaries work
- Alumni programming and check‑ins to maintain accountability
How to Choose Smartly
Step 1: Start with an ASAM‑Informed Assessment
- Intake should screen for substance use severity, withdrawal risk, mental health, medical conditions, social supports, and housing
- The American Society of Addiction Medicine (ASAM) dimensions help match you to the right level of care
- Ask for clarity: Which ASAM level is recommended and why?
Quick template to ask on the first call:
- What ASAM level of care do you recommend for my situation?
- What criteria put me at that level? What would change it?
- How fast can admission occur? Is there a waitlist?
Step 2: Verify Individualized Plans and Evidence‑Based Programming
- Treatment plan should be written with the patient, not pre‑filled
- Confirm a mix of individual therapy and evidence‑based groups (CBT, DBT, CM)
- Ask how progress is measured (e.g., goals, symptom tracking, urine screens used clinically, not punitively)
Questions to ask:
- How many individual therapy sessions per week?
- Which specific groups are offered? How often?
- How are trauma and co‑occurring disorders addressed?
Step 3: Confirm MAT Availability and Psychiatry Access
- Can the program start or continue methadone, buprenorphine, or naltrexone?
- How quickly can psychiatry evaluate and adjust medications?
- Are withdrawal symptoms managed on site?
Step 4: Check Credentials and Staffing Ratios
- Are therapists licensed (LCSW, LPC, LMFT, LADC/LCADC)?
- Is there 24/7 nursing (for inpatient) and physician availability?
- What is the typical group size? How many patients per clinician?
Step 5: Practical Supports
- Transportation assistance or rideshare vouchers to reduce missed sessions
- Bilingual services and interpreters
- Evening/weekend programming options
- Family scheduling flexibility
Step 6: Insurance Verification and Network Status
- Have the program verify benefits for NJ FamilyCare (Medicaid) or your commercial plan
- Ask if they are in‑network; if out‑of‑network, what is the projected out‑of‑pocket?
- Get a written estimate before admission, including labs and medications
Questions to clarify:
- What will I owe each week at my authorized level of care?
- What happens if additional days are recommended but insurance denies?
- Can you help submit appeals?
Red Flags to Avoid
- “Guaranteed cure” or promises of 100% success
- Vague pricing or refusal to provide an estimate
- No medical oversight for moderate to severe withdrawal
- No MAT options offered for opioid or alcohol use disorders
- No individualized plan or minimal individual therapy
- Unwillingness to coordinate with your family or outpatient providers
A Quick Vetting Checklist You Can Use Today
- Licensed by NJ DMHAS and accredited (Joint Commission or CARF)
- ASAM‑aligned assessment completed before or at intake
- CBT, DBT, and contingency management in the schedule
- MAT offered on-site or through partner providers
- Psychiatry available within days (or faster if needed)
- Co‑occurring disorders treated; trauma‑informed practices in place
- Family programming and regular updates
- Transportation and bilingual supports available
- Clear costs in writing; insurance verified; in‑network when possible
- Plan for aftercare starts on Day 1
Costs and Insurance Basics in New Jersey
Parity Protections, Prior Authorization, and Appeals
- Mental health and substance use benefits are protected by federal and state parity laws; coverage must be comparable to medical/surgical benefits
- Prior authorization rules vary by plan. Short “stabilization” authorizations are common; quality programs help with ongoing authorizations
- If coverage is denied, you have appeal rights. The New Jersey Department of Banking and Insurance can help consumers understand benefits and file complaints: NJ Department of Banking and Insurance
Tip: Keep all denial letters and notes from phone calls (date, person, reference number). Programs can supply supporting clinical documentation.
Typical Cost Ranges by Level of Care
The cost of rehab in NJ varies based on location, staffing, and insurance contracts. Ballpark figures in New Jersey:
- Medical detox (inpatient): Often billed per diem. Without insurance, several thousand dollars per day is common; with insurance, deductibles/co‑insurance apply
- Residential/inpatient: Self‑pay rates may range from low to mid five figures for 30 days; in‑network insurance reduces out‑of‑pocket costs significantly
- PHP: Often billed per day; with insurance, expect copays or coinsurance. Self‑pay daily rates can be several hundred to over a thousand dollars
- IOP: Typically billed per session or per day; self‑pay might run a few hundred dollars per day of attendance
- Standard outpatient: Standard therapy rates vary; insurance usually covers with a copay
- MAT medications: Cost depends on medication type and insurance formulary; generics reduce costs. Methadone is typically covered via OTP participation; buprenorphine and naltrexone coverage varies by plan
Always request a Good Faith Estimate if paying out of pocket.
Using FMLA and Short‑Term Disability
- Many patients use the Family and Medical Leave Act (FMLA) to protect job time while in treatment
- Short‑term disability may offset lost wages during detox, residential, or PHP
- Programs can provide documentation (diagnosis codes, treatment start dates, anticipated duration)
Payment Plans and Confirming Coverage Before Admission
- Reputable programs offer transparent payment plans when needed
- Always confirm coverage and out‑of‑pocket estimates before admission
- Ask whether labs, medications, and any outside services (e.g., imaging) are included or billed separately
If something isn’t clear, pause. Get it in writing and review with a trusted person.
