Choosing a drug rehab center in New Jersey can feel overwhelming. This overview breaks down what programs offer, how care levels differ, what evidence-based therapies and medications look like, and how insurance & costs work. It also explains intake, detox, aftercare, and safety standards so families can make informed, medically sound decisions.
Key Takeaways
- Care should match need: safe medical detox when needed (24/7), then inpatient or residential, PHP, IOP, or outpatient using ASAM Criteria.
- Safety & evidence matter: CBT, DBT, motivational interviewing, plus MAT for alcohol and opioid use (buprenorphine, methadone via OTP, naltrexone). Integrated mental health care.
- In New Jersey, check quality: NJ license, accreditation by The Joint Commission or CARF; clear withdrawal protocols (CIWA, COWS), physician oversight & masters-level clinicians; avoid guaranteed cures
- Plan costs and access early: verify insurance benefits, prior authorization, deductibles, and copays; NJ FamilyCare/Medicaid options; ask for an itemized estimate, consider FMLA or short-term disability, and transport needs.
What Local Drug Rehab Programs Offer
Settings and Levels of Care
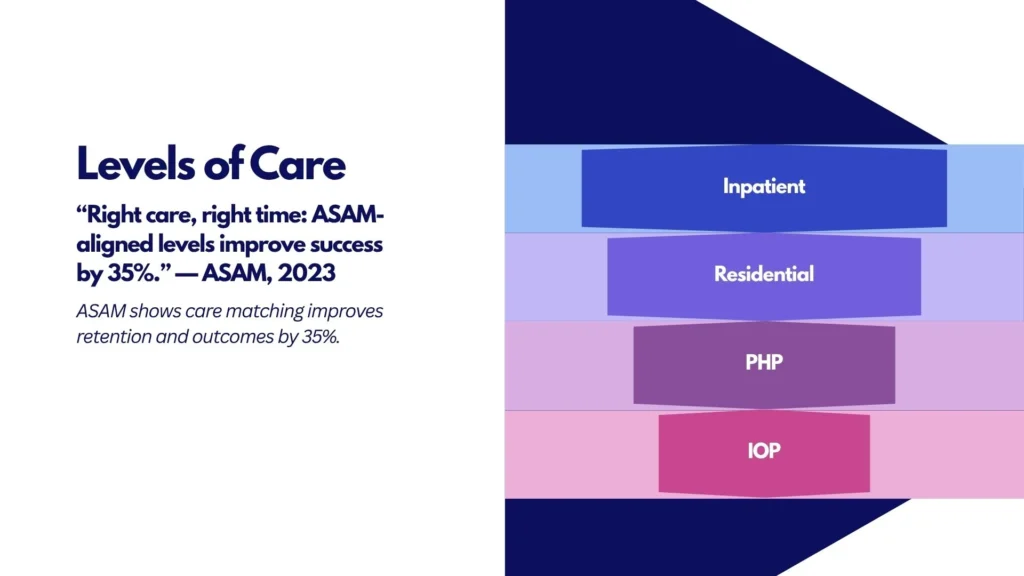
Local rehab facilities in New Jersey typically organize services by level of care, matching the intensity of treatment to clinical need using ASAM Criteria. This “right care, right time” model improves safety and outcomes.
| Level of care | Setting | Yes, medically managed | Who it’s for | Detox/withdrawal management |
|---|---|---|---|---|
| Inpatient (ASAM 4.0) | Hospital-based, 24/7 medical | Continuous | Severe withdrawal risk; medical or psychiatric instability | Yes, medically managed |
| Residential (ASAM 3.1–3.7) | Non-hospital, 24-hr support | Continuous | Moderate–severe SUD needing structure & safety | Some residential programs provide on-site withdrawal management (3.7-WM) |
| Partial Hospitalization, PHP (ASAM 2.5) | Day treatment, go home at night | ~20+ hrs/week | Step-down from higher care or high-intensity start | No acute detox; can start/continue MAT |
| Intensive Outpatient, IOP (ASAM 2.1) | Clinic or telehealth | ~9–19 hrs/week | Moderate SUD, stable housing/support | No detox; close monitoring with MAT |
| Outpatient, OP (ASAM 1.0) | Clinic or telehealth | ≤8 hrs/week | Mild SUD, maintenance/relapse prevention | No detox; medication follow-up |
Note: Many centers offer flexible scheduling (days, evenings, weekends) and blended in-person plus telehealth. For alcohol-specific outpatient support, read our article on outpatient alcohol rehab in New Jersey.
