Drug addiction is a medical condition, not a moral failure. It changes brain circuits that control reward, stress, and self-control, which is why cravings and relapse can happen. This article explains what drug addiction means, key signs of addiction and risks, how clinicians assess it, and evidence-based care that supports steady recovery for individuals and families.
“A physical and psychological dependence on a substance that has caused impairment and distress in an individual’s life.”
Laura Riley, LCADC | Clinical Director at Rolling Hills Recovery Center
Key Takeaways
- Addiction is a chronic, treatable medical condition that changes brain reward, stress, and self‑control systems; it isn’t a moral failing.
- Watch for key signs: strong cravings, using more or longer than planned, lots of time spent getting or using, problems at work or school, risky use, tolerance, and withdrawal. Overdose signs need 911, right away.
- Effective care blends medications for opioid or alcohol use disorders with counseling (CBT, motivational interviewing), family involvement, and safe withdrawal management.
- Harm reduction saves lives: carry naloxone, avoid using alone, consider fentanyl test strips where legal, and make an overdose plan. Aftercare & relapse prevention keep progress going.
What is Drug Addiction?
Drug addiction is a chronic, relapsing brain condition marked by compulsive substance use despite harm. Clinically, it is described in the DSM‑5 as “substance use disorder” (SUD), which exists on a spectrum from mild to severe.
The condition involves changes in reward and stress pathways, tolerance, and withdrawal. It is not a moral failing; it is a treatable medical condition with effective medication-assisted treatment (MAT), therapies, and recovery supports.
The DSM‑5 “Substance Use Disorder” Spectrum
The DSM‑5 does not use the term “addiction” as a diagnosis. Instead, it lists 11 criteria for SUD. The number of criteria met determines severity:
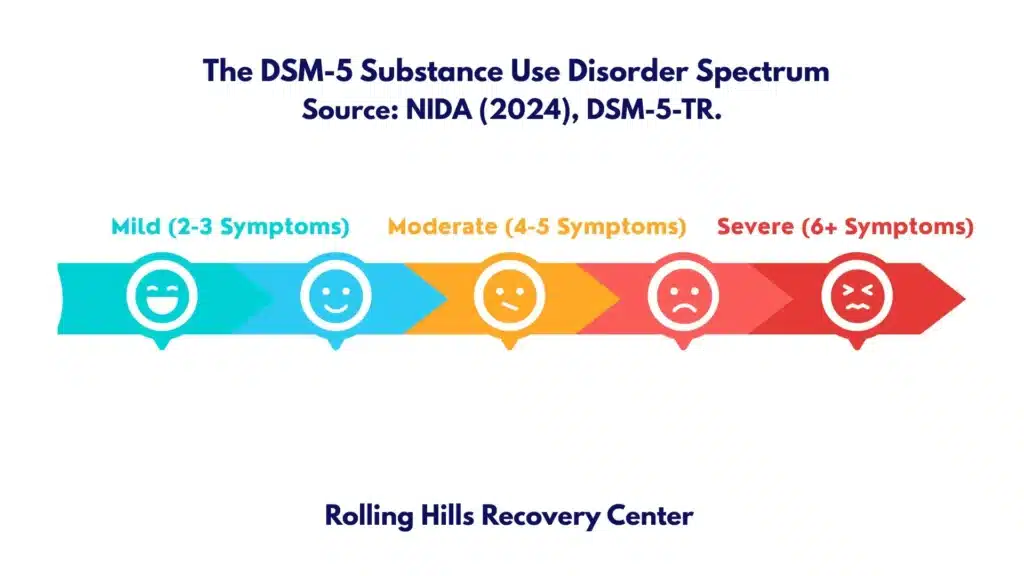
- Mild: 2–3 criteria
- Moderate: 4–5
- Severe: 6 or more
Examples of criteria include using more or longer than intended, unsuccessful attempts to cut down, cravings, role failures, hazardous use, tolerance, and withdrawal. The formal criteria can be reviewed in resources from the National Institute on Drug Abuse (NIDA) and the American Society of Addiction Medicine (ASAM).
