
This article explains alcoholism in New Jersey through a clinical lens. It covers how alcohol use disorder is recognized, what symptoms matter, and safe next steps. Expect clear, evidence-based options for detox, medications, and therapy, plus practical screening tools and ways to prepare for an assessment at Rolling Hills Recovery Center.
Key Takeaways
- Alcoholism in New Jersey is common and treatable; notice early signs & use quick screens like AUDIT-C or CAGE. Two or more concerning answers should prompt a timely medical evaluation.
- Safe care works best in steps: supervised detox when withdrawal risk is present, then medications for alcohol use disorder (naltrexone, acamprosate, disulfiram) plus counseling. Pair meds & therapy with family support and the right level of care (residential, PHP, IOP, outpatient).
- In emergencies, call 911, place the person on their side, avoid giving more alcohol or inducing vomiting; after stabilization, arrange follow-up care. For emotional crises, call or text 988
- Prepare for an assessment: bring insurance and ID, a medication list, medical history, and simple goals. Expect screening for anxiety and depression, and labs if needed (LFTs, GGT, MCV); acting sooner often leads to better outcomes.
Scope and Trends in New Jersey
What Alcohol Use Disorder Means
Alcoholism is best described using the DSM-5 term alcohol use disorder (AUD). It is a medical condition with impaired control over drinking, preoccupation with alcohol, continuing use despite harm, and functional impairment. DSM-5 lists 11 criteria across four domains (control, social impairment, risky use, and pharmacologic criteria like tolerance and withdrawal). Severity is based on how many criteria are met over a 12‑month period:
- Mild: 2–3 criteria
- Moderate: 4–5 criteria
- Severe: 6 or more criteria
Any severity warrants attention. The goal is not judgment; it is early, compassionate care.
How Alcohol Harms Show Up in New Jersey
Statewide epidemiology from the New Jersey Department of Health (NJDOH) and national agencies offers a consistent picture:
- Emergency departments see thousands of adult and adolescent visits yearly, with alcohol implicated, intoxication, withdrawal, injuries, pancreatitis, gastritis, and trauma after falls or fights.
- Motor vehicle crashes involving alcohol continue to account for a meaningful share of fatalities and serious injuries. Law enforcement data and trauma centers in the state’s urban corridors and along the shore corridors report seasonal spikes.
- Mortality includes chronic liver disease and cirrhosis, certain cancers, and alcohol poisoning. Alcohol is a contributing cause in many violent deaths and suicides.
- Treatment admissions for AUD fluctuate with insurance coverage, treatment availability, and policy changes. Expanded telehealth and parity enforcement have changed access patterns since 2020.
Compared with national benchmarks from CDC and NIAAA, New Jersey’s binge drinking prevalence is often near or slightly below the national average, but even “average” translates to a significant public health burden. Alcohol’s harms concentrate unevenly by county and zip code, with patterns shaped by outlet density, pricing, and local norms.
References for data and definitions:
- New Jersey Department of Health (NJDOH)
- National Institute on Alcohol Abuse and Alcoholism (NIAAA)
- Centers for Disease Control and Prevention (CDC Alcohol)
Differences Across the State
New Jersey is diverse. Patterns vary between the urban corridor (Hudson, Essex, Union, Middlesex), suburban belts, college towns, and shore counties (Monmouth, Ocean, Atlantic, Cape May), with seasonal tourism.
| Region | Typical patterns | Implications for care |
|---|---|---|
| Urban corridor (north/central) | Higher alcohol outlet density near transit; co-occurring stimulant or opioid use in some neighborhoods; ED volumes reflect late‑night injuries and intoxication | Co-located services with primary care and mental health; evening clinic hours; integrated trauma care |
| Suburban belts | Home-based heavy drinking, impaired driving risk after social events; access barriers due to stigma | Confidential, flexible outpatient and intensive outpatient programs; employer EAP coordination |
| College towns | Binge episodes around games and Greek life; mixed nicotine/cannabis co-use | Campus SBIRT, peer-led prevention, amnesty education, quick linkage to care |
| Shore counties (seasonal) | Seasonal spikes in DUI, injuries, and detox demand; transient workforce and tourism | Surge-capable detox, partnerships with hospitals, mobile crisis capacity, safe ride outreach |
Local conditions matter. Treatment must fit the pattern and the person.
Post‑Pandemic Patterns
- Heavy drinking shifted to homes during COVID‑19 restrictions, with increases in retail alcohol sales and solitary drinking. Nationally, surveys showed more high‑risk drinking days, and the state followed this pattern.
- Telehealth for assessment and therapy increased access but does not replace in‑person detox when withdrawal is unsafe.
- Many people delayed care, then presented later with more medical complexity, liver disease, depression, and anxiety have been prominent co-occurring issues.
Risk Factors and Context
Social Determinants in New Jersey
- Housing costs and economic pressure: High rents and property taxes are common stressors. Financial strain can worsen drinking as a coping strategy and also limit access to treatment without insurance clarity.
- Commuting stress: Long commutes, shift work, and traffic add fatigue and stress, which increases evening or weekend drinking.
- Seasonal tourism: Shore communities see seasonal influxes that increase alcohol availability, social events, and impaired driving risk.
Addressing these requires practical supports, transportation to treatment, evening hours, and employer collaboration.
Outlet Density and Pricing
- Retail and bar density vary by municipality. Higher density correlates with more alcohol-related harm.
- Price promotions and extended hours can shape consumption. New Jersey’s market is privately operated with local licensing caps, so conditions vary town by town.
- Community coalitions often work with municipal leaders to balance economic interests with public safety.
Campus Drinking Pressures
- Tailgating, fraternity/sorority events, and social media challenges normalize heavy drinking. First-year students and athletes may be at higher risk.
- Effective strategies: screening during student health visits, amnesty policies for medical emergencies, peer mentors, and alcohol-free late-night programming.
Legal Landscape Shaping Availability and Norms
- Licensing and enforcement: The New Jersey Division of Alcoholic Beverage Control (ABC) regulates licensing of manufacturers, wholesalers, and retailers. Municipalities control local issuance within state limits.
- Underage laws: It is illegal for those under 21 to purchase or knowingly possess alcohol in public places. Under 21 motorists face “zero tolerance” for BAC at or above 0.01% with penalties.
- DUI/DWI: For drivers 21 and older, the per se limit is 0.08% BAC. Penalties escalate with BAC and repeat offenses and can include fines, license suspension, ignition interlock devices, and education. Open container laws apply in vehicles.
- Good to know: Medical amnesty and Good Samaritan protections may reduce penalties when seeking help for an intoxicated minor or a medical emergency. When in doubt, call 911.
For current statutes and penalties, see the New Jersey ABC and state judiciary resources.
Clinical Recognition and Screening
Red Flags at Home and in Clinic
- Tolerance: Needing more drinks to feel the same effect; drinking stronger beverages
- Withdrawal: Morning alcohol shakes, sweating, anxiety, nausea, or drinking to relieve these
- Loss of control: Drinking more or longer than planned; failed attempts to cut down
- Blackouts: Memory gaps after drinking
- Health impact: GI bleeding, gastritis, pancreatitis, sleep problems, neuropathy, or elevated blood pressure
- Social impact: DUI, missed work, strained relationships, or secrecy about drinking
Any of these is enough to start a conversation about care.
Screening Tools That Work
- AUDIT‑C: Three questions on frequency, quantity, and binge drinking. Fast, validated, useful in primary care and emergency settings.
- Full AUDIT: Ten items; better for severity stratification.
- CAGE: Four questions (Cut down, Annoyed, Guilty, Eye-opener). Useful, but less sensitive for women and some populations.
- Single‑item screen: “How many times in the past year have you had 5 (men) or 4 (women) or more drinks in a day?” A non‑zero answer indicates risk.
How to run a quick screen (3–5 minutes):
- Normalize: “I ask everyone about alcohol, because it affects health.”
- Use AUDIT‑C or a single item; score immediately.
- If positive, ask about withdrawal symptoms and safety risks (driving, falls, pregnancy).
- Assess readiness to change on a 0–10 scale; reflect back without judgment.
- Offer brief advice and set a concrete next step (follow‑up, referral, or medication trial).
Validated tool sources:
- WHO’s AUDIT materials
- NIAAA Clinician’s Core Resource
When to Order Labs
- Baseline labs in primary care or at intake may include: CBC (look for macrocytosis; MCV elevation), CMP (AST, ALT, bilirubin), GGT, lipid panel, HbA1c, and pregnancy test when appropriate.
- CDT (carbohydrate-deficient transferrin) can help detect heavy drinking over prior weeks.
- Thiamine, magnesium, and phosphate are often low with heavy use.
- If withdrawal is suspected: check vitals, CIWA‑Ar scoring, consider EKG if tachycardia or electrolyte abnormalities.
- Imaging and hepatology referral when evidence of advanced liver disease (thrombocytopenia, coagulopathy, ascites).
Labs support the history; they do not diagnose AUD alone.
Co‑Occurring Conditions and Trauma
- Anxiety, depression, PTSD, and chronic pain commonly co‑occur and can be both cause and consequence of alcohol use.
- Screen using PHQ‑9, GAD‑7, and PTSD screeners. Ask about sleep, trauma history, and suicidal ideation.
- Coordinate psychopharmacology carefully; limit benzodiazepines outside medically supervised withdrawal.
What Primary Care Can Do Today (SBIRT)
SBIRT = Screening, Brief Intervention, and Referral to Treatment:
- Screening: AUDIT‑C at intake and annually.
- Brief intervention (5–15 minutes): Provide feedback on risk, link alcohol to symptoms; use motivational interviewing. Set a specific goal (e.g., two alcohol‑free days weekly; no more than 3 drinks in one day).
- Referral to treatment: Same‑day warm handoffs to a detox or intensive outpatient program when indicated. Telehealth can bridge gaps.
Documentation tip: Record the screening tool used, score, brief advice provided, and the plan.
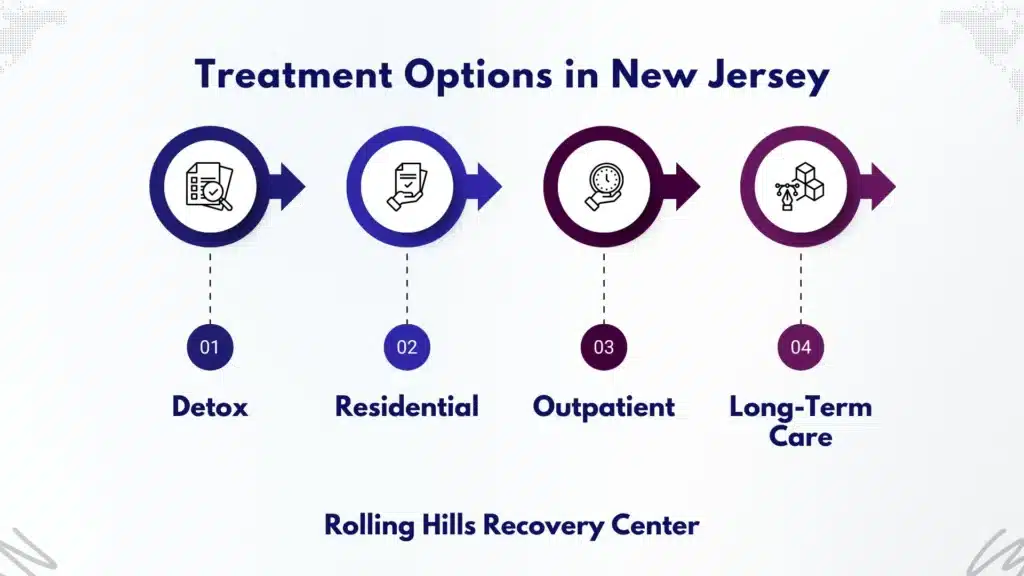
Treatment Pathways in New Jersey
The First 72 Hours: Safe Detox with Medical Oversight
Alcohol withdrawal can be dangerous. Medical detox is indicated when any of the following are present:
- History of severe withdrawal, seizures, or delirium tremens
- Significant daily use or morning drinking
- Unstable vitals, marked tremor, vomiting, or confusion
- Pregnancy, serious medical comorbidity, or lack of reliable support at home
Typical elements of supervised withdrawal:
- Benzodiazepine protocol based on CIWA‑Ar (symptom-triggered preferred when feasible)
- Thiamine before glucose, folate, multivitamins, fluids, and electrolyte correction
- Monitoring for seizures, Wernicke’s encephalopathy, and arrhythmia
- Early transition planning to medications for AUD and therapy
Rolling Hills Recovery Center coordinates closely with hospitals and primary care to ensure detox transitions into ongoing care. No one should leave detox without a plan and a medication discussion.
Medications for AUD
Evidence-based, FDA‑approved:
- Naltrexone (oral daily or extended‑release monthly injection): Reduces heavy drinking by lowering craving and reward from alcohol. Avoid if acute hepatitis or liver failure; check LFTs baseline and during treatment.
- Acamprosate (three times daily): Helps maintain abstinence by stabilizing glutamate/GABA balance. Renally cleared; suitable with liver disease (dose adjust in renal impairment).
- Disulfiram: Creates an aversive reaction if alcohol is consumed; best when supervised and when abstinence is the goal. Screen for cardiac disease and psychosis; educate thoroughly.
Additional options sometimes considered:
- Off‑label agents (e.g., gabapentin, topiramate) may help in select cases.
- Medications for co‑occurring depression or anxiety should be integrated with care, with an eye on sedation risks.
How to choose:
- Set the goal: cut down versus abstain.
- Review liver and kidney status.
- Weigh adherence preferences (daily pill vs. monthly injection).
- Start promptly, ideally before discharge from detox or at the first outpatient visit.
Therapies That Help
- Cognitive behavioral therapy (CBT): Skills for coping with triggers, restructuring thoughts, and planning sober activities.
- Motivational enhancement therapy (MET): Strengthens internal motivation and commitment to change.
- Contingency management: Incentives for meeting recovery goals, especially helpful for engagement.
- 12‑step facilitation and mutual‑help linkage: Works as a recovery support for many; participation is voluntary and can be paired with evidence‑based care.
- Trauma‑informed care: Safety, choice, collaboration, and empowerment are essential.
Family Involvement
Family systems can heal, too. Effective strategies:
- Education on AUD as a medical condition
- Coaching on communication and boundary setting
- Support for co‑dependent or enabling patterns
- Inclusion in relapse prevention planning
For details on how families can engage, see our resource on the role of family support in rehab.
Levels of Care and Matching
- Residential/inpatient: 24/7 support for severe AUD, unsafe home environment, or repeated relapse. Medical and psychiatric care on site.
- Partial Hospitalization Program (PHP): Daytime treatment (5–6 hours/day), home at night. Good for step‑down after residential or when an intensive structure is needed without a 24/7 stay.
- Intensive Outpatient Program (IOP): 9–12 hours/week; group and individual therapy; medication management. Compatible with work or school.
- Outpatient therapy and medication management: Weekly sessions, flexible scheduling, telehealth option.
Matching steps:
- Evaluate withdrawal risk and medical/psychiatric complexity.
- Assess home safety and support.
- Consider transportation and work obligations.
- Start at the least restrictive level that still ensures safety and efficacy; step up or down as needed.
Recovery Supports and Inclusive Care
- Peer recovery coaching, alumni groups, and community mutual‑help meetings are common pillars.
- Digital supports: craving trackers, breathalyzers with accountability features, and telehealth check‑ins.
Holistic Supports That Reinforce Sobriety
- Sleep hygiene, balanced nutrition, and movement are protective.
- Structured physical activity improves mood, sleep, and stress tolerance for practical ideas to build a movement plan into recovery.
Rolling Hills Recovery Center combines evidence-based treatment with holistic approaches, coordinated with your primary care clinician for continuity. Lab follow‑up, medication refills, and screening for relapse risks are aligned between teams.
Access, Safety, and Prevention
If Alcohol Poisoning is Suspected
Act fast. Signs of alcohol poisoning include vomiting, confusion, seizures, slow or irregular breathing, pale or bluish skin, or unresponsiveness. Step-by-step:
- Call 911 immediately.
- Keep the person on their side to prevent choking if vomiting.
- Do not leave them alone; monitor breathing and responsiveness.
- Do not give coffee, showers, or try to “sleep it off.”
- Provide responders with known alcohol amount, other substances, and medical conditions if known.
Remember: underage callers may have amnesty protections when seeking help. Safety first.
Mental Health Crisis and Suicide Risk
Alcohol can rapidly worsen depression and suicidal thoughts.
- Call or text 988 for the Suicide and Crisis Lifeline if there is any concern for self-harm.
- Remove access to firearms and large quantities of medications or alcohol during a crisis.
- If there is imminent danger, call 911 and state “mental health emergency.”
Safer Nights Out and On the Shore
- Use rideshare, designated driver, or public transit. Some shore towns and campuses offer safe ride programs; check local resources.
- Plan your limit in advance: no more than 3 drinks on any day and no more than 7 per week for women, and no more than 4/14 for men (NIAAA low-risk limits). Lower limits or abstinence are advised when on certain medications, during pregnancy, or with health conditions.
- Eat before drinking; alternate alcohol with water; avoid mixing with sedatives or opioids.
Workplace and Campus Policies That Help
- Good employer practices: clearly posted EAP contacts, supervisor training to recognize impairment, return-to-work agreements that include treatment support instead of automatic termination.
- College policies: Medical amnesty education, routine screening in student health, late-night alcohol-free programming, training for resident assistants, and peer outreach.
Planning a Treatment Call: A Quick Checklist
Before calling a program like Rolling Hills Recovery Center, gather:
- Insurance card (front/back) and photo ID
- Current medications and allergies
- Medical conditions and prior treatment history (including detox or rehab, dates if possible)
- Typical daily alcohol amount, time of last drink, and any withdrawal symptoms
- Safety concerns: seizures, suicidal thoughts, pregnancy
- Practical constraints: work schedule, childcare, transportation
- Personal goals: abstinence, cut down, repair relationships, protect job
What to ask on the call:
- Do you offer medical detox if needed?
- Which medications for AUD are available? Can injections be started?
- What are therapy options (CBT, MET), and are evening groups offered?
- How do you coordinate with my primary care clinician?
- Is family involvement welcomed, and how?
What to Expect at an Assessment
- Medical screening: vitals, withdrawal risk (CIWA‑Ar), labs as indicated.
- Psychosocial assessment: history, supports, housing, legal issues.
- Safety planning: suicide risk assessment, access to substances or weapons, emergency contacts.
- Treatment plan: level of care recommendation, medication options, first appointments, and consent forms.
- Practical support: verification of benefits, transportation planning, and a same- or next-day start when safety requires.
Relapse‑Prevention Skills and Community Coalitions

Core skills practiced early and often:
- Identify triggers: people, places, and feelings. Map out a week and mark risk times.
- Use “urge surfing”: delay 10 minutes, breathe, move, call a support, then re-evaluate.
- HALT check: Hungry, Angry, Lonely, Tired, act on the need, not the urge.
- Build a recovery routine: morning check-in, movement, meals, meetings, and sleep at set times.
- Digital helps: craving logs, drink trackers, and reminder apps for medications.
Community action matters too:
- Join coalitions that address outlet density, safe ride campaigns, and campus-community partnerships.
- Partner with primary care and behavioral health clinics to normalize screening and referral.
Simple Tools and Templates
Self‑monitoring drinking diary (print or note on phone):
- Each day: write date, number of standard drinks, time, place, mood before/after, people present, and any triggers.
- Weekly review: note patterns; choose one high‑risk slot to change next week.
Personal warning signs list:
- Early: skipping meals, poor sleep, “just one drink” thoughts, avoiding supportive people
- Middle: rationalizing detours to old bars, stopping meds or therapy
- Late: lying about plans, drinking alone, contacting old drinking friends
- Action: tell a support person, attend a meeting, book an extra therapy session, move your body for 20 minutes
Emergency contacts card:
- 988 (Suicide & Crisis Lifeline)
- A trusted person (name/phone)
- Your counselor/clinic
- Local taxi or rideshare code
Useful calculators and checkers:
- NIAAA standard drink calculator and low-risk drinking limits
- WHO AUDIT screening forms and scoring
Rolling Hills staff can help set up these tools and sync them with a care plan shared with your primary care clinician when you consent.
References and Further Reading
- New Jersey Department of Health (NJDOH): https://www.nj.gov/health/
- National Institute on Alcohol Abuse and Alcoholism (NIAAA): https://www.niaaa.nih.gov
- CDC Alcohol and Public Health: https://www.cdc.gov/alcohol/
- New Jersey Division of Alcoholic Beverage Control (ABC): https://www.nj.gov/oag/abc/
- WHO AUDIT (Alcohol Use Disorders Identification Test): https://www.who.int/publications/i/item/WHO-MSD-MSB-01.6a
Conclusion
Alcohol use disorder strains health, families, and life. Spot signs & use screening, act early, and choose evidence-based care with follow‑up. Detox, meds, and therapy work best together.
Frequently Asked Questions (FAQs)
What Does “Alcoholism in NJ” Mean in Medical Terms?
Alcoholism in New Jersey refers to alcohol use disorder (AUD) diagnosed by DSM-5 criteria.
The diagnosis is based on patterns such as loss of control over drinking, increasing tolerance, withdrawal symptoms, craving, spending a lot of time drinking or recovering, and continuing use despite harm.
Geography does not change the criteria, but local factors in New Jersey, commuting stress, seasonal tourism at the Shore, campus life, and outlet density, can influence risks and relapse triggers.
What Early Signs of Alcoholism Should Families Look For?
Common early signs include drinking more than planned, frequent hangovers, slipping grades or job performance, missed obligations, secrecy around alcohol, blackouts, and conflicts at home.
Physical clues: sleep problems, reflux or stomach pain, tremor in the morning, needing a “hair of the dog.” A brief screen like AUDIT-C or CAGE can help; if two or more concerns show up, an evaluation for alcohol use disorder is recommended, sooner rather than later.
How is Alcoholism Treated: Detox & Medications, Then Therapy?
Treatment is tailored, but often follows three steps:
• Stabilization: supervised detox for safety if withdrawal risk is moderate to high, using symptom-based care (e.g., CIWA-Ar).
• Medications for AUD: naltrexone (daily or monthly), acamprosate, or disulfiram when appropriate to reduce craving or support abstinence.
• Therapies and skills: CBT, motivational enhancement, relapse-prevention planning, family involvement, plus sleep, nutrition & stress care.
• Levels of care can include residential treatment, partial hospitalization, intensive outpatient (IOP), and standard outpatient. Co-occurring conditions (anxiety, depression, trauma) are treated alongside alcoholism to improve outcomes.
What Should Someone Bring and Expect at a First Assessment for Alcoholism at Rolling Hills Recovery Center?
Plan for a thorough intake. Bring photo ID, insurance card, a current medication list, allergies, past medical and mental health history, and any recent labs if available. The assessment typically includes:
• A medical exam and vital signs, with liver-related labs considered (LFTs, GGT, MCV) if indicated.
• Screening for withdrawal risk, craving, mood, sleep, and safety.
• A discussion of goals, supports, obstacles, and practical needs (work, family, transport).
• A clear plan for level of care, detox if needed, meds, and therapy.
What Should Be Done in an Alcohol Emergency in New Jersey, and How Can Risk Be Lowered?
If alcohol poisoning is suspected: call 911, stay with the person, keep them on their side to protect the airway, avoid giving more alcohol, don’t force vomiting. Share what was taken and when.
New Jersey’s Good Samaritan protections encourage calling for help. After stabilization, arrange follow-up for alcohol use disorder to address the root cause.
To lower risk: do not drive after drinking (use a designated driver or a ride app), set a drink limit before events, eat and hydrate, avoid mixing alcohol with sedatives or opioids, and have a buddy plan.
For emotional crises or thoughts of self-harm, contact the 988 Suicide & Crisis Lifeline.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












