Suboxone can steady withdrawal, quiet cravings, and help you feel like yourself again. Here, we explain how it works, when to start, and what a safe induction looks like, based on what we do every week at Rolling Hills Recovery Center. You will see clear steps, realistic timelines, and what support to expect along the way.

Key Takeaways
- Suboxone eases withdrawal and cravings; most feel relief in 30 to 60 minutes; start in clear moderate withdrawal (COWS 8 to 12).
- Timing matters: 12 to 24 hours after short-acting opioids; 24 to 48 hours after long-acting or methadone; with fentanyl, consider micro-induction to avoid precipitated withdrawal; go slow, reassess.
- Safety first: common effects include nausea, headache, constipation; avoid alcohol and benzodiazepines when possible; keep naloxone at home, and book regular follow-ups every 30 to 90 days.
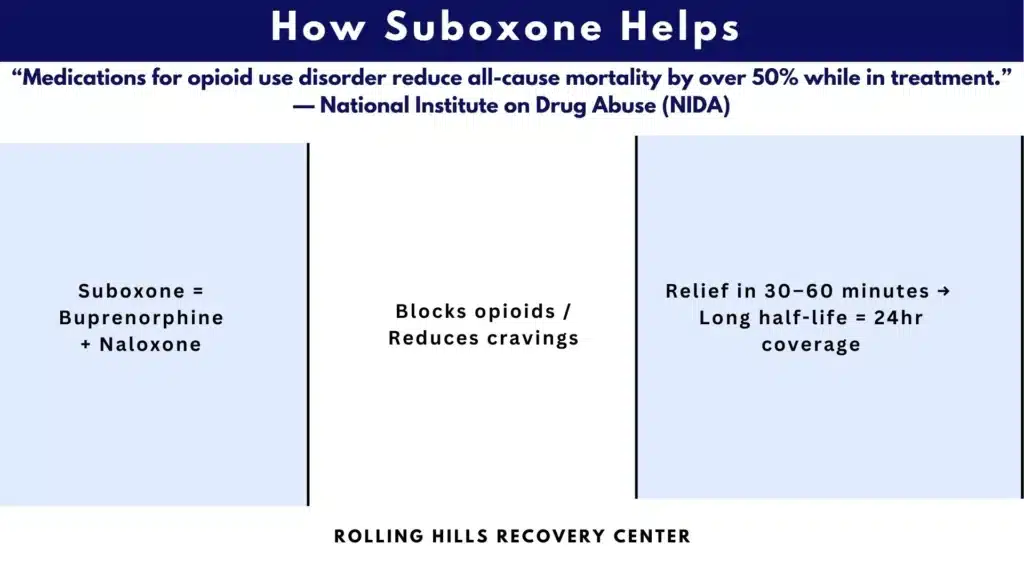
- Outcomes are better with medication plus support; medications for opioid use disorder cut overdose deaths by about half while in care; maintenance works better than quick tapers. Simple plan, safer start.
What Suboxone is and How it Helps Withdrawal
Buprenorphine Naloxone in Brief
Suboxone is the brand name for a combination of buprenorphine and naloxone, taken most often as a sublingual film or tablet. Buprenorphine is a partial opioid agonist that binds to mu opioid receptors with high affinity but activates them only partially. That partial activation eases withdrawal symptoms and reduces cravings without producing the same degree of euphoria or respiratory depression that full agonists like heroin, oxycodone, or fentanyl can cause. Naloxone is an opioid antagonist added to reduce misuse if the medication is injected; when used under the tongue as directed, naloxone has minimal effect.
SAMHSA describes medications for opioid use disorder as the combination of FDA-approved medications and counseling to treat OUD. That is the model Rolling Hills Recovery Center follows in New Jersey, integrating evidence-based care with whole-person supports.
How it Reduces Withdrawal and Cravings
Withdrawal happens when decreased receptor activation triggers a surge of noradrenergic and other stress signals. Because buprenorphine occupies mu receptors with strong binding, it blocks other opioids and stabilizes the system. The partial agonist activity relieves acute withdrawal and cravings, while the receptor blockade blunts the effect of any opioid used on top.