- NIDA overview: https://nida.nih.gov/publications/drugfacts/understanding-drug-use-addiction
- ASAM definition of addiction: https://www.asam.org/quality-care/definition-of-addiction
Tolerance and Withdrawal
- Tolerance: needing more of the substance to get the same effect or reduced effect with the same amount.
- Drug and alcohol withdrawal: a predictable set of physical and mental symptoms that occur when use is reduced or stopped (e.g., opioid withdrawal can cause muscle aches, diarrhea, yawning; alcohol withdrawal may cause tremor, anxiety, seizures).
Tolerance and withdrawal indicate physical dependence, which can happen with or without addiction. Addiction includes loss of control & continued use despite harm.
Core Neurobiology in Brief
- Reward and salience: Addictive drugs increase dopamine signaling in mesolimbic pathways (ventral tegmental area to nucleus accumbens), tagging the substance and cues as highly “important” (salient).
- Learning and memory: Repeated use strengthens associations between cues, stress, and drug relief; habits form.
- Stress systems: The brain’s anti-reward system (e.g., CRF, dynorphin) ramps up with repeated use, increasing negative mood and stress, which drives more use.
- Prefrontal control: Chronic use can reduce top-down control from the prefrontal cortex, making it harder to resist cues or delay reward.
- Result: Compulsion and craving persist even when a person knows the risks. Treatment aims to restore balance through medications, psychotherapy, structure, and support.
Global and national health agencies treat SUD as a health condition that responds to care, not as a character flaw. See World Health Organization (WHO): https://www.who.int/health-topics/substance-abuse
Signs and Symptoms to Recognize
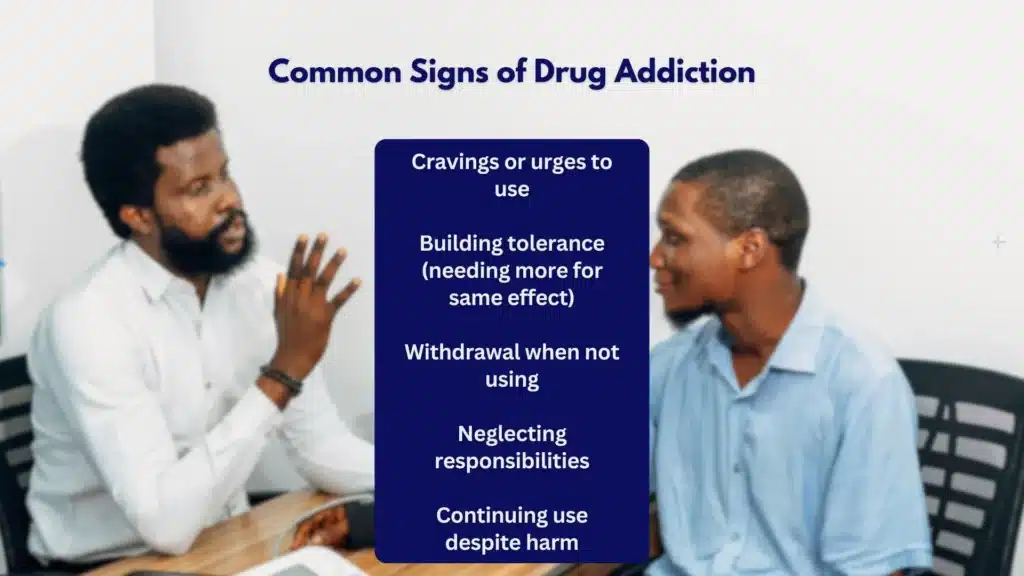
Impaired Control and Cravings
- Using more or longer than intended
- Unsuccessful attempts to cut down or stop
- Persistent cravings or urges to use
- Episodes of binge use or “lost time” around substance use
Quick how-to check (informal, not a diagnosis):
- Ask: “Have you tried to cut down but couldn’t?” and “Do cravings interfere with your day?”
- Note any regular morning use or use to “feel normal” after withdrawal symptoms.
- Consider frequency and amount vs. what you planned to use.