Programs like Rolling Hills Recovery Center align care with ASAM levels, so a person may start in one level and step up or down as needs change.
Medical Detox and Stabilization
Withdrawal management should be safe, measured, and specific to the substance(s) involved.
- Alcohol or benzodiazepines: Use validated tools such as CIWA-Ar for alcohol. Protocols may include benzodiazepines, anticonvulsants, thiamine, fluids, and close vitals monitoring. 24/7 nursing and physician oversight are expected for higher-risk cases.
- Opioids: Use COWS for symptom scoring. Buprenorphine initiation is common; methadone via an OTP; adjunct medications (e.g., clonidine, antiemetics) as needed. Continuous assessment for respiratory depression, dehydration, and co-use of sedatives.
- Stimulants: No FDA-approved detox medications, but symptom-focused care (sleep, hydration, nutrition) and monitoring for mood or psychosis.
- Polysubstance: Plan for overlapping risks, especially if alcohol, benzos, or opioids are combined.
Detox is a starting point, not a standalone treatment. A warm handoff into ongoing care reduces relapse risk.
Evidence-Based Therapies
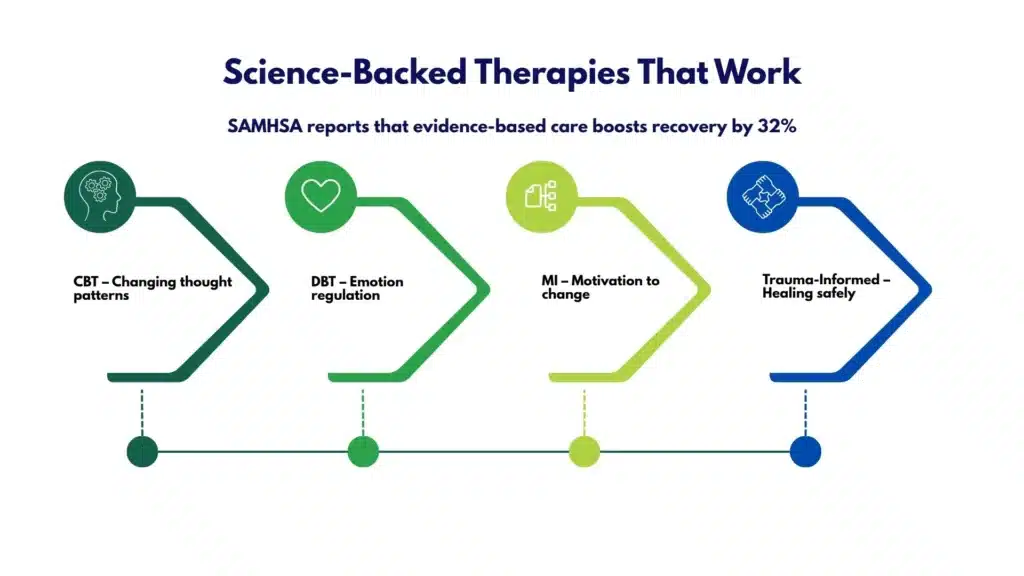
Effective programs depend on interventions that have research support:
- Cognitive Behavioral Therapy (CBT): Restructure thinking patterns, build coping skills, and practice relapse-prevention tools.
- Dialectical Behavior Therapy (DBT) skills: Distress tolerance, emotion regulation, and interpersonal effectiveness for high-emotion states.
- Motivational Interviewing (MI): Nonjudgmental style to strengthen personal motivation & commitment to change.
- Trauma-informed care: Prioritize safety and pacing; EMDR or other trauma therapies when appropriate and after stabilization.
- Family therapy: Educate loved ones, set healthy boundaries, and improve support systems.