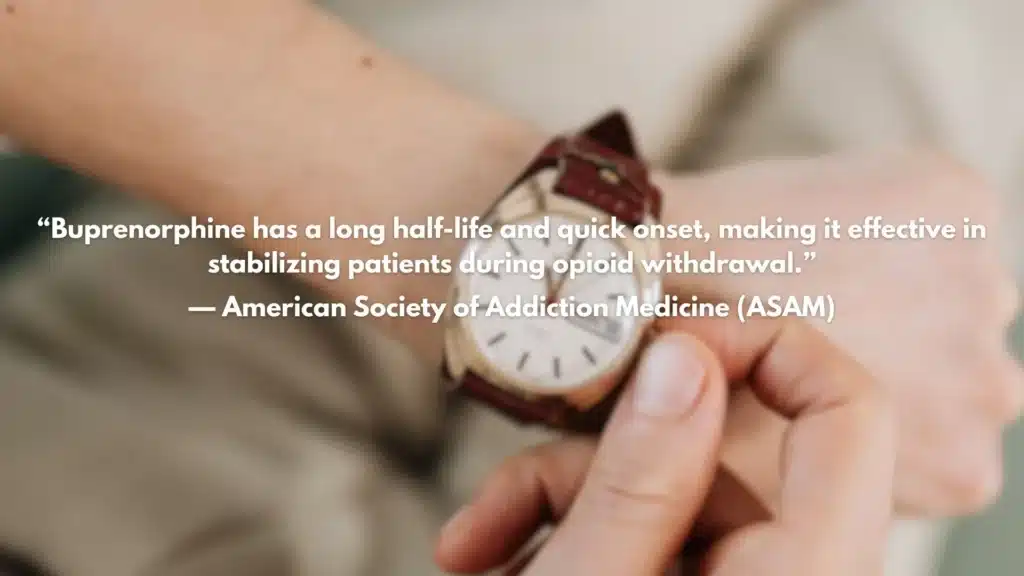
Two practical features matter during withdrawal:
- Fast onset: people usually feel relief within 30 to 60 minutes of the first adequate dose.
- Long half-life: levels are stable over 24 hours, which smooths symptoms across the day and night.
Buprenorphine also has a ceiling effect for respiratory depression. After a certain dose, its ability to slow breathing plateaus, which improves safety relative to full agonists. That ceiling does not mean overdose is impossible, especially with alcohol or benzodiazepines on board, but it is a key safety difference.
Onset, Ceiling Effect, and Real World Outcomes
The question we hear most in early visits is simple. Does Suboxone help with withdrawal? In clinical practice and randomized trials, yes. Most people feel noticeably better within the first few doses, and standard dosing keeps withdrawal controlled within a day or two. More importantly, medications for opioid use disorder reduce overdose deaths and keep people in treatment.
NIDA summarizes the mortality finding clearly. Being on buprenorphine or methadone is associated with about a 50 percent reduction in all-cause mortality compared with being off treatment. The NIH and the ASAM algorithm are aligned on this point.
Reference links:
- NIDA overview of medications to treat OUD: https://nida.nih.gov/research-topics/medications-opioid-use-disorder
- NIH commentary on MOUD and mortality: https://www.nih.gov
As NIDA Director Nora D. Volkow, MD, notes, medications for opioid use disorder save lives.
When to Start and Induction Basics
Timing Your First Dose
Starting too soon can trigger precipitated withdrawal, because buprenorphine displaces full agonists while providing only partial activation. The basic rule is to wait until moderate withdrawal is present.
Clinical Opioid Withdrawal Scale, or COWS, is the standard tool. A COWS score of 8 to 12 or more suggests moderate withdrawal and is a common threshold for starting. You can review COWS with a clinician or use a simplified self-check under guidance.
ASAM and FDA labeling support these timing principles. In northern New Jersey, we also see the fentanyl effect often. People can look or feel ready, then still precipitate. The answer is not to avoid treatment but to adjust the induction plan.
Standard Induction Step-by-Step
A standard office or home induction is straightforward. The key is to go slow enough to avoid precipitated withdrawal, but fast enough to relieve symptoms.
Step 1. Stop opioids and wait for moderate withdrawal. Confirm COWS ≥8 to 12, or clear signs such as yawning, runny nose, gooseflesh, stomach cramps, dilated pupils.
Step 2. First dose 2 mg to 4 mg sublingual buprenorphine naloxone. Let it dissolve fully. Do not eat or drink for 15 minutes after.
Step 3. Reassess in 45 to 60 minutes. If withdrawal persists, add 2 mg to 4 mg.
Step 4. Target total day 1 dose of 2 to 8 mg based on relief and tolerance. Do not chase complete comfort immediately; the goal is clear improvement.
Step 5. Day 2, total daily dose usually 8 to 16 mg in one or two divided doses. Many stabilize at 16 mg per day. Some need 20 to 24 mg. Your prescriber will individualize.
FDA label supports these ranges, and ASAM’s guideline mirrors them. Rolling Hills Recovery Center coordinates with DEA-registered prescribers who follow these protocols and observe the response with the patient.