Time Spent, Role Failures, and Social Problems
- A lot of time spent obtaining, using, and recovering
- Missing work, school, or family responsibilities
- Relationship conflict, isolation, or withdrawal from hobbies
- Continued use despite knowing it worsens anxiety, pain, or sleep
Some people maintain jobs and family roles while meeting SUD criteria; this is often called “functional” use. It still carries real risks and often masks symptoms. Learn more about a functional addict pattern and what to watch for.
Risky Use and Dependence Physiology
- Using in hazardous situations (e.g., driving, mixing sedatives)
- Continued use despite medical problems (e.g., ulcers, asthma, arrhythmia)
- Tolerance and withdrawal, as noted above
Red flags for severe dependence:
- Morning shakes or sweats relieved by a drink or pill
- Blackouts with alcohol
- Using opioids or benzodiazepines to cope with withdrawal from the other
- Escalating doses or switching to higher-potency formulations (e.g., fentanyl)
Polysubstance Patterns and Overdose Red Flags
Polysubstance use, such as combining opioids with benzodiazepines, alcohol, or stimulants, raises overdose risk.
Red flags:
- Using alone
- Rapidly changing drug supply or unknown source (street pills)
- Needles or paraphernalia plus sedatives or alcohol
- Blue lips, snoring/gurgling breathing, pinpoint pupils
- Unresponsiveness
Immediate action:
- Call 911
- Administer naloxone if an opioid overdose is suspected
- Stay until help arrives
Find overdose data and prevention basics at the CDC: https://www.cdc.gov/drugoverdose/index.html
Causes and Risk Factors
Genetic Vulnerability and Early Initiation
- Genetics: 40–60% of risk is inherited. Variants affect reward pathways, metabolism, impulsivity, and stress response.
- Early initiation: The earlier the regular use (especially before age 15), the higher the lifetime risk of SUD and severity. Developing brains are more sensitive to drug effects and cue learning.
Practical step: delay initiation and limit access in the home. Store medications locked; dispose of unused prescriptions at take-back locations.
Trauma, Adverse Childhood Experiences, and Co‑Occurring Disorders
- Trauma and ACEs: Physical or sexual abuse, neglect, household substance use, and violence increase SUD risk. Substances often become coping tools.
- Mental health disorders: Anxiety, depression, bipolar disorder, PTSD, ADHD, and psychotic disorders commonly co-occur with SUD. Treat both together for better outcomes.
- For example, see how attention symptoms intersect with substance risk in our overview on ADHD and addiction.
How to screen:
- Ask about mood, sleep, panic, and trauma symptoms.
- If present, plan integrated care, medication, and therapy that address both conditions.
Potency, Availability, and Social Determinants
- High-potency formulations: Fentanyl, xylazine-adulterated opioids, high-THC cannabis concentrates, and stimulant adulterants increase compulsion and medical risk.
- Availability and exposure: Peer use, local supply, and exposure to targeted marketing affect initiation and relapse.
- Social determinants: Housing instability, unemployment, food insecurity, and limited access to care drive both onset and persistence.
Simple supports that help:
- Stable housing
- Reliable transportation to treatment
- Supportive employment policies and benefits
Stress, Sleep, Progression, and Relapse Risk
- Chronic stress and sleep disruption are both triggers and outcomes; they worsen cue reactivity.
- Progression: Use may start intermittently, progress to habitual use, then compulsive patterns. Relapse often occurs during high-stress transitions.
- Risk is dynamic: it changes with life events, psychiatric symptoms, pain, and environment.
Skill-building targets:
- Sleep routine (same wake time, light exposure in the morning)
- Daily stress unload (10 minutes of breath work or gentle movement)
- Structured time blocks around known triggers
Health Consequences and Complications
Overdose and Poisoning
- Opioids: respiratory depression, hypoxia, brain injury, death
- Stimulants: arrhythmia, stroke, hyperthermia
- Sedatives and alcohol: central nervous system depression; with opioids, risk rises sharply
- Unknown contaminants: adulterants increase toxicity and reduce response to standard care
Basic prevention:
- Never use alone; test a small amount first
- Carry naloxone; teach family how to use it
- Avoid mixing sedatives with opioids or alcohol
Infections: HIV, Hepatitis, and Others
- Blood-borne infections: HIV, hepatitis B, and C via shared needles or equipment
- Skin and soft tissue: abscesses, cellulitis
- Endocarditis: heart valve infection from bloodstream bacteria
- Respiratory infections from smoking or vaping
Harm reduction approaches (clean supplies, vaccination, and testing) reduce these harms.