- Contingency management principles: Behavioral incentives to reinforce treatment goals, implemented within legal and ethical guidelines.
- Peer support services: Recovery coaching to improve engagement and continuity.
Holistic services, mindfulness, exercise, and nutrition counseling can complement (not replace) therapy. Rolling Hills Recovery Center incorporates both evidence-based and holistic approaches to support the whole person.
Medication-Assisted Treatment (MAT) for Alcohol or Opioid Use Disorder
MAT should be offered and discussed with every eligible patient, with shared decision-making, informed consent, and ongoing monitoring.
- Opioid Use Disorder (OUD):
- Buprenorphine: Office-based initiation and maintenance; reduces cravings and overdose risk.
- Methadone: Dispensed through a certified Opioid Treatment Program (OTP); effective for long-acting stabilization.
- Naltrexone (oral or extended-release): Requires full detox; blocks opioid effects.
- Alcohol Use Disorder (AUD):
- Naltrexone (oral or XR): Reduces heavy drinking days and cravings.
- Acamprosate: Supports abstinence maintenance, particularly post-detox.
- Disulfiram: Deterrent for motivated patients with supervision.
Clinician monitoring includes liver/kidney function checks when indicated, medication interactions, pregnancy considerations, and consistent safety planning (including naloxone for those at opioid risk).
Co-Occurring Mental Health Support
Substance use disorders often overlap with mood, anxiety, PTSD, ADHD, or other conditions. Quality programs provide:
- Psychiatric evaluation and medication management
- Integrated treatment planning (not “parallel” or siloed)
- Suicide risk screening and safety plans
- Coordination with primary care for medical conditions
- Access to specialized tracks (e.g., women, veterans, LGBTQ+, trauma-focused)
Rolling Hills Recovery Center treats dual-diagnosis disorders within the same plan, which tends to improve stability and reduce returns to use.
Licensure and Accreditation Expectations in New Jersey
When considering any NJ facility, expect the following:
- State licensure by the NJ Department of Human Services, Division of Mental Health and Addiction Services (DMHAS). Regulations for substance use treatment include N.J.A.C. 10:161A (residential) and N.J.A.C. 10:161B (outpatient).
- Accreditation by The Joint Commission or CARF. Accreditation shows external review of safety, quality, and continuous improvement.
- ASAM-aligned level-of-care placement and continued-stay review.
- For methadone, OTP certification by SAMHSA, plus DEA registration and state approval.
Facilities should display licensure and accreditation status, and be open about policy and outcomes.
How to Evaluate Quality in New Jersey
Use this quick checklist to assess any local program:
- Verify NJ licensure (DMHAS) and ask for accreditation (The Joint Commission or CARF).
- Ask which ASAM levels are offered and how level-of-care decisions are made.
- Confirm 24/7 medical coverage in detox and the specific withdrawal protocols (alcohol, opioids, benzos).
- Review staff credentials:
- Physician medical director with addiction experience
- Masters-level clinicians (LCSW, LPC, LMFT) and licensed/certified alcohol and drug counselors (e.g., LCADC, CADC)
- Nurses experienced in withdrawal management
- Look for integrated psychiatric care and co-occurring disorder capability.
- Medication services: Buprenorphine, methadone via OTP referral or on-site if an OTP, naltrexone, and evidence-based AUD medications.
- Safety policies: Urgent response procedures, infection control, medication storage, and overdose prevention, including naloxone availability.
- Privacy practices: HIPAA compliance, clear consent forms for family communication.
- Family involvement options with patient consent: education sessions, structured family therapy.
- Outcomes monitoring: standardized measures (e.g., retention, symptom scales, quality of life) and post-discharge follow-up.
- Ethical billing: Plain-language estimates, utilization review transparency, no surprise charges.