Getting Started and What to Expect the First Week
Pre‑Admission Screening
- A brief phone screen to confirm safety, withdrawal risk, and immediate needs
- Benefit verification for NJ FamilyCare or commercial plans
- Scheduling of admission date or same‑day arrival if urgent
- Transportation support arranged if available
Template to organize details:
- Admission date/time:
- What to bring (ID, insurance card, medication list):
- Any fasting/lab requirements:
- Family contact and update schedule:
Day 1: Medical Evaluation and Withdrawal Management
- Nurse intake, vitals, and laboratory screening (as indicated)
- Physician exam and medication reconciliation
- Initiation of withdrawal management protocols if needed (e.g., buprenorphine induction)
- Safety planning and review of any acute risks (overdose, self‑harm), with crisis resources on hand, such as the 988 Suicide and Crisis Lifeline
Orientation, Therapy Schedule, and Daily Structure
Expect a structured schedule that may include:
- Morning check‑in and vital signs (higher intensity levels)
- Group therapy: CBT skills, relapse prevention, psychoeducation
- Individual therapy 1–2x/week (varies by level of care)
- Medication management and psychiatry follow‑up
- Wellness blocks: movement, mindfulness, sleep hygiene. Programs with holistic tracks often integrate graduated physical activity
- Case management: legal, housing, work, and school coordination
A sample first‑week schedule (adjusted by level of care):
- Monday: Intake labs; CBT group; individual therapy; MAT check‑in
- Tuesday: DBT skills; family session; recovery planning
- Wednesday: Psychoeducation; contingency management group; peer support
- Thursday: Psychiatric follow‑up; relapse prevention; wellness
- Friday: Safety plan review; community supports; discharge planning touchpoint
Family Check‑Ins
- With consent, families receive updates at least weekly
- Family sessions focus on communication, boundary‑setting, and aftercare coordination
- Loved ones are coached on overdose response and naloxone access under New Jersey’s standing order
Discharge Planning Begins Day 1
Effective programs plan forward:
- Confirm next level of care (e.g., IOP or OP), appointment dates, and transportation
- Verify MAT continuity (prescriptions, next dispensing site)
- Build a relapse prevention plan: triggers, coping, early warning signs, and a personal crisis plan
- Connect with community supports: mutual‑help meetings, recovery community centers, and peer coaching
- Provide harm‑reduction tools for safety if relapse occurs (naloxone, safe‑use education, test strip information)
When identity‑affirming care is important, ensure the continuing care plan includes resources matched to the patient’s needs.
Decision Anchors When Rankings are Absent
In New Jersey, public “rankings” rarely capture what matters most for outcomes. Anchors that do:
- Licensure by DMHAS and third‑party accreditation (Joint Commission or CARF)
- Evidence‑based care: CBT, DBT, CM, and properly used MAT
- Real medical oversight with psychiatry access
- Co‑occurring disorder and trauma‑informed capabilities
- Family involvement and education
- Timely access (low waitlists and rapid induction for MAT)
- Clear costs, written estimates, and insurance support
- Outcomes tracking and strong aftercare
For licensure and program types, start with DMHAS. For science on what works, see NIDA treatment resources. For coverage rights and parity help, consult the NJ Department of Banking and Insurance. If there is an immediate safety concern, contact the 988 Suicide and Crisis Lifeline.
Rolling Hills Recovery Center aligns care with these anchors, evidence‑based therapies, MAT, inclusive programming, medical and psychiatric oversight, and a recovery plan that starts at admission and continues well after discharge.
Conclusion
Choosing addiction care in New Jersey comes down to evidence-based treatment, strong medical oversight, and a level of care that fits. Key steps: get an assessment, verify insurance & aftercare, ask about MAT and therapy.
Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey offering evidence-based and holistic approaches.
Our experienced team helps people overcome substance abuse and achieve lasting results, verify benefits, book an assessment, and begin treatment.
Frequently Asked Questions (FAQs)
What Levels of Care are Available in New Jersey?
Addiction treatment in New Jersey typically includes several levels of care so treatment can match clinical need.
Common options: medical detox for safe withdrawal; residential/inpatient for 24/7 support and stabilization; partial hospitalization (PHP) for intensive daytime treatment; intensive outpatient (IOP) several days a week; standard outpatient for step-down care; and medication-assisted treatment (MAT) for opioid or alcohol use disorders.
Movement between levels is based on ongoing assessment & progress, not a one‑size approach.
How Does Insurance Usually Work for Addiction Treatment in NJ?
Most commercial plans and many public plans cover treatment under mental health parity rules.
Coverage varies by plan: prior authorization may be required, length of stay can depend on medical necessity, and there may be co-pays or deductibles.
Verifying benefits up front helps prevent surprises. Documentation from the clinical team supports approvals, and appeals are possible if care is denied. Short-term disability or FMLA may help with time away from work during treatment.
When is Medication-Assisted Treatment Used During Treatment?
Medication-assisted treatment is considered for opioid use disorder (buprenorphine, methadone, naltrexone) and alcohol use disorder (naltrexone, acamprosate, sometimes disulfiram).
These medications are paired with counseling and recovery supports. They reduce cravings, stabilize brain chemistry, and lower overdose risk.
Dosing is individualized, monitored by a medical provider, and the duration can be short or long-term depending on response. It is evidence-based care, not swapping one drug for another.
What Should Families Expect in the First Week of Treatment?
The first week of treatment focuses on safety and clarity. Expect a medical and psychosocial assessment, labs when indicated, withdrawal management if needed, and a personalized care plan.
Orientation to the daily schedule happens fast, individual therapy, group therapy, medication review, sleep, and nutrition support.
Family contact is encouraged (when appropriate) to set expectations, boundaries, and a simple safety plan. Discharge planning starts early, even day one, so aftercare isn’t rushed later.
What Sets Rolling Hills Recovery Center Apart in Addiction Treatment?
Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches.
The team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
Clinically, that means validated therapies (such as CBT and motivational interviewing), careful medical oversight, coordinated care for co-occurring mental health, and practical family involvement.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