Cardiovascular, Pulmonary, Liver, and Kidney Injury
- Stimulants: hypertension, coronary spasm, cardiomyopathy, stroke
- Alcohol: fatty liver, hepatitis, cirrhosis, pancreatitis; hypertension
- Opioids: hypoxemia, sleep-disordered breathing, pulmonary edema
- Inhaled drugs: COPD, asthma exacerbations, pneumonitis
- Kidney injury: rhabdomyolysis, dehydration, contaminants
Cognitive and Mood Changes, Pregnancy Risks
- Cognitive: attention and memory problems, executive dysfunction; some improve with sustained abstinence and sleep recovery
- Mood: irritability, depression, anxiety; substance-induced mood disorder may blur with primary mental health conditions
- Pregnancy: miscarriage, low birth weight, neonatal abstinence syndrome, preeclampsia; prenatal care plus medication treatment improves outcomes
Legal and Occupational Harm, Stigma, and Barriers to Care
- Legal: DUI, possession, probation violations, child custody
- Occupational: discipline, loss of license or job; missed opportunities
- Stigma: internalized shame, fear of losing employment, biased care; all reduce help-seeking
- Barriers: cost, transportation, childcare, lack of insurance clarity
If cost is a barrier, learn how benefits apply to treatment and parity protections. See options for insurance coverage for drug rehab.
Assessment, Treatment, and Recovery

At Rolling Hills Recovery Center in New Jersey, licensed clinicians combine evidence-based care and holistic supports (sleep, nutrition, movement, mindfulness). Care is individualized and trauma-informed. The goal is lasting stability and better life functioning.
Screening Tools and Drug Testing Basics
Common screening tools used in primary care and specialty settings:
- ASSIST (WHO Alcohol, Smoking and Substance Involvement Screening Test): identifies risk across substances; WHO resource: https://www.who.int/teams/mental-health-and-substance-use/alcohol-drugs-and-addictive-behaviours/assist
- AUDIT (Alcohol Use Disorders Identification Test): for alcohol risk and probable AUD
- DAST‑10 (Drug Abuse Screening Test): brief screen for drug-related problems
- NIDA Quick Screen: 1–4 questions followed by ASSIST if positive; NIDA resource: https://nida.nih.gov/sites/default/files/pdf/nmassist.pdf
How to start screening (step-by-step):
- Ask permission: “Would it be okay if I ask a few routine questions about alcohol and drug use to support your health?”
- Use a validated tool (AUDIT for alcohol; DAST‑10 or ASSIST for drugs).
- If positive, ask about goals and readiness to change.
- Offer brief advice, schedule follow-up, and discuss treatment options. Provide naloxone if opioid use is present or suspected.
Drug testing basics (used clinically to inform care, not to punish):
- Specimens: urine (most common), saliva (short window), blood (rare), hair (long window, less specific)
- Windows of detection vary by drug, dose, frequency, and metabolism
- False positives and negatives happen; confirmatory testing (GC/MS) is sometimes needed
- Always combine results with clinical interview and collateral history
Template: simple shared monitoring plan
- Frequency: weekly for 4 weeks, then biweekly if stable
- Randomization: 24-hour notice window
- Transparency: review results together in session
- Response: adjust care, not blame; focus on safety
Levels of Care and Withdrawal Management
Care is matched to severity, stability, and environment.
- Outpatient (OP): 1–3 sessions/week; suitable for mild to moderate SUD with strong supports
- Intensive Outpatient (IOP): 9+ hours/week; structure without 24/7 care
- Partial Hospitalization (PHP): ~20 hours/week; daily groups and medical oversight
- Residential/Inpatient: 24-hour structured environment; ideal for unsafe home settings or high relapse risk
- Medically Managed Withdrawal (detox): short-term stabilization for alcohol, benzodiazepines, or opioids with medical monitoring
How to choose a level (simple process):
- Assess safety: suicide risk, medical complications, pregnancy, housing
- Identify withdrawal risks: alcohol and benzodiazepine withdrawal can be dangerous; plan a medical taper
- Consider supports: family, employer flexibility, transportation
- Step up or down: move between levels as stability changes
FDA‑Approved Medications
Medications reduce cravings, normalize brain circuits, and lower overdose risk. They can be used short- or long-term, and combined with therapy.