Red flags to avoid:
- Promises of a “cure” or 100% success rates
- Vague pricing; pressure to provide credit card details before clinical screening
- No physician oversight in detox; no MAT options
- One-size-fits-all programs without individualized plans
- No aftercare planning or refusal to coordinate care with your other providers
Access, Costs, and Insurance

Getting care funded can feel complex. Here’s a practical, step-by-step approach:
- Verify your benefits first
- Call your insurer using the member services number on your card. Ask:
- Behavioral health coverage for substance use treatment
- Deductible met to date; out-of-pocket max
- Copays and coinsurance by level of care (detox, inpatient, residential, PHP, IOP, outpatient)
- In-network programs near your ZIP code
- Prior authorization requirements
- Many centers can verify for you in minutes. For details specific to New Jersey, see insurance coverage for drug rehab in NJ.
- Call your insurer using the member services number on your card. Ask:
- Understand in-network vs. out-of-network
- In-network often means lower out-of-pocket costs and easier authorization.
- Out-of-network can still be viable depending on your plan; ask for single-case agreement options if a specific program is clinically indicated.
- NJ FamilyCare/Medicaid and parity protections
- NJ FamilyCare covers many levels of SUD care; benefits vary by managed care plan.
- Federal & state parity laws require coverage for mental health/substance use to be comparable to medical/surgical benefits.
- Prior authorization and medical necessity
- Most insurers require authorization for detox and higher levels of care. The program should handle clinical documentation aligned with ASAM Criteria.
- Deductibles, copays, and coinsurance
- Ask for a “good-faith estimate” of your total costs at each level of care, including lab fees, medication costs, and professional fees.
- FMLA and short-term disability
- Many patients qualify for protected leave under the Family and Medical Leave Act (FMLA). Your clinician can provide documentation. Short-term disability may help replace part of your income during treatment.
- Transportation and logistics
- Ask about transportation to and from treatment, especially for PHP/IOP. Programs may help coordinate rides or telehealth.
- What to ask admissions to estimate the total cost
- Which services are included vs which are billed separately?
- Are labs, medications, and specialty consults included?
- What is the average length of stay at each level?
- If a step-up in care is needed, how will billing change?
Tip: Keep photos of your insurance card (front/back), a list of medications, allergies, and prior authorizations. Having these ready speeds admission.
Intake, Detox & Treatment Pathways
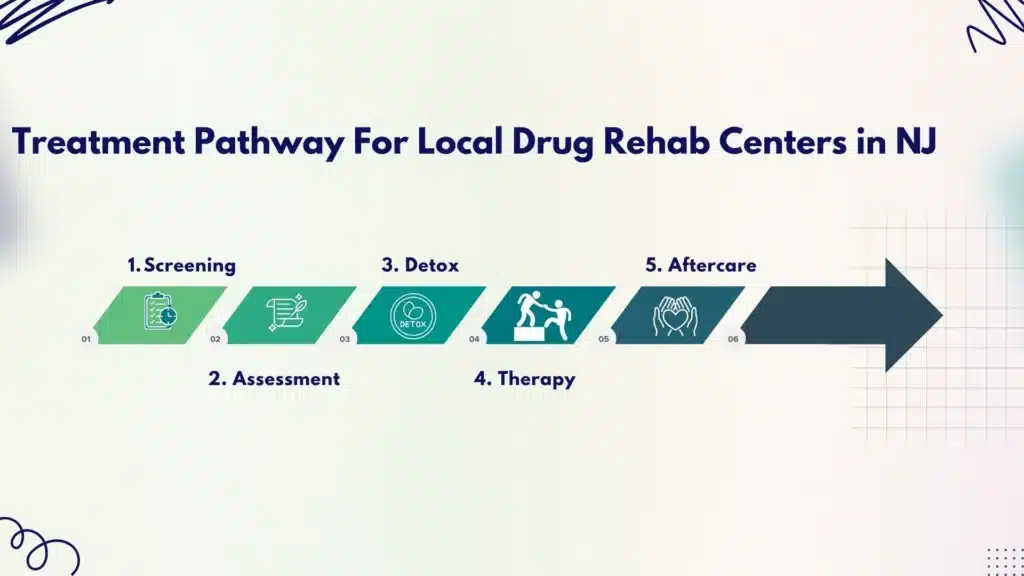
A reliable pathway is structured but flexible. Expect the following steps.
Step 1: Screening and Pre-Admission
- Brief phone screen covering substances, last use, withdrawal history, medical/psychiatric conditions, and safety risks.
- Insurance verification and scheduling. If urgent, same-day or next-day assessment is common.
Step 2: Assessment Upon Arrival
- Biopsychosocial interview using DSM-5 criteria for substance use disorders
- Physical exam, vitals, review of systems, and medication reconciliation
- Labs as indicated (CBC, CMP, liver enzymes, hepatitis/HIV screening with consent, pregnancy test when relevant)
- Withdrawal risk scoring: CIWA-Ar, COWS, or benzodiazepine risk evaluation
- Suicide risk and violence risk assessment; safety planning
- ASAM level-of-care determination and initial treatment plan
Step 3: Stabilization and MAT Initiation
- Alcohol/benzo withdrawal protocol with close monitoring; thiamine before glucose if alcohol use disorder is suspected
- Opioid withdrawal protocol; buprenorphine induction when COWS indicates moderate withdrawal; methadone referral/coordination with an OTP if that’s the best fit; naltrexone considered after detox for appropriate candidates
- Begin overdose education and provide naloxone on-site or at discharge for those at risk
Step 4: Core Therapies and Dose of Treatment
- PHP: Typically 5 days/week, ~20–30 hours weekly, combining groups, individual therapy, medical visits, and skills practice
- IOP: 3–5 days/week, ~9–15 hours; group therapy, weekly individual counseling, and medication management as needed
- Outpatient: Weekly 1–2 sessions for ongoing therapy or medication follow-up
- Individual therapy every 1–2 weeks minimum; more often early in care
- Family sessions (with patient consent) to improve support and reduce relapse risk
Content areas commonly covered:
- Craving management and relapse prevention planning
- Coping skills, mood, and anxiety management
- Sleep hygiene and nutrition
- Trauma-informed stabilization skills
- Vocational or educational support
- Legal and social services navigation, if needed
Step 5: Estimated Timelines
- Detox/withdrawal management: 3–7 days on average (varies by substance and medical status)
- Residential: Often 2–4 weeks, sometimes longer, based on need
- PHP: 1–3 weeks
- IOP: 4–12 weeks
- Outpatient/continuing care: months, sometimes longer
Timeframes are individualized; the best predictor is clinical progress, not the calendar.
Step 6: Step-Down Progression and Aftercare Handoff
- Movement between levels is based on ASAM continued-stay criteria, safety, and functioning
- A complete aftercare plan is created before discharge, with appointments scheduled and transportation considered
- Warm handoffs to providers (direct communication, records sent with consent)
Programs like Rolling Hills Recovery Center coordinate these transitions to reduce gaps that can lead to return-to-use.
Aftercare, Relapse Prevention, and Community Supports
Strong aftercare reduces relapse risk and supports long-term recovery.
- Discharge plan with appointments in hand
- Primary care, psychiatry, therapy, and recovery support are scheduled prior to discharge
- Medication bridge scripts and follow-up dates confirmed
- Relapse warning signs to watch for
- Increasing isolation, skipping appointments, sleep disruption, romanticizing past use, sudden stressors, and stopping medications
- Encourage early outreach to the care team if warning signs appear
- Recovery housing considerations
- Ask about sober living options, house rules, drug testing, curfews, transportation, and costs
- Choose homes that coordinate with your outpatient team
- Peer support options
- 12-step meetings (AA/NA) or secular options like SMART Recovery
- Peer recovery coaches can support accountability and linkage to services
- Telehealth check-ins
- Virtual therapy or medication follow-ups help maintain momentum, especially during work or school
- Overdose prevention and naloxone training
- Everyone at risk of opioid exposure should receive naloxone and training; family/friends too
- Return-to-use plan (a simple, written plan)
- If substances are used, who to call first?
- What steps restore safety and stabilize quickly? (e.g., same-day IOP visit, MAT appointment)
- Remove drugs/paraphernalia, update coping strategies, and review triggers with your therapist
- No shame—treat return-to-use as a signal to adjust care
- Community resources in New Jersey
- County mental health/addiction boards, recovery community centers, transportation assistance, legal aid, and vocational training programs
- NJ’s DMHAS site lists hotlines and regional providers
Special populations
- Women may benefit from gender-responsive groups addressing trauma, parenting, and perinatal needs; for local guidance, read our article on women’s drug rehab in New Jersey.
