Women face unique medical, emotional, & safety needs in recovery. Women’s drug rehab in NJ centers focus on trauma, mental health, and family roles, with options from detox to outpatient.
Evidence-based therapy, medication when appropriate, and compassionate support, along with childcare, transportation, and postpartum care, can improve outcomes and confidence while protecting privacy and dignity at every step.
Key Takeaways
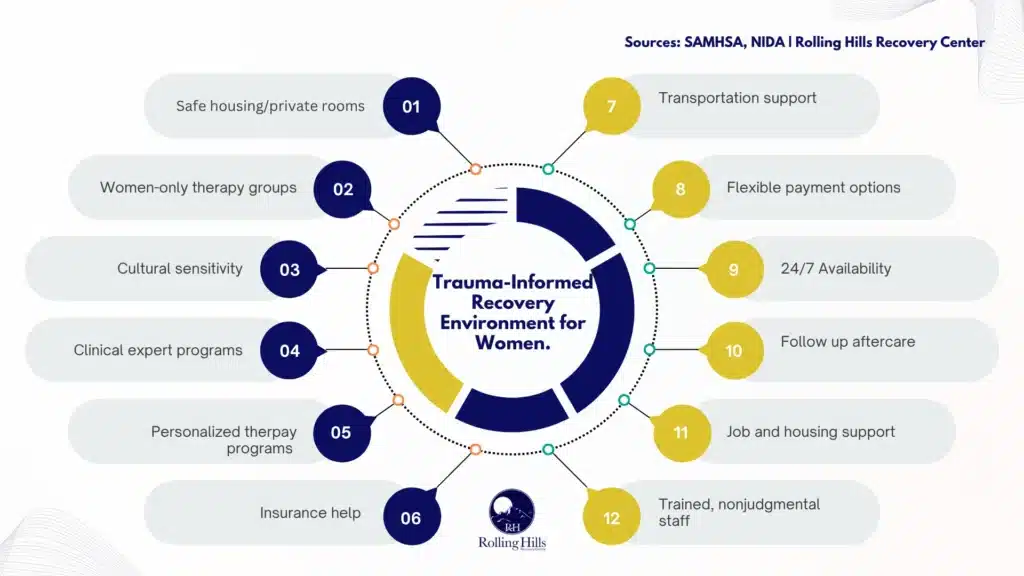
- Women’s programs work best when they are trauma‑informed, prioritize safety and privacy, and use women‑only groups when helpful.
- Treat the whole person: substance use and mental health together, plus pregnancy or postpartum care; use MAT like buprenorphine, methadone, or naltrexone when appropriate with OB/GYN coordination.
- Care can step up or down: medical detox, residential, PHP or IOP, then outpatient; start relapse prevention and naloxone planning early.
- Real‑life help matters, insurance and NJ Medicaid benefits, FMLA support, childcare & transportation, confidentiality; inclusive care for LGBTQ+ people and those facing IPV.
What Women’s Drug Rehab Means in New Jersey
Gender-Responsive, Trauma‑Informed Environments
Women’s drug rehab in New Jersey refers to treatment settings designed around the realities many women face: caregiving roles, trauma exposure, intimate partner violence risk, and unequal access to resources.
Programs that are gender‑responsive and trauma‑informed prioritize:
- Safety first: predictable routines, private spaces, secure visitor policies, and zero tolerance for harassment.
- Emotional safety: staff trained in trauma‑informed care; choice and consent embedded in every step; no shaming.
- Peer connection: women’s groups, parenting groups, and mentorship that normalize help‑seeking.
- Culturally sensitive care: respect for race/ethnicity, language, faith, and immigration concerns; interpreters when needed.
- Practical supports: childcare options, flexible scheduling, and coordination with social services.
These elements improve engagement because many women enter treatment with chronic stress, limited time, and a high fear of judgment. Care must be compassionate and practical.
Co‑Occurring Mental Health Needs are Common
Depression, anxiety, and PTSD frequently overlap with substance use in women. Effective programs screen for:
- Mood and anxiety disorders
- PTSD and complex trauma
- Eating disorders
- Bipolar spectrum disorders
- ADHD and learning differences
- Suicidality and self‑harm risk
Validated tools (PHQ‑9, GAD‑7, PCL‑5, Columbia Suicide Severity Rating Scale) help identify needs early. Treatment plans should integrate therapy, medication management when appropriate, and skills training (e.g., grounding, distress tolerance) to reduce relapse risk.
Pregnancy and Postpartum Require Special Protocols

Substance use during pregnancy and postpartum carries both medical and social risks. Clinicians follow established guidance for prenatal screening, medication treatment, and coordination with OB/GYN. Key priorities:
- Immediate, nonjudgmental screening for pregnancy in detox and admission.
- Medication for opioid use disorder (MOUD) with methadone or buprenorphine during pregnancy per the American College of Obstetricians and Gynecologists (ACOG).
- Neonatal Abstinence Syndrome (NAS) education and hospital coordination.
- Breastfeeding guidance: often encouraged for women on stable methadone or buprenorphine with no ongoing illicit use and no contraindications.
- Postpartum relapse prevention: rapid follow‑up visits, sleep and nutrition support, partner counseling, safe‑storage plans for medications, and mental health screening (postpartum depression/anxiety).
ACOG’s recommendations on pregnancy and opioid use disorder are a standard reference. See ACOG’s “Opioid Use and Opioid Use Disorder in Pregnancy.”
Why Gender‑Specific Programming Matters
Evidence from the National Institute on Drug Abuse (NIDA) and the Substance Abuse and Mental Health Services Administration (SAMHSA) indicates that gender‑specific, trauma‑informed programming improves engagement, retention, and satisfaction with care.
Women are more likely than men to have histories of trauma and caregiving strain; treatment that addresses these factors keeps women in care longer, which correlates with better outcomes. NIDA’s pages on Substance Use in Women and SAMHSA’s Women and Substance Use resources provide additional details.
Rolling Hills Recovery Center applies these principles by combining evidence‑based treatments with holistic supports in a calm, private environment. The emphasis is on practical progress and sustained recovery… not perfection.
Levels of Care and Core Treatments
Finding the Right Level of Care
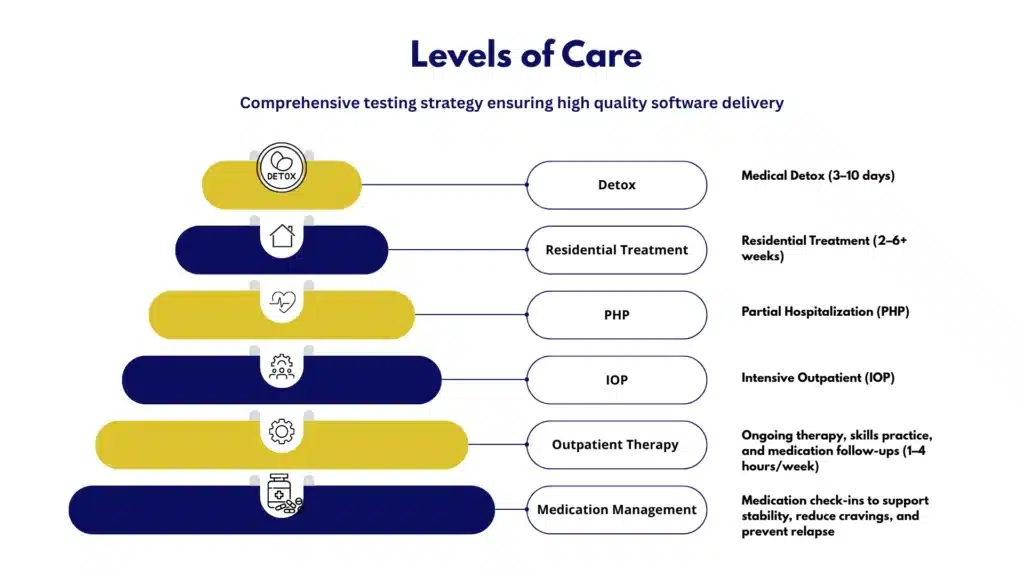
Treatment is matched to severity, stability, and life demands. A typical pathway:
- Medical detox (3–10 days): For withdrawal from alcohol, benzodiazepines, or opioids under close supervision; stabilization of vitals, hydration, and sleep.
- Residential treatment (2–6 weeks or longer): 24/7 structured setting; intensive therapy; ideal when home triggers are strong or safety is a concern.
- Partial Hospitalization Program PHP (4–6 hours/day, 5 days/week): Step‑down from residential or a high‑support entry point; daily group and individual therapy with medical oversight.
- Intensive Outpatient Program IOP (9–12 hours/week): Therapy while maintaining work, school, or caregiving; strong relapse‑prevention focus.
- Outpatient and medication management (1–4 hours/week): Ongoing therapy, skills practice, and medication follow‑ups.
A stepped‑care approach allows movement up or down as symptoms, safety, and stability change.
FDA‑Approved Medications for OUD and AUD, Including Pregnancy Considerations
Medication supports brain stabilization and reduces relapse risk. For many women, especially those with trauma histories, medications help make therapy possible by quieting cravings and withdrawal.
- Opioid Use Disorder (OUD): methadone, buprenorphine, extended‑release naltrexone (XR‑NTX).
- Alcohol Use Disorder (AUD): naltrexone (oral or XR), acamprosate, disulfiram (select cases).
Below is a quick comparison:
| Medication | Indication | How it helps | Pregnancy/Postpartum notes |
|---|---|---|---|
| Methadone | OUD | Full opioid agonist; prevents withdrawal and cravings | Recommended in pregnancy (ACOG); coordinate dose adjustments; breastfeeding often supported if stable and no illicit use |
| Buprenorphine | OUD | Partial agonist; lowers overdose risk vs full agonists | Deterrent by causing an aversive reaction if alcohol consumed |
| XR‑Naltrexone | OUD/AUD | Opioid antagonist; blocks effects; also reduces alcohol cravings | Typically not initiated during pregnancy for OUD; may be considered postpartum in select cases; discuss risks/benefits |
| Naltrexone (oral) | AUD | Reduces heavy drinking days | Avoid in pregnancy unless benefits outweigh risks; discuss contraception plans |
| Acamprosate | AUD | Supports abstinence, normalizes glutamate | Recommended in pregnancy (ACOG); monoproduct commonly used in pregnancy; breastfeeding may be encouraged if criteria are met |
| Disulfiram | AUD | Deterrent by causing an aversive reaction if alcohol is consumed | Not used in pregnancy; requires high motivation and monitoring |
Overdose reversal: naloxone is lifesaving in opioid overdose and should be carried by patients and family. In pregnancy, naloxone is still recommended in suspected overdose; maternal survival is the priority.
For women focusing on opioid recovery, see Rolling Hills Recovery Center’s program information for rehab for opioid addiction in NJ.
Evidence‑Based Psychotherapies That Work

Trauma‑informed, skills‑based treatments build resilience:
- Cognitive Behavioral Therapy (CBT): thought‑behavior links; relapse prevention; coping skills.
- Dialectical Behavior Therapy (DBT): emotion regulation, distress tolerance, and interpersonal effectiveness; helpful for self‑harm risk and volatility.
- Eye Movement Desensitization and Reprocessing (EMDR): trauma processing; reduces PTSD symptoms that often drive substance use.
- Contingency Management (CM): incentives for meeting targets (e.g., negative drug screens); strong evidence for stimulant use disorders.
- Motivational Interviewing (MI): aligns treatment goals with personal values; increases readiness for change.
- Family therapy: boundary setting, co‑parenting plans, and education to reduce stigma and improve support.
- Psychiatric care: when indicated, medication for depression, anxiety, or bipolar spectrum disorders.
Whole‑Person Care: Family, Nutrition, Sleep, and Recovery Capital
Wellness basics are not “extras.” Programs should provide:
- Nutrition counseling to stabilize energy and mood; address anemia or deficiencies common in postpartum and chronic stress.
- Sleep restoration plans (sleep hygiene, behavioral strategies, and, when needed, cautious medication).
- Pain management without escalation of addictive medications (PT, non‑opioid options, mindfulness, graded activity).
- Parenting and caregiving supports; referrals to WIC, Early Head Start, or family services when helpful.
- Case management to rebuild recovery capital: identification documents, benefits, education, and legal navigation.
Overdose Education and Naloxone
Overdose risk spikes during transitions (post-detox, postpartum, after incarceration, or after short abstinence). Best practice includes:
- Training on overdose recognition and response.
- Naloxone distribution to patients and family.
- Safer‑use education for those not yet abstinent.
- Linkage to syringe services and infectious disease screening, where appropriate.
- Safety planning for high‑risk days (anniversaries, custody hearings, sudden stress).
The CDC’s overdose prevention resources and New Jersey DMHAS updates are good references.
Access, Logistics, and Support in New Jersey
Insurance and Medicaid Basics
In New Jersey, commercial insurance and NJ FamilyCare (Medicaid) cover substance use treatment benefits under parity law. Practical steps:
- Contact the number on the insurance card. Ask for SUD benefits, in‑network facilities, deductible, and prior authorization rules.
- Request benefits verification from a treatment provider.
- If uninsured, apply for NJ FamilyCare; ask about presumptive eligibility.
- Keep copies of approvals and authorization numbers.
Rolling Hills Recovery Center can verify benefits quickly. To review options, visit the page on insurance coverage for drug rehab in NJ.
Helpful resources:
- SAMHSA treatment and funding information
- NJ Department of Human Services – Division of Mental Health and Addiction Services (DMHAS)
FMLA and Job Protection
The Family and Medical Leave Act (FMLA) may protect up to 12 weeks of unpaid, job‑protected leave for serious health conditions, including treatment for substance use disorders, when care is delivered by a healthcare provider. These are the basics you should know:
- Employer size: 50+ employees within 75 miles.
- Employee eligibility: at least 12 months employed and 1,250 hours worked in the past year.
- Confidential: only necessary information is shared with HR; diagnosis details are typically not required.
Request documentation from the treating clinician; be proactive if you need step‑down scheduling over several weeks.
Childcare and Family Logistics
Common solutions include:
- Daytime PHP/IOP tracks while children are in school.
- On-site or partner childcare (when available).
- Telehealth therapy sessions during nap times or after bedtime.
- Family calendars and backup caregiver plans; written consent for designated caregivers to pick up children.
- Parenting support groups and co‑parenting agreements to reduce conflict and triggers.
Transportation and Location
Transportation is often the barrier. Options:
- Medicaid non‑emergency medical transportation (NEMT) for eligible NJ FamilyCare members, schedule rides ahead of time.
- NJ TRANSIT routes and reduced fare programs.
- Mileage reimbursement or ridesharing support through community partners.
- Strategic scheduling (cluster appointments to reduce trips).
Privacy and Confidentiality Protections
Patients have strong privacy protections:
- HIPAA safeguards personal health information.
- 42 CFR Part 2 adds extra confidentiality for SUD treatment records.
- Releases of information (ROI) are patient‑controlled and time‑limited.
- Safe contact preferences: Specify voicemail/text instructions and who may receive information.
Coordinating with OB/GYN and Primary Care
For pregnant or postpartum patients, or those with chronic conditions:
- Share medication lists and safety plans with OB/GYN and primary care (with consent).
- Align prenatal and pediatric appointments with treatment schedules.
- Plan hospital coordination for delivery, NAS care, and breastfeeding counseling.
- Update all prescribers to prevent unsafe drug interactions.
Community Resources and Peer Recovery
Connection reduces relapse. Useful supports:
- Mutual‑help options: Women for Sobriety, SMART Recovery, AA/NA women’s meetings, and faith‑based groups if desired.
- Peer recovery specialists for coaching and system navigation.
- Domestic violence resources and legal aid when safety is a concern.
- NIDA and SAMHSA websites for education and treatment locators.
- NJ DMHAS for state resources and programs.
Housing and Employment (Social Determinants)
Address real‑world stressors:
- Housing: sober living, transitional housing, or rapid rehousing through local Continuums of Care.
- Employment: resume refresh, interview preparation, and record‑expungement assistance; protected recovery time during early care.
- Food security and utilities: NJ 211, WIC, SNAP.
- Financial planning: payment plans, medication assistance programs, and budgeting guidance.
How to Choose Women’s Drug Rehab in NJ
Licensure and Accreditation
Confirm that the program holds:
- State licensure through New Jersey (DMHAS oversight).
- National accreditation (e.g., The Joint Commission or CARF).
- Clear patient rights and grievance policies are posted and easy to understand.
Ask for documentation; reputable programs share this openly.
Staff Credentials and Stability
Look for a multidisciplinary team with:
- Board‑certified addiction medicine physicians or psychiatrists.
- Licensed clinical social workers, professional counselors, and psychologists trained in trauma care (EMDR/DBT).
- Nursing coverage with detox experience.
- Case managers and peer specialists with women’s services expertise.
Low turnover and ongoing staff training are signs of quality.
Assessment Quality and Individualized Care
Effective programs use standardized, validated tools for intake and ongoing assessment. Minimum expectations:
- Full biopsychosocial assessment within 24–72 hours of admission.
- Screening for IPV, depression, anxiety, PTSD, suicidality, and eating disorders.
- ASAM multidimensional assessment to match the level of care.
- Written, individualized care plan updated weekly or bi‑weekly.
- Measurable goals: attendance, cravings scale, urine drug testing frequency, symptom reduction targets.
Medication Policies and Inclusive Care
Medication practices should be safe, science‑based, and stigma‑free:
- On-site or closely coordinated MOUD and AUD medications.
- Pregnancy‑informed protocols per ACOG; lactation and postpartum guidance included.
- Naloxone distribution and training for patient and family.
- Non‑punitive responses to lapses; quick re‑stabilization pathways.
- Inclusion and safety for LGBTQ+ patients; staff training on gender identity and sexual orientation; and affirming groups available.
For alcohol‑focused outpatient options that fit work and family schedules, see Rolling Hills Recovery Center’s outpatient alcohol rehab in NJ.
Outcomes Tracking and Relapse‑Prevention Planning
Quality programs measure what matters:
- Retention/engagement rates by level of care.
- Functioning measures (work/school attendance, family stability).
- Post‑discharge follow‑ups at 30/90/180 days.
- Patient‑reported outcomes (cravings, quality of life).
- Written relapse‑prevention plan before discharge, with next‑day follow‑up scheduled.
A Quick Selection Checklist
Use this step‑by‑step list when calling programs:
- Ask about licensure/accreditation and staff credentials.
- Confirm women‑specific groups and trauma‑informed policies.
- Verify MAT availability and pregnancy/postpartum protocols.
- Request a sample weekly schedule (PHP, IOP, or residential).
- Ask about IPV screening, safety planning, and confidentiality.
- Confirm family therapy and parenting supports.
- Review discharge planning, aftercare, and 24/7 crisis coverage.
- Clarify insurance, out‑of‑pocket costs, and prior authorization.
- Discuss transportation and childcare solutions.
- Ask how they measure outcomes and share results.
Aftercare and Relapse Prevention
Step‑Downs That Sustain Progress
Continuity of care matters. Evidence shows better outcomes when patients move through structured step‑downs:
- Residential → PHP → IOP → Outpatient → Alumni/peer support
- Medication continuity throughout, with dose adjustments as stress changes
- Frequent check‑ins during the first 90 days post‑discharge
Establish these transitions before leaving a higher level of care.
Trauma‑Informed Safety Planning
Safety planning is essential, especially for women with IPV risk or stalking concerns. Include:
- A code word with friends/family to signal help.
- Shelters, legal aid, and emergency contacts are listed and saved.
- Copies of key documents stored safely (and digitally).
- Phone settings: blocked contacts, privacy controls, and location services reviewed.
- Plan for safe medication storage and home boundaries.
Parenting Supports That Fit Real Life
Recovery and parenting can support each other when planned:
- Feed/sleep routines that reduce stress and improve regulation.
- Emergency caregiver plans and written consent forms.
- Pediatrician coordination for infant NAS follow‑up, nutrition, and immunizations.
- Parenting groups addressing guilt and shame; skills for calm discipline and attachment.
Mutual‑Help, Peer Mentors, and Community

Encourage connection with:
- Women‑only or trauma‑informed meetings (AA/NA/SMART, Women for Sobriety).
- Online communities and tele‑meetings for nights/weekends.
- Peer recovery coaches for accountability and resource navigation.
- Alumni groups and volunteer roles to build purpose.
Telehealth and Digital Tools
Leverage tech to maintain momentum:
- Tele‑IOP or tele‑therapy for busy weeks or childcare gaps.
- Asynchronous check‑ins (secure messaging) for early warnings.
- Craving trackers and mood apps; scheduled prompts for medication and sleep.
- Calendar reminders for therapy, labs, and RX refills.
Naloxone Readiness and Overdose Prevention
Relapse can happen; overdose should not be fatal:
- Keep naloxone in home, purse/diaper bag, and car; teach family how to use it.
- Review overdose signs: slowed breathing, pinpoint pupils, blue lips, unresponsiveness.
- Call 911 first, then give naloxone, rescue breathe if trained; stay with the person.
- Avoid using alone; if a lapse occurs, reduce the amount, and tolerance drops quickly after abstinence.
The CDC’s overdose prevention resources and New Jersey’s DMHAS updates can help you stay current on community naloxone access and training.
Coping Skills for Triggers and Stress
Skills need practice. Simple daily routine:
- Morning: brief grounding (5‑4‑3‑2‑1 sensory check), medication, hydration, breakfast.
- Midday: movement break, snack, short breathing exercise.
- Evening: reflect on triggers; text a peer or attend a meeting; prepare for sleep.
- Weekly: therapy, skills group, and a planned reward (self‑care is not optional).
Core tools:
- Urge surfing: notice cravings like waves; they pass.
- Opposite action (DBT): choose the action that supports long‑term goals.
- Thought records (CBT): challenge “always/never” thinking.
- Trauma‑safe grounding: cold water splash, describe five objects in the room, focus on feet on the floor.
A Simple Relapse‑Prevention Plan Template
Copy, print, or save the following and review weekly:
- My top three reasons to stay sober: [fill in]
- Early warning signs I’m slipping: [list 5]
- People I will call/text within 15 minutes if I have cravings: [names/numbers]
- Safe places I can go within 30 minutes: [locations]
- Skills I will use when triggered (pick 3): [e.g., 4‑7‑8 breathing, opposite action, walk outside]
- My medication plan and refill dates: [medication, dose, pharmacy, refill date]
- Meeting schedule this week: [days/times]
- High‑risk situations to avoid right now: [list]
- If I do lapse: I will call [name], schedule an urgent session, use naloxone if needed, and return to a higher level of care if safety is at risk.
- Backup plan: If I cannot reach my supports, I will go to [clinic/ER] or call 988/911 for immediate help.
Step‑by‑Step: Your First 14 days After Discharge
- Day 1: Attend scheduled appointment (therapy or medication). Confirm next three appointments.
- Day 2: Fill all prescriptions; set alarms for dosing; check naloxone supply.
- Day 3: Join one women’s meeting; ask for a temporary sponsor or peer mentor.
- Day 4: Finalize weekly calendar with childcare, work, and recovery blocks.
- Day 5: Create a food plan and sleep routine for the next 7 days.
- Day 6: Review relapse‑prevention plan; share with one trusted person.
- Day 7: Rest day with low‑stress activities; short nature walk.
- Day 8–10: Add one coping skill daily; practice it twice.
- Day 11: Confirm transportation for next week; pre‑book rides if needed.
- Day 12: Clean and organize one area at home to reduce triggers.
- Day 13: Family check‑in; discuss boundaries and support needs.
- Day 14: Reflect on wins; adjust plan; identify one small reward.
Practical Tools and Templates You Can Use Today
- Questions to ask before admission (printable):
- What levels of care are available for women?
- How do you screen for trauma, depression, anxiety, and IPV?
- Which medications do you offer for OUD and AUD? Pregnancy protocols?
- Do you provide EMDR or DBT?
- Can you coordinate with my OB/GYN or pediatrician?
- What childcare or scheduling flexibility is available?
- How do you measure outcomes and share updates with me?
- What is the aftercare plan and alumni support?
- Medication and appointment tracker (weekly):
- Medications/doses and times
- Refill dates, pharmacy info
- Therapy/group schedule
- Transport booked? yes/no
- Naloxone location and expiration date
- Safety wallet card:
- Three emergency contacts
- Primary clinic number
- 988 Suicide & Crisis Lifeline
- Local urgent care/ER
- Insurance call script:
- “I’m calling to confirm substance use treatment benefits. Can you tell me: deductible and out‑of‑pocket max; in‑network facilities; pre‑authorization requirements for detox, residential, PHP, and IOP; covered medications for addiction treatment; and any limits on visit numbers?”
Rolling Hills Recovery Center’s Approach in New Jersey
- Evidence‑based and holistic: Integrated CBT/DBT, MOUD and AUD medications, family therapy, and relapse‑prevention planning.
- Women‑centered supports: trauma‑informed groups, parenting resources, coordination with OB/GYN, and discreet scheduling to protect privacy.
- Flexible access: step‑downs from residential to PHP/IOP and outpatient, with telehealth options where appropriate.
- Insurance navigation: benefits verification, pre‑auth support, and transparent cost discussions; see insurance coverage for drug rehab in NJ.
- Alcohol‑focused outpatient options: flexible daytime/evening care through our alcohol rehab in NJ.
References and Further Reading
- National Institute on Drug Abuse (NIDA): Substance Use in Women
- American College of Obstetricians and Gynecologists (ACOG): Opioid Use and Opioid Use Disorder in Pregnancy
- Centers for Disease Control and Prevention (CDC): Overdose Prevention
These sources provide current, non‑commercial information and are useful when comparing programs or planning next steps.
Conclusion
Women do best with care that is safe, trauma-informed & practical. Most helpful: integrated mental health, appropriate MAT, and strong aftercare.
Rolling Hills Recovery Center is here to help. Our team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
Next steps: reach out, verify insurance benefits, and schedule an assessment.
Frequently Asked Questions (FAQs)
What is Women’s Drug Rehab and How is it Different from Mixed‑Gender Care?
Women’s drug rehab uses gender‑responsive, trauma‑informed treatment that accounts for higher rates of anxiety, depression, PTSD, intimate partner violence, pregnancy, and postpartum needs.
Safer spaces, women‑only groups, and childcare planning are common. Clinically, these features improve engagement and retention, which supports better outcomes.
What Treatments are Used in Women’s Drug Rehab, Including During Pregnancy or Postpartum?
Women’s drug rehab commonly includes CBT & DBT, trauma therapies like EMDR, contingency management, and family work.
For opioid use disorder, methadone or buprenorphine can be used during pregnancy; alcohol use disorder may involve naltrexone or acamprosate when appropriate.
Care is coordinated with OB/GYN and primary care, plus lactation planning if needed.
How Long Does Women’s Drug Rehab Take in New Jersey, and What Levels of Care are Available?
Detox is usually days; residential is often 2–6 weeks; partial hospitalization or IOP can run several weeks to a few months. Not one‑size‑fits‑all. The plan depends on medical needs, safety, home support, and progress.
Insurance, including many NJ plans and some Medicaid options, may help cover parts of women’s drug rehab.
How Should Someone Prepare for Women’s Drug Rehab in New Jersey?
Bring ID, insurance info, current medication lists, and contact numbers. Arrange childcare and transportation when possible; programs can problem‑solve these barriers.
Expect screening for trauma, mood, and substance use. Safe storage of medications, privacy rules, and planning for aftercare are part of women’s drug rehab from day one.
How Does Rolling Hills Recovery Center Support Women’s Drug Rehab in New Jersey?
Rolling Hills Recovery Center's drug rehab services emphasize trauma‑informed therapy, evidence‑based care, coordination with medical providers, and practical supports like relapse‑prevention skills and family involvement.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