Medication comparison (simplified):
| Medication | For | How it works | Key benefits | Key cautions/notes |
|---|---|---|---|---|
| Buprenorphine (SL/monoproduct or with naloxone) | Opioid use disorder | Partial opioid agonist; stabilizes receptors | Lowers overdose risk; office-based; flexible dosing | Must be dispensed by a certified opioid treatment program; QTc monitoring |
| Methadone | Opioid use disorder | Full agonist; daily dosing in OTP | Strong retention; effective in long-term OUD | Avoid in cardiac disease or severe hepatic disease; requires abstinence before starting |
| Naltrexone (oral or XR injection) | Opioid use disorder & alcohol use disorder | Opioid antagonist; blocks effects/reduces reinforcing effects | Non-addictive; monthly injection option | Requires full detox from opioids; avoid in acute hepatitis or liver failure |
| Acamprosate | Alcohol use disorder | Modulates glutamate/GABA | Supports abstinence; renally cleared | TID dosing; adjust in renal impairment |
| Disulfiram | Alcohol use disorder | Blocks aldehyde dehydrogenase (aversive reaction with alcohol) | Useful with supervised dosing & committed patients | Avoid in cardiac disease or severe hepatic disease; requires abstinence before start |
Medication selection is individualized. The evidence base is strong for methadone and buprenorphine in OUD and naltrexone or acamprosate in AUD. See NIDA and ASAM guidance above for best practices.
Evidence‑Based Therapies
- Cognitive Behavioral Therapy (CBT): Identify triggers, thoughts, and routines; build coping and problem-solving skills.
- Motivational Interviewing (MI): Strengthens motivation and readiness; aligns care with the person’s goals.
- Contingency Management (CM): Reinforces sobriety and healthy behaviors with tangible incentives.
- Family therapy (e.g., CRAFT, multidimensional family therapy): Enhances communication, boundaries, and support.
- Trauma-informed care: Addresses trauma symptoms safely.
- Peer support: 12-step, SMART Recovery, and other mutual-help groups.
At Rolling Hills Recovery Center, clinical care is paired with holistic supports, sleep optimization, nutrition, movement, stress skills, because those daily levers reduce cravings and relapse risk.
Harm Reduction and Overdose Planning
Harm reduction saves lives and can be a bridge to treatment.
- Naloxone: Carry and train loved ones; available without a prescription in many pharmacies
- Fentanyl test strips: May detect fentanyl in powders or pills; reduces risk when used correctly
- Safer use: Don’t use alone; avoid mixing opioids with alcohol or benzodiazepines; start with a test dose
- Vaccinations: Hepatitis A and B; influenza and pneumococcal if indicated
- Safer supplies and disposal: Use sterile equipment; dispose of sharps safely; secure medications
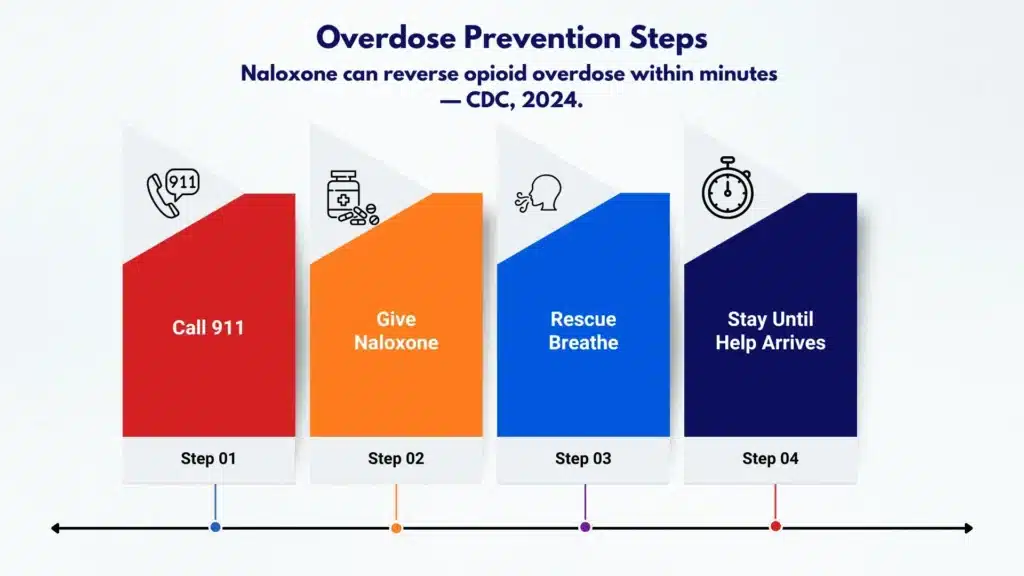
Overdose plan template (keep it visible):
- If unresponsive or slow breathing: call 911 immediately
- Give naloxone: 4 mg intranasal; repeat in 2–3 minutes if needed
- Rescue breathing: 1 breath every 5–6 seconds if not breathing
- Stay until help arrives; place in recovery position if breathing resumes
Relapse Prevention, Aftercare, and Community Supports
Relapse prevention is a skill set that can be learned. It includes triggers, tools, and a weekly structure that keeps recovery active.
Core skills:
- Identify top 5 triggers: people, places, feelings, times of day, paydays
- Build a coping menu: phone a support, 10-minute walk, urge surfing, delay-use plan (wait 30 minutes then reassess)
- Craving plan: hydrate, eat, move, call; avoid HALT (hungry, angry, lonely, tired)
- Sleep, nutrition, and movement: Routine aids mood stability and reduces cue reactivity
Simple craving card template (carry it):
- My 3 biggest triggers are: ________ / ________ / ________
- If I get an urge, I will: 1) text/call ________ 2) drink water & step outside 3) set a 10-minute timer & breathe
- If I slip, I will: contact my clinician and attend the next group; no shame, reset
Aftercare and support:
- Step-down aftercare and relapse prevention: IOP to OP; continue meds if helpful
- Mutual-help: AA/NA, SMART Recovery, Refuge Recovery; attend at least weekly early on
- Family involvement: education, boundaries, support without enabling; family sessions improve outcomes
- Employer involvement: When safe, coordinate leave or accommodations, prioritize recovery activities around work
For individuals with workplace or licensing concerns, clinicians can help document participation and progress. Recovery is not linear, and small adjustments, like schedule changes or remote visit options, reduce relapse risk.
Practical Tools You Can Use Today
- Self-check: Take AUDIT for alcohol and DAST‑10 for drugs; bring results to your clinician. If you’re unsure how to score, ask your provider to review them with you.
- Sleep reset (7 days):
- Fixed wake time
- 30–60 minutes of morning light
- No caffeine after noon
- 10-minute wind-down in the evening
- 72-hour recovery plan:
- Day 1: Remove substances and paraphernalia; set up naloxone at home; schedule first appointment
- Day 2: Tell one trusted person; attend one support meeting; write my craving plan
- Day 3: Walk 20 minutes; prepare two simple meals; secure rides to treatment
- Safety checklist:
- Naloxone is accessible and family trained
- Avoid mixing sedatives and alcohol/opioids
- Do not use alone; test dose first if using
- Documentation template for appointments:
- What went well this week: ________
- Cravings (0–10): ________; triggers: ________
- Any use? How much/when: ________
- Medication effects/side effects: ________
- Questions for my clinician: ________
How Rolling Hills Recovery Center Supports Care in New Jersey
- Comprehensive assessment: medical, psychiatric, and social needs
- Medication‑assisted treatment for opioids and alcohol; careful monitoring
- Therapies: CBT, MI, CM, and family sessions
- Holistic supports: sleep, nutrition, movement, mindfulness training
- Flexible levels of care: outpatient through higher-intensity programming as clinically indicated
- Coordination with families and employers when requested to support stability
For individuals balancing work, school, or caregiving, plans are tailored to maintain life responsibilities while strengthening recovery.