- Veterans often benefit from trauma-informed, military-culture-competent care and VA coordination; programs like drug rehab for veterans in NJ align services with VA benefits and community supports.
Tools, Templates, and Helpful References
Use these practical tools to speed decisions and improve safety.
Quick “What Level of Care Fits Me Right Now?” Checklist
- Life-threatening withdrawal risk, severe medical/psychiatric instability → Inpatient detox
- Moderate withdrawal risk, not medically fragile → Residential with withdrawal management or closely monitored PHP
- High therapy need but safe at home → PHP
- Need structure but must work or study → IOP
- Stable, focusing on relapse prevention/MAT maintenance → Outpatient
Always confirm with an ASAM-based assessment by a licensed clinician.
Admissions Call Script (Print or Save)
- “I’m seeking treatment for [substance(s)], last use [date/time]. I have [symptoms or risks].”
- “What ASAM levels of care do you offer?”
- “Are you licensed by NJ DMHAS and accredited by The Joint Commission or CARF?”
- “Do you provide MAT (buprenorphine, naltrexone)? How quickly can I start?”
- “Is detox 24/7 with on-site medical coverage?”
- “What is your average schedule and therapy hours per week at each level?”
- “How do you coordinate aftercare and schedule follow-ups before discharge?”
- “Can you verify my insurance benefits today?”
Cost Estimator Questions
- “What is my estimated total out-of-pocket cost per week at PHP, IOP, and OP?”
- “What is billed separately (labs, medications, physician visits)?”
- “If I step up or down in care, how will costs change?”
- “Is transportation available or covered?”
- “What payment plans are available if needed?”
Weekly Treatment Schedule Template (Example)
- Monday: Group therapy (2 hrs), individual therapy (1 hr), medication check (30 min)
- Tuesday: Skills group (2 hrs), family session (1 hr)
- Wednesday: CBT group (2 hrs), peer recovery coaching (30 min)
- Thursday: DBT skills (2 hrs), mindfulness/yoga (1 hr)
- Friday: Relapse prevention group (2 hrs), discharge planning check-in (30 min)
Adjust dose and mix to match your care plan.
Relapse Prevention Plan Template (Fill-In)
- Triggers I will watch for: ______
- Early warning signs: ______
- My top 5 coping skills: ______
- People I will call (with numbers): ______
- Meetings I will attend each week: ______
- Medications I take and when: ______
- Plan if I return to use: call ______, schedule ______, remove substances, attend ______ within 24 hours
Helpful References for Readers
- Treatment locator and helpline
- SAMHSA Treatment Locator
- SAMHSA National Helpline
- Evidence-based care
- New Jersey standards and consumer info
- NJ Department of Human Services: Division of Mental Health and Addiction Services
- Accreditation and level-of-care matching
- The Joint Commission Behavioral Health Care Accreditation (see The Joint Commission site for Behavioral Health standards)
Notes on Safety, Privacy, and Family Involvement
- Safety: Detox should include round-the-clock monitoring when indicated, with clear escalation pathways to higher medical care if needed.
- Privacy: HIPAA-compliant releases allow helpful family involvement while protecting your rights. You choose who gets updates.
- Family: With consent, families can learn about enabling vs support, boundary-setting, and constructive communication. A short family education series often improves outcomes.
How Rolling Hills Recovery Center Fits Locally
As a New Jersey program focused on evidence-based treatment plus holistic supports, Rolling Hills Recovery Center offers:
- Level-of-care alignment using ASAM Criteria and individualized planning
- Evidence-based therapies (CBT, DBT-informed skills, MI) integrated with holistic services
- MAT access for OUD and AUD, with ongoing medical oversight
- Trauma-informed and co-occurring capable care, including psychiatric services
- Family engagement with patient consent, and aftercare planning that includes scheduled follow-ups and telehealth options
- Ethical billing, outcomes monitoring, and coordination with community partners
For those balancing work or school, consider intensive outpatient and outpatient pathways, including outpatient alcohol rehab in New Jersey; for coverage questions, our team can confirm insurance coverage for drug rehab in NJ and outline expected costs before you start.
Veterans and families can explore specialized services like drug rehab for veterans in NJ, with careful coordination to community and VA resources.
If immediate help is needed outside business hours, call the SAMHSA National Helpline listed above, or 911 for emergencies.
Conclusion
Choosing a drug rehab in New Jersey means safe detox, right care levels, evidence-based therapy & steady aftercare. Confirm licensure, understand insurance, and plan for relapse risks. Next, verify benefits and book an assessment.
Frequently Asked Questions (FAQs)
What Levels of Care do Local Drug Rehab Centers Offer?
Drug rehab centers in New Jersey typically provide a full continuum of care so treatment matches a person’s needs over time. This often includes:
• Medical detox for safe withdrawal
• Inpatient or residential care (24/7 support)
• Partial Hospitalization Program (PHP), usually 20+ hours a week
• Intensive Outpatient Program (IOP), commonly 9–19 hours a week
• Standard outpatient, 1–8 hours a week
• Medication for opioid or alcohol use disorder when appropriate (such as buprenorphine, methadone via OTPs, or naltrexone)
• Individual, group, and family therapy
Most drug rehab centers in NJ align care with ASAM Criteria and step patients up or down based on progress & safety. Co-occurring mental health care is common, as is relapse prevention and aftercare planning.
How Can Families Check Quality and Safety at Local Drug Rehab Centers?
Quality at local rehab centers can be checked with a few key steps:
• Confirm an active New Jersey license from the state’s behavioral health authority
• Look for accreditation (The Joint Commission or CARF)
• Ask about medical oversight (physician leadership) and nursing coverage, especially 24/7 in detox
• Review detox & withdrawal protocols (use of CIWA for alcohol, COWS for opioids)
• Ensure evidence-based therapies are used (CBT, DBT, motivational interviewing)
• Check privacy practices (HIPAA), family involvement, and outcomes tracking
• Request clear financial policies
Red flags: guaranteed cures, vague pricing, no physician access, pressure to enroll immediately without assessment. If something feels off, pause & ask more questions.
What do Local Drug Rehab Centers Cost, and How Does Insurance Work?
Costs at centers in New Jersey vary by level of care, length of stay, and benefits. A simple way to plan:
1. Call your insurer and ask about substance use benefits, in-network options, prior authorization, deductibles, copays, and out-of-pocket maximums.
2. Ask the center to verify benefits and provide an itemized estimate (room/board if residential, labs, medications, therapy hours).
3. Check if NJ FamilyCare/Medicaid applies, or if your plan follows mental health parity rules.
4. Discuss time away from work, FMLA, or short-term disability may help.
5. Clarify transportation, pharmacy costs, and any fees that might appear later.
A good local program should explain coverage in plain language & help you estimate total cost before admission.
What Happens During Intake and Detox at Local Drug Rehab Centers?
Intake at a local rehab center starts with a clinical assessment: substance history, DSM-5 criteria, medical and mental health review, vitals, and sometimes labs. Withdrawal risk is scored with tools like CIWA (alcohol) or COWS (opioids).
Detox focuses on comfort and safety. Medications may include benzodiazepines for severe alcohol withdrawal, buprenorphine or methadone for opioid withdrawal (per regulations), plus hydration, sleep, nutrition, and symptom relief. Monitoring is frequent, often 24/7 in higher-acuity settings.
Once stable, the team maps the next step: inpatient/residential, PHP, or IOP, sets therapy goals, considers medication for relapse prevention, involves family when appropriate, and schedules aftercare. It’s not one-size-fits-all, but structured.
SAMHSA Treatment Locator: https://findtreatment.gov/
Principles of Drug Addiction Treatment: https://nida.nih.gov/sites/default/files/podat-3rdEd-508.pdf
NJ Department of Mental Health and Addiction Services: https://www.nj.gov/humanservices/dmhas/
Joint Commission Standards: https://www.jointcommission.org/en-us/standards
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts