An outpatient alcohol rehab center in New Jersey offers structured therapy and medical support while people keep living at home and working.
This overview explains who benefits, how care is delivered, and what to expect from assessment, treatment, and follow-up. It also outlines safety checks, medications, and ways to choose a licensed, evidence-based program.

Key Takeaways
- Outpatient alcohol rehab in New Jersey fits mild to moderate AUD when there’s safe housing & steady support; IOP is usually 9–15 hrs/week, standard outpatient about 1–5 hrs/week.
- Treatment uses proven therapies (CBT, motivational work, contingency management) and, when needed, meds like naltrexone, acamprosate, or disulfiram; privacy is protected by HIPAA & 42 CFR Part 2.
- Entry starts with a brief screening (e.g., AUDIT-C) and ASAM Criteria to match the right level of care; most insurance and NJ FamilyCare cover services due to parity, verify benefits, and know copays.
- Watch safety signs: risky withdrawal, unstable medical or mental health, or unsafe housing; in those cases, detox or residential first, then step down. Aftercare and relapse-prevention matter, a lot.
- Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey offering evidence-based addiction treatment plus holistic approaches; a team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
Outpatient Alcohol Rehab Center New Jersey
What “Outpatient” Means for Alcohol Use Disorder
Outpatient alcohol rehab in New Jersey offers structured treatment while a person lives at home. It generally includes two levels of care:
Both levels use evidence-based therapies, safety planning, and measured goals. The difference is intensity.
Standard Outpatient (OP)
- Usually 1–3 hours per week
- One individual session weekly or biweekly, plus groups as needed
- Best for mild Alcohol Use Disorder (AUD) or after completing IOP/residential
Intensive Outpatient Program (IOP)
- Typically 9–15 hours weekly, often 3–5 days a week, mornings or evenings
- Multiple groups plus weekly individual therapy, family contact, and case management
- A good fit for mild to moderate AUD with stable housing and adequate supports
A New Jersey program should match you to the lowest safe, effective level of care. This is based on ASAM Criteria, an accepted national framework used by NJ-licensed providers to determine the right intensity of services.
Who Benefits From Cutpatient Care?
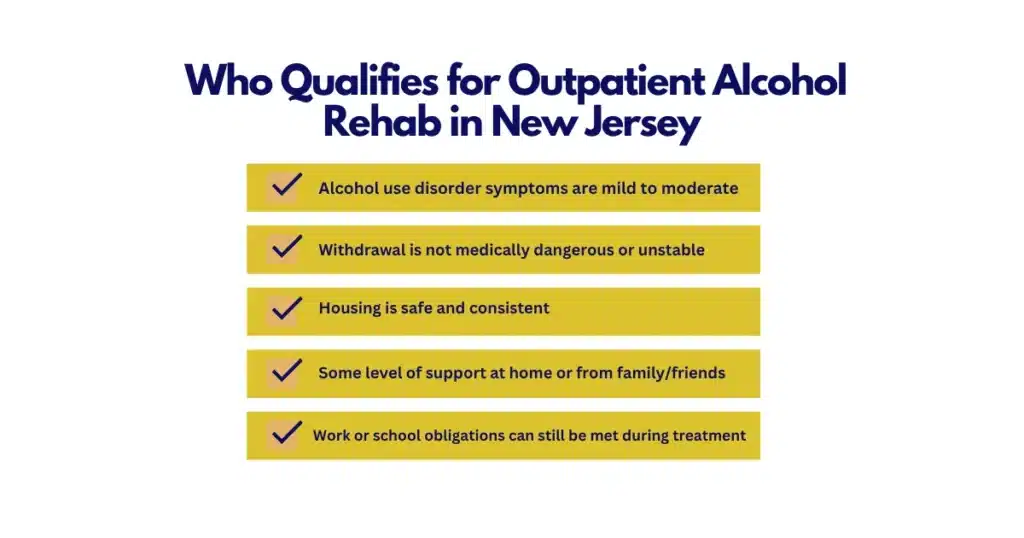
Outpatient care is appropriate when:
- Alcohol symptoms are mild to moderate
- Withdrawal is not medically dangerous or unstable
- Housing is safe and stable
- There are supportive family or friends, or at least consistent contact with sober supports
- Work or school responsibilities can be balanced with treatment
- There is motivation to reduce or stop alcohol use (even if it fluctuates, ambivalence is normal)
Patients with severe withdrawal risk, unsafe housing, or high medical/psychiatric risk usually need inpatient alcohol detox or residential treatment first. More on that below.

Evidence-Based Care Used in New Jersey Outpatient Programs
The goal is to reduce harm and improve stability. Core, research-supported approaches include:
- Cognitive Behavioral Therapy (CBT): build coping skills, challenge unhelpful thoughts, manage cravings
- Motivational Enhancement Therapy (MET): strengthen personal motivation and confidence for change
- Contingency management: small rewards for attendance, negative alcohol tests, or hitting goals
- Relapse prevention: identify triggers, practice skills, plan for high-risk moments
- Family-based interventions: psychoeducation, communication training, boundary-setting
- 12-step facilitation and mutual-support connections (optional, but helpful for many)
- Medication for Alcohol Use Disorder (MAT), when appropriate
Medications for AUD (MAT)
- Naltrexone (oral daily or monthly injectable): reduces reward from drinking and may cut cravings
- Acamprosate (oral, three times daily): supports early recovery by easing post-acute alcohol withdrawal symptoms
- Disulfiram (oral daily): causes unpleasant reaction if alcohol is consumed; best with supervision and structure
Medication decisions are individualized, considering medical history, liver function, goals, and risks. A program should coordinate with your primary care clinician and share lab results as needed.
Privacy and Your Information
New Jersey programs follow HIPAA and 42 CFR Part 2 confidentiality rules for substance use treatment. This means your treatment information is generally not shared without your written consent, except in very specific situations (e.g., medical emergencies, mandated reporting). Ask to see the Notice of Privacy Practices during intake.
A Quick Comparison of Outpatient Levels
| Feature | Standard Outpatient (OP) | Intensive Outpatient (IOP) |
|---|---|---|
| Time per week | ~1–3 hours | ~9–15 hours |
| Structure | Individual therapy and occasional groups | Several groups weekly, weekly individual, family sessions |
| Best for | Mild AUD, step-down from IOP | Mild to moderate AUD needing more structure |
| Common schedule | 1 evening a week | 3–5 days/week, mornings or evenings |
| Monitoring | Periodic testing as needed | Regular alcohol/drug testing and check-ins |
| Cost | Lower total weekly cost | Higher weekly cost but still outpatient |
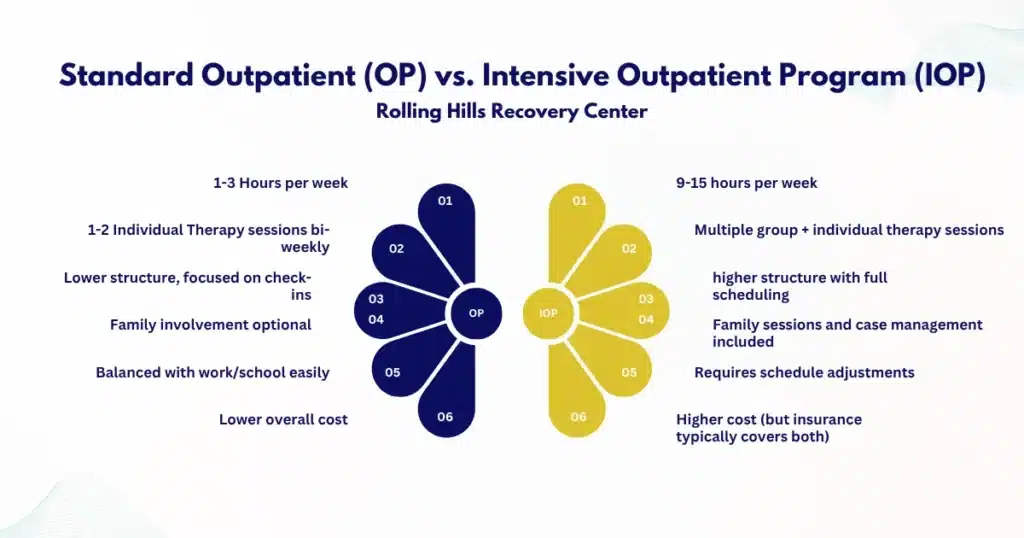
Rolling Hills Recovery Center offers evidence-based outpatient and IOP services in New Jersey with both clinical and holistic supports. Care can be stepped up or down to match progress and safety needs.
Admissions, Assessment, and Insurance in New Jersey
How Admission Typically Works
Most programs use a standardized, step-by-step intake:
- Screening
- A brief screen, such as AUDIT-C, to gauge risk from drinking
- Questions about current drinking patterns, withdrawal, and safety
- Comprehensive assessment
- ASAM multidimensional assessment to identify the right level of care
- Medical and psychiatric history, medications, supports, housing, employment or school needs
- Lab work as needed (e.g., liver function tests), with coordination to your PCP
- Benefits verification
- The provider confirms insurance coverage, co-pays, and any authorization needs
- If uninsured, discuss self-pay rates, payment plans, or assistance
- Intake appointment
- Paperwork, privacy forms, consent to release information (if you want)
- A first counseling session to set goals and start a safety plan
- Start treatment
- Orientation to groups and schedule
- Baseline testing, medication planning if indicated
If there are concerns for unsafe withdrawal or medical instability, staff will arrange a higher level of care before outpatient begins.
What Paperwork to Bring
- Photo ID
- Insurance card(s)
- Current medication list and doses
- Contact info for your primary care and any specialists
- Emergency contact and preferred pharmacy
- Any prior treatment records (if available)
- A work or school schedule (to match session times)
Insurance Coverage in NJ
- Most commercial plans and NJ FamilyCare (Medicaid) cover outpatient and IOP for substance use treatment when medically necessary
- New Jersey parity protections require health plans to cover mental health and substance use treatment comparably to medical/surgical care
- Prior authorization may be needed for IOP or MAT; your program should assist
Typical costs depend on plan specifics:
- Co-pays may range from $0 to $40–$60 per session for standard outpatient, sometimes higher
- Deductibles and coinsurance can apply, especially for IOP
- Self-pay rates vary widely by provider and services included
Always confirm your benefits in writing when possible.
A Simple Script to Confirm In-Network Coverage
- Call the member services number on your insurance card.
- Use this script:
“Hello, I’m calling to verify outpatient substance use treatment benefits in New Jersey. Is Rolling Hills Recovery Center in-network for outpatient and intensive outpatient services? If so, what are my benefits? Do I need prior authorization? What are my co-pay, coinsurance, and deductible? How many sessions are covered and over what period? Is medication management for alcohol use disorder covered? What is my out-of-pocket maximum for the year?”
Ask for the representative’s name, reference number for the call, and a benefits summary by email if available.

Timelines
- Many programs can complete screening the same day
- Assessment is often within 24–72 hours
- IOP start dates are usually available weekly; some offer rolling admissions
- MAT consultation can be scheduled quickly if indicated
If timing feels urgent, say so. Programs can often adjust.
What to Expect in Care
Weekly Time Commitment
- IOP: roughly 9–15 hours per week in groups and individual sessions
- OP: 1–3 hours per week
- Sessions are offered in the morning, afternoon, and early evening to accommodate work or school
- Hybrid models are common: some in-person groups, some telehealth
Core Services
- Individual therapy: goal-setting, CBT, and MET, skills practice
- Group therapy: relapse prevention, coping skills, peer support, psychoeducation
- Family sessions: communication, expectations, boundary setting
- Case management: housing, transportation, legal needs, medical follow-up
- Medication management: evaluation for naltrexone, acamprosate, or disulfiram
- Alcohol and drug testing: when appropriate to support safety and monitor progress
- Crisis and safety planning: steps to handle cravings, lapses, emergencies
Rolling Hills Recovery Center integrates holistic support, mindfulness, stress reduction, fitness, and nutrition to reduce relapse risk and improve overall well-being.
Co-Occurring Mental Health Support
Many people with AUD have anxiety, depression, trauma, or ADHD. Your plan should address both at once. Therapists and prescribers coordinate care to reduce symptoms that drive drinking. For more on overlapping ADHD symptoms and substance use, see the resource on ADHD and addiction.
Relapse-Prevention Planning
Expect a written plan that includes:
- Early warning signs and high-risk situations
- Triggers (internal, external)
- Skills to use (urge-surfing, delay-distraction-decide, reaching out)
- A list of sober activities and supports
- Crisis contacts and urgent care steps
Programs may recommend mutual-support meetings, recovery coaching, or alumni groups. Some people prefer secular supports; you should have options.
Testing and Accountability
- Breathalyzer or EtG/EtS urine testing can be used periodically
- Testing is not punitive; it guides clinical decisions and allows timely support
- Missing a test or a positive result leads to a care conversation, not shame
Telehealth and In-Person Blends
- Video visits for therapy and medication check-ins are common
- Some sessions require in-person attendance, especially certain groups or when labs are needed
- Telehealth must comply with privacy standards; choose a private space if possible
Safety Planning: A Quick Template
- My highest-risk times: evenings after work; weekends alone
- People I can contact: name, number
- Delay plan: wait 20 minutes, drink water, use coping skill, revisit choice
- Distraction ideas: quick walk, cold shower, breathing exercise, call a friend
- Remove or reduce exposure: no alcohol in the home; decline events with heavy drinking
- If danger rises: go to urgent care, call 988 for suicidal thoughts or severe distress, or 911 for medical emergencies
Coordinating with Primary Care
- Share medication lists and health concerns, especially liver health
- Discuss thiamine supplementation if heavy drinking or poor nutrition is present
- Align on labs and follow-up visits
- With written consent, your therapists and prescribers collaborate to keep care consistent
A Simple Weekly IOP Schedule Template
- Monday: 6–9 pm group
- Tuesday: 6–9 pm group
- Thursday: 6–9 pm group
- Individual therapy: Mon-Fri, 5 pm
- Medication check-in: every other Tuesday at 7 pm (telehealth)
Your schedule can flex around work or caregiving responsibilities.
“The outpatient level of care is a valuable community-based introduction to counseling. It affords the individual support, psychoeducation, and identification of coping skills. It is delivered with flexible scheduling, with both in-person and virtual options that are convenient for our busy lifestyles.”
Laura Riley, LCADC | Clinical Director at Rolling Hills Recovery Center
Choosing a New Jersey Outpatient Program
Licensure and Accreditation
- NJ DMHAS licensure: verify that the facility is licensed by the New Jersey Department of Human Services, Division of Mental Health and Addiction Services (DMHAS)
- Accreditation: The Joint Commission or CARF indicates extra quality oversight
A licensed, accredited program should use ASAM Criteria for level-of-care decisions and maintain strong privacy protections.
Staff Credentials
- Physicians (MD/DO), nurse practitioners, and registered nurses
- Licensed clinical social workers (LCSW), licensed professional counselors (LPC), licensed clinical alcohol and drug counselors (LCADC)
- Trauma-informed training; continuing education in SUD care
- Access to psychiatric consultation for co-occurring conditions
Cultural Responsiveness and Inclusion
- Services should reflect your identity and preferences, language, culture, faith, and sexual orientation or gender identity
- Ask about staff training on trauma, stigma reduction, and culturally responsive care
Medication Access
- Confirm availability of naltrexone (including extended-release injection), acamprosate, and disulfiram
- Ask about medication monitoring and liver function testing
- Clarify how medication integrates with therapy goals
Transportation and Scheduling
- Evening or weekend groups for working adults
- Telehealth options for bad weather or childcare gaps
- NJ FamilyCare members may have access to non-emergency medical transportation—ask your plan
- Proximity to NJ Transit can ease commute stress
Employer-Friendly Options
- Work-ready schedules and documentation if you are using FMLA or short-term disability
- Discreet communication that protects privacy
- Return-to-work planning and relapse prevention in the workplace
Aftercare and Alumni Support
- Step-down plans to OP after IOP
- Alumni groups or check-ins for accountability and community
- Coordination with community supports (mutual-help, recovery community centers)
- Mini “booster” sessions during high-risk periods (holidays, anniversaries)
Questions to Ask When Comparing Programs
- Are you NJ DMHAS-licensed and accredited (Joint Commission or CARF)?
- What therapies are used? How do you tailor care for AUD?
- Do you offer MAT for alcohol use disorder? On-site? Injectable naltrexone?
- How many hours per week is IOP? Evening options?
- How often do you drug/alcohol test, and how do you use the results?
- How do you coordinate with my primary care clinician or psychiatrist?
- What is the process if I need a higher level of care?
- What are my estimated out-of-pocket costs?
- What aftercare support do you provide?

Safety, Outcomes, and When to Step Up Care
Red Flags That Outpatient is Not Enough
If any of the following are present, consider a higher level of care first:
- Risk of severe alcohol withdrawal (history of delirium tremens, seizures, very high daily intake, unstable vitals)
- Inability to maintain abstinence long enough to participate safely in outpatient
- Active suicidal thoughts, untreated psychosis, or severe depression without stabilization
- Unstable medical conditions worsened by alcohol (e.g., GI bleeding, uncontrolled liver disease)
- Unsafe housing or domestic violence without immediate safety measures
- Active pregnancy with heavy use requiring close medical monitoring
Programs should use the ASAM Criteria to recommend medically monitored withdrawal management (detox) or residential treatment when needed. Once stabilized, patients can step down to IOP or OP.
How Transitions Work
- A warm handoff to detox or residential program
- Transfer of clinical information (with consent)
- Re-entry plan to outpatient after stabilization
- Medication continuation, e.g., resuming naltrexone after detox if appropriate
Harm Reduction Strategies
Not everyone is ready to stop immediately. Reducing risk still matters.
- Set a simple goal: drink less often, fewer drinks per occasion
- Plan alcohol-free days each week
- Eat before and during any drinking; hydrate often
- Avoid driving; use rideshares or a designated driver
- Store thiamine (vitamin B1) if heavy use and poor diet are concerns, discuss dosing with your clinician
- Remove hard liquor from the home; do not keep alcohol visible
- Practice urge-surfing and delay strategies; cravings pass
If there’s co-use of other substances, let your provider know. Safety planning will adjust.
Outcomes to Aim For
- Fewer heavy-drinking days
- Longer periods between drinking episodes
- Improved sleep, mood, and energy
- Repaired relationships and better work or school performance
- Lower medical risks and improved lab markers
Evidence shows that for people with mild to moderate AUD and stable supports, IOP can produce outcomes comparable to residential care. The key is matching intensity to need, using medications when indicated, and building a real-world relapse-prevention plan.
Tools and Templates You Can Use
- Insurance call sheet: note rep name, date/time, reference number, coverage summary
- Weekly schedule builder: pencil in groups first, then add recovery activities (walks, meetings, meals)
- Relapse prevention worksheet:
- Triggers: list 5
- Early warning signs: list 5
- Skills: 3–5 (breathing, calling a peer, delaying, journaling)
- Support list: 3–5 names and numbers
- If I slip: who I call, what I say, and how I re-enter care within 24 hours
- Medication tracker: doses, side effects, questions for prescriber
- Family communication plan: what to share, boundaries, emergency steps
When to Ask for More Help
- Cravings feel unmanageable despite the current plan
- Drinking increased after a stressor or loss
- Panic attacks, severe anxiety, or depression are rising
- A medical clinician noted concerning labs or new symptoms
- You’re worried your life is becoming unmanageable. This self-check can help: Are drugs and alcohol making life unmanageable?
Getting more structure early prevents bigger setbacks later.
How Rolling Hills Recovery Center Approaches Outpatient Alcohol Treatment
- Evidence-based treatments: CBT, MET, relapse prevention, contingency management
- Holistic supports: mindfulness, stress management, movement, and nutrition basics
- MAT for AUD when indicated: naltrexone (including extended-release), acamprosate, disulfiram
- Trauma-informed, culturally responsive care; inclusive programming for diverse patients
- Flexible scheduling with in-person and telehealth options
- Coordination with your PCP and specialists
- Alumni and step-down options to maintain gains
Care plans are personalized and adjusted over time. The focus remains on safety, measurable progress, and meaningful life changes.
Simple How-To Steps to Get Started in New Jersey
- Make the call
- Ask for an alcohol use evaluation and mention any urgent safety concerns (withdrawal, suicidality).
- Complete the screen
- Be honest about how much and how often you drink; this ensures the right level of care.
- Verify benefits
- Use the script above; get a written summary if possible.
- Prepare for intake
- Bring ID, insurance, medication list, and any labs or records.
- Plan transportation and a private space for telehealth if needed.
- Start with a first week plan
- Note your group days and times.
- Remove alcohol from the home.
- Identify two people you can call if cravings hit.
- Review safety
- Write a 5-step safety plan before your first group session.
- Program staff will help fine-tune it.
- Reassess after two weeks
- Discuss what’s working and what’s not.
- Consider MAT if cravings remain high.
New Jersey-Specific Quality Checks
- Confirm the program appears under NJ DMHAS-licensed providers
- Ask how ASAM Criteria are used to set and adjust your level of care
- Request information on outcome tracking (e.g., reductions in heavy-drinking days, retention rates)
- Ensure privacy practices are clear and in writing
- If needed, ask about connections to higher levels of care (detox/residential), including rapid transfers
Practical FAQs
How Long Does IOP Last?
- Commonly 6–12 weeks, but length should be individualized. Some complete sooner; others need more time or step down to OP.
Can I Keep Working?
- Yes, many patients attend evening IOP. Ask about employer documentation and privacy.
Will I Be Forced to Stop Drinking Immediately?
- The recommendation may be to stop for safety. But treatment meets you where you are. If you choose harm reduction, the plan will still aim to reduce risk and improve health.
What If I Slip?
- Tell your therapist right away. Slips are data. The plan will be adjusted, sometimes adding sessions, skills, or medication support.
Do I Have to Attend 12-Step Meetings?
- Not required. If you want them, the staff can help you connect. Secular alternatives are available.
Reliable Education Resources
- NIAAA: treatment science and medications for AUD – https://www.niaaa.nih.gov
- ASAM Criteria (level-of-care framework) – https://www.asam.org/asam-criteria
- NJ Department of Human Services – DMHAS (state standards and licensure) – https://www.nj.gov/humanservices/dmhas/
- CDC Alcohol and Public Health (risks and health impact) – https://www.cdc.gov/alcohol
Conclusion
Outpatient alcohol treatment in New Jersey works best when care matches need, therapy & medication, family support, and relapse planning. Choose evidence-based care; ask about MAT, schedules, insurance; watch red flags. Next steps: verify benefits and schedule an assessment.
The expertise at Rolling Hills Recovery Center, a drug and alcohol rehab and addiction treatment center in New Jersey, offers evidence-based treatment and holistic approaches; our team helps individuals overcome substance abuse and achieve lasting results, and can help readers.
Frequently Asked Questions (FAQs)
What is Outpatient Alcohol Rehab in New Jersey, and Who is it Best For?
Outpatient alcohol rehab in New Jersey is structured treatment delivered while a person lives at home. It suits individuals with mild to moderate alcohol use disorder who have stable housing, reliable transportation, and no signs of dangerous withdrawal.
Medical teams typically use standard screens (e.g., AUDIT-C) and the ASAM Criteria to match care safely. If there’s severe withdrawal risk, unsafe housing, or acute medical/psychiatric needs, detox or residential may be safer first, then step down to outpatient alcohol rehab in New Jersey.
What Happens Day to Day in Outpatient Alcohol Rehab in New Jersey?
Most programs offer individual therapy, group therapy, family sessions, relapse-prevention skills, and medication options when appropriate. Intensive outpatient (IOP) is usually 9–15 hours per week; standard outpatient may be 1–5 hours.
Expect cognitive behavioral strategies, motivational work, and support for sleep, nutrition, and stress. Toxicology testing is used when clinically helpful. Care coordination with primary care & psychiatry is common.
Many clinics blend in-person and telehealth to keep outpatient alcohol rehab in New Jersey flexible and accessible.
How Long Does Outpatient Alcohol Rehab in New Jersey Take, and Can Someone Keep Working?
Length varies by need. IOP often runs 6–12 weeks, followed by step-down to fewer hours, then aftercare. Many people continue working or attending school because sessions can be scheduled in the evenings or early mornings.
Privacy protections (HIPAA and 42 CFR Part 2) safeguard treatment information. If work stress or shift hours interfere, clinicians adjust the plan so outpatient alcohol rehab in New Jersey remains doable, not overwhelming.
What Does Outpatient Alcohol Rehab in New Jersey Cost, and Will Insurance Help?
Costs depend on session frequency, testing, and medications. Most commercial plans and New Jersey Medicaid (NJ FamilyCare) have mental health and substance use coverage due to parity laws.
Out-of-pocket costs may include copays, coinsurance, and deductibles. Programs usually verify benefits up front and explain any fees in plain language.
If finances are tight, ask about payment plans; keeping outpatient alcohol rehab in New Jersey affordable improves follow-through and outcomes.
What Sets Rolling Hills Apart for Outpatient Alcohol Rehab in New Jersey?
Rolling Hills Recovery Center delivers evidence-based care with medical oversight and a whole-person approach, therapy, medications, family support, and coordinated aftercare.
Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches.
Our team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
This clinical focus, plus practical scheduling and ongoing relapse-prevention, helps outpatient alcohol rehab in New Jersey feel structured yet humane.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