Frequently Asked Practical Questions
Is Addiction a Disease or a Choice?
There is a choice in the first use for many people; over time, brain and behavior changes reduce control and increase compulsion. The medical model is supported by ASAM and NIDA. It is a treatable disease, and people recover every day.
Do Medications Just “Replace One Drug with Another”?
No. Medications like buprenorphine and methadone stabilize receptors, cut cravings, and reduce overdose risk. They improve work, parenting, and health outcomes. Dose and duration are individualized. Naltrexone is a non‑addictive option for some.
How Long Does Treatment Last?
It varies. Many benefit from at least 3–6 months of structured care and 12 months of medication support for OUD. Some continue medications longer. The right length is the one that keeps you safe, working, and well.
What About Privacy?
Substance use treatment is protected by HIPAA and, in many cases, 42 CFR Part 2. With your consent, clinicians can coordinate with family and employers to support your recovery and accommodations, but you remain in control of disclosures.
When Urgent Help is Needed
- Alcohol withdrawal warning signs: tremor, sweating, anxiety, elevated heart rate, seizures, and hallucinations. Seek medical care promptly, as complicated withdrawal can be life‑threatening.
- Benzodiazepine withdrawal: similar risks; requires slow, supervised taper.
- Opioid overdose: unresponsive, slow or no breathing, bluish lips/fingertips, administer naloxone and call 911.
- Suicidal thoughts or risk of harm: go to the nearest emergency department or call emergency services.
How to Take the First Step
- Schedule an assessment: A clinician will review health history, withdrawal risk, mental health, and goals.
- Prepare for your visit:
- List substances, amounts, and times
- Current medications and allergies
- Past treatment, what helped and what didn’t
- Insurance details or payment questions
- Ask about:
- Medications for your specific substance pattern
- Level of care that fits your life
- How family can be involved
- Aftercare plan from the start
Rolling Hills Recovery Center’s team in New Jersey works to reduce friction at each step, from quick screening to stable aftercare. The aim is durable change, better health, and a life that feels worth protecting.
Conclusion
Addiction is a medical condition, treatable with the right plan. Key points: watch for cravings and loss of control; medicines plus counseling work; harm reduction saves lives. Recovery grows with steady support & aftercare.
Frequently Asked Questions (FAQs)
What is Addiction to Drugs, and Why is it Considered a Brain Disease?
Drug addiction (in clinical terms) is a chronic medical condition in which substance use becomes compulsive despite harm.
Brain reward, stress, and self‑control circuits change over time; this is why cravings, tolerance, and withdrawal appear and why relapse can occur.
It is not a moral failing. With the right plan, assessment, medications & counseling, steady support, people recover.
What Are the Early Signs & Symptoms of Drug Addiction to Watch for?
Common signs include stronger cravings, using more or longer than planned, failed cut‑down attempts, spending a lot of time getting or using, and giving up activities.
Physical changes like tolerance and withdrawal, sleep shifts, mood swings, and secrecy are frequent. Risky use (driving, mixing drugs, using alone) and role problems at school or work also matter.
Red flags for overdose: slowed or stopped breathing, blue lips, unresponsiveness, call 911 now.
What Risks Come with Drug Addiction if it is Not Treated?
Risks include overdose, infections, and organ injury (heart, liver, kidneys). Mental health symptoms often worsen. Potent synthetic opioids like fentanyl raise poisoning risk, especially when mixing substances.
Pregnancy complications can occur. Legal, financial, and relationship strain grows. Early, evidence‑based treatment lowers these risks & improves long‑term health.
What is Treatment Like Day to Day, and How Can Someone Get Started?
Expect a structured plan: medical check‑ins, therapy sessions, skills practice, and medication as indicated. Sleep, meals, movement, and stress tools are built in; small wins count. To start:
• Schedule a medical evaluation; do not abruptly stop heavy alcohol or benzodiazepines due to withdrawal risk.
• Carry naloxone if opioids are involved; teach family how to use it.
• Reduce triggers at home, set a simple safety plan, and line up support (one trusted person is enough to begin).
• Contact Rolling Hills Recovery Center to arrange an assessment and talk through level of care options.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