Fentanyl Exposure and Micro Induction
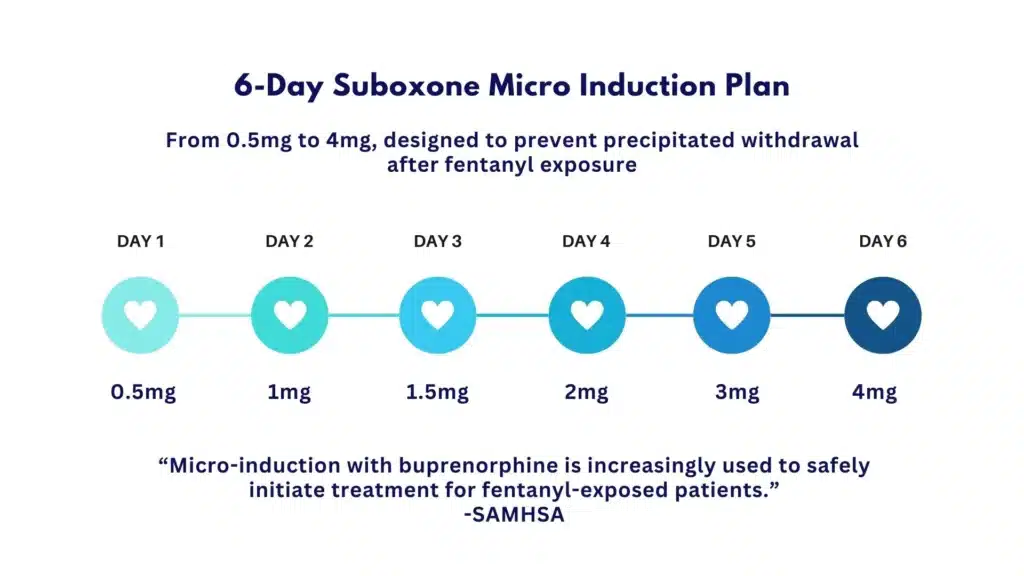
With ongoing fentanyl exposure, the risk of precipitated withdrawal is higher. A micro induction, also called the Bernese method, overlaps very small doses of buprenorphine while the person continues their usual opioid for a few days. The dose of buprenorphine is increased daily, then the full switch occurs without a long washout.
One simple micro-induction sequence used in clinics:
- Day 1: 0.5 mg twice daily while continuing baseline opioid
- Day 2: 1 mg twice daily
- Day 3: 2 mg twice daily
- Day 4: 3 mg twice daily, begin cutting back baseline opioid
- Day 5: 4 mg twice daily, stop baseline opioid
- Day 6 and after: 12 to 16 mg per day maintenance
That is a template, not medical advice. The concept is tiny doses that slowly occupy receptors, so there is no sudden displacement.
A 48-hour Home Induction Template
People often start at home with daily contact from a clinician. Here is a common pattern used by our team and partner prescribers in New Jersey.
Day 0 evening. Last use of a short-acting opioid. Prepare for a morning start. Hydrate, set alarms, arrange a ride if needed, and keep naloxone spray nearby.
Day 1 morning. When COWS is at least moderate, take 2 mg. Wait 45 to 60 minutes. If still uncomfortable, take another 2 mg. Repeat once more if needed. Stop when you feel clear relief. Text or call your prescriber to report the total.
Day 1 evening. If symptoms break through, take an extra 2 mg to 4 mg. Many people end day 1 at 4 to 8 mg total.
Day 2. Take yesterday’s effective total as a single morning dose or split morning and evening, usually reaching 8 to 16 mg total. Continue daily check-ins until stable.
If you are not improving by 2 to 3 hours, call the prescriber. It may be underdosing. If symptoms get sharply worse after a dose, that can be precipitated withdrawal. Do not take more without checking in.
Safety, Side Effects and Interactions
Common and Serious Effects
The most common side effects are nausea, headache, constipation, increased sweating, and sleep changes the first week. These often improve with hydration, gentle movement, and stool softeners. Some feel a dry mouth sensation from the film; rinsing after 15 minutes helps.
Serious risks include respiratory depression when combined with other sedatives, allergic reactions, and rare liver enzyme elevations. The FDA label recommends baseline liver function tests and periodic monitoring. People with severe hepatic impairment may need the buprenorphine mono product or careful dose adjustment.
Precipitated withdrawal is the event to avoid up front. If it happens, the treatment is usually supportive care plus additional small buprenorphine doses under supervision, because continuing doses can reoccupy receptors more fully and reduce symptoms over several hours.
Alcohol, Benzodiazepines, and Other Sedatives
Alcohol, benzodiazepines like alprazolam, zolpidem, pregabalin, and other sedating drugs can increase the risk of slowed breathing, confusion, or falls. ASAM suggests avoiding or reducing other CNS depressants when possible. If a benzodiazepine is prescribed for a clear indication, the prescriber should coordinate doses and monitor closely rather than withhold lifesaving OUD treatment.
We talk about this openly at intake. Safety planning, consent, and pharmacy checks keep people safe.
Special Cases: Liver Disease, Pregnancy, Adolescents
Liver disease. Buprenorphine is metabolized in the liver. Mild to moderate impairment usually still allows standard dosing with monitoring. Severe impairment requires specialist involvement. Baseline LFTs help guide decisions.
Pregnancy. Buprenorphine is considered a first-line medication in pregnancy. Many providers prefer the buprenorphine mono product rather than the combination with naloxone during pregnancy, though emerging data suggest the combo is also acceptable. The priority is to maintain stability and avoid lapses or withdrawal that can stress the fetus. Coordinate with OB care.
Adolescents and young adults. Buprenorphine can be used for OUD in people 16 and older in many settings, with consent requirements based on New Jersey law. Engagement strategies and family support matter a lot in this age group.
Storage, Diversion Mitigation, Naloxone Rescue
Treat Suboxone like any other controlled prescription. Store in a locked box, out of reach of children and pets. Never share or sell it. Many prescribers will use pill counts, prescription drug monitoring program checks, and observed dosing early on to reduce diversion risk. Everyone in the home should know where naloxone spray is kept and how to use it. SAMHSA and state programs can provide naloxone without a prescription, and Rolling Hills Recovery Center distributes it during programming.
FDA label: https://www.fda.gov/science-research/bioinformatics-tools/fdalabel-full-text-search-drug-product-labeling
SAMHSA MOUD overview: https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions
Duration, Tapering and Outcomes
Maintenance vs Taper
Medication is not a short sprint. People do best when they remain on the dose that keeps withdrawal and cravings controlled for as long as they are benefiting. Short tapers of a few weeks have a high relapse risk. Longer maintenance is linked to better retention, less illicit opioid use, lower overdose risk, and improved function.
If you and your clinician choose to taper later, a slow, symptom-guided taper is safer. Examples include reductions of 2 mg every 2 to 4 weeks, with pauses for stressful periods or breakthrough symptoms. Some taper to 2 mg, then use micro decreases of 0.5 mg at a time. There is no medal for speed. There is real harm in rushing.
Combining Medication with Whole-Person Care

Medication treats the biology of OUD. Recovery involves the rest of life, too. Evidence supports combining MOUD with counseling, peer recovery support, case management, and help with sleep, pain, PTSD, or depression. When practical barriers are removed, people stay with care longer. Transportation help, telehealth options, and pharmacy stocking are small fixes that prevent big setbacks.
We pair buprenorphine care with skills-based therapy, relapse prevention planning, and optional holistic services like mindfulness and exercise. The intent is not to replace medication, but to build on it.
Setting Goals and Tracking Progress
Clear, measurable goals help you and your clinician see if the plan works. We suggest a simple dashboard reviewed every 30 to 90 days.
- Cravings trend: number of craving episodes per week
- Sleep: hours per night and number of nights without waking from withdrawal
- Function: attendance at work or school, childcare, or household tasks completed
Add urine toxicology results, emergency visits, and any overdoses to keep the picture honest. The goal is not perfect scores. It is steady movement toward stability that lasts.
Access, Rules and Next Steps
Who Can Prescribe and How to Get an Appointment
Any DEA-registered clinician can prescribe buprenorphine for OUD since the X waiver requirement was removed under federal law. That change opened doors in primary care, psychiatry, and addiction clinics. In practice, local rules and comfort vary.
Rolling Hills Recovery Center helps patients in New Jersey connect with in-house or affiliated prescribers who follow ASAM standards and accept major insurance. If you already have a doctor, we coordinate counseling and recovery supports around their medication plan. If you do not, we start with a same-week assessment, review risks, and schedule an induction plan that fits your life.
If you prefer to search on your own, the SAMHSA treatment locator and the New Jersey state helpline are useful starting points:
- SAMHSA locator: https://findtreatment.gov
- NJ Addiction Services: https://www.nj.gov/humanservices/dmhas/home/hotlines/
Telehealth, Insurance and Pharmacy Steps
Telehealth. Federal flexibilities allow buprenorphine initiation by telehealth in many cases, including audio-only if video is not available, subject to evolving DEA rules and your state’s regulations. New Jersey currently allows telehealth for MOUD with standard documentation. Ask your clinician if an in-person visit is required at any point.
Insurance. Check prior authorization rules before the first prescription. Most plans in New Jersey cover generics without prior authorization, but quantity limits can vary. People sometimes hit delays at the pharmacy if the store does not stock 2 mg films. A quick call 24 hours before induction avoids that surprise.
Pharmacy. Keep the same pharmacy when possible. Ask for naloxone to be dispensed with the first fill. Pharmacists are core members of the care team, and many will counsel on side effects and storage.
What Duboxone does and Does Not Do
What it does. It treats opioid withdrawal and cravings, blocks euphoric effects of additional opioids at sufficient doses, reduces overdose risk while on treatment, and supports long-term stability when combined with counseling and practical supports.
What it does not do. It does not solve pain, depression, or housing by itself. It does not guarantee freedom from relapse. It does not prevent overdose from other sedatives or alcohol. It is not to be mixed casually with illicit benzodiazepines or gabapentinoids.
If you are wondering whether Suboxone can make you feel high, the ceiling effect and partial agonist profile explain why it is much less likely to produce euphoria in people with OUD. For more details, see our discussion on whether someone can get high on Suboxone.
When to Call for Help During Induction
Call your prescriber, urgent care, or 911, depending on severity, if any of the following occur during induction:
- Worsening withdrawal that is severe after a dose and does not improve within 2 hours
- Signs of overdose, such as very slow or stopped breathing, blue lips, or unresponsiveness
- Severe allergic reaction with swelling of lips or tongue, hives, or trouble breathing
If you are not sure, call. Many induction problems are solved with small adjustments. Sometimes a short micro-induction is all that is needed. Our team can also help you decide if a different medication, like methadone or extended-release buprenorphine, is a better fit.
People often reach out when life feels stuck. If you are thinking I want to stop using, but I cannot, that is common and treatable. Our overview on wanting to stop and not being able to covers first steps, including medication options. If substance use is making daily life unmanageable, our page on recognizing when life has become unmanageable can help you sort next actions.
Clinical perspective from Rolling Hills Recovery Center, New Jersey. Our licensed multidisciplinary team uses ASAM-based assessments, collaborates with DEA-registered prescribers for buprenorphine, and integrates therapy, peer support, and recovery coaching. We have seen hundreds of inductions go well with these basics. Wait for moderate withdrawal, start low and reassess often, keep naloxone available, and pair medication with real-life supports. The result is predictable. Sleep improves, cravings fade, and people get back to work, school, or parenting. That is the point.
Conclusion
Suboxone reduces withdrawal and cravings so you can feel steady. Start in moderate withdrawal, dose safely, and pair medication with counseling & recovery support. Watch for side effects, keep follow-ups, and small steps matter.
Frequently Asked Questions (FAQs)
Does Suboxone Help with Withdrawal, and How Fast Will I Feel It?
Yes, Suboxone helps with withdrawal. Most people start to feel relief within 30 to 60 minutes after the first dose, with steadier control by day 2 to day 3 as dosing is adjusted. That early relief comes from buprenorphine partially activating the same opioid receptors to calm symptoms and cut cravings, while naloxone discourages misuse.
Does Suboxone Help with Withdrawal if I’ve Been Using Fentanyl?
It does, but timing and the first doses matter more with fentanyl. Because fentanyl can linger in fatty tissues, starting too soon can trigger precipitated withdrawal. We wait for clear moderate withdrawal signs (COWS about 8 to 12 or higher), or we use micro‑induction, also called the Bernese approach, starting with very small doses like 0.5 to 1 mg and building up while your full‑agonist dose tapers.
When Should I Take the First Dose if I Want Suboxone to Help with Withdrawal?
Start when withdrawal is clearly present to prevent precipitated symptoms. After short‑acting opioids like heroin, oxycodone, or most pills, wait about 12 to 24 hours. After long‑acting opioids or methadone, wait 24 to 48 hours. Aim for COWS 8 to 12 before the first 2 to 4 mg, then reassess every 45 to 90 minutes on day 1 for symptom relief.
Does Suboxone Help with Withdrawal During Pregnancy, and is it Safe?
Yes. Buprenorphine is recommended in pregnancy for opioid use disorder. Many clinicians use the buprenorphine‑only product during pregnancy, and it still helps with withdrawal in the same way. Compared with no treatment, staying on medication lowers overdose risk and improves prenatal care engagement. Compared with methadone, buprenorphine is linked to lower rates and severity of neonatal abstinence syndrome in several studies.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts