Veterans often face substance use alongside PTSD, TBI, chronic pain, and sleep problems. Effective veteran-focused treatment in New Jersey addresses all of it, safely, step by step.
This overview outlines evidence-based treatment, medications, trauma therapies, and practical supports like family involvement & benefits coordination, so recovery is safer, more stable, and built for military culture.
Key Takeaways
- Treat the whole picture: addiction with PTSD, TBI, pain, and sleep. Stabilize first, then add trauma work when ready.
- Begin with screening and labs: AUDIT-C, DAST-10, PCL-5. Medically supervised withdrawal if needed. Use MAT like buprenorphine or naltrexone to reduce cravings; avoid benzos with opioids.
- Use proven therapies. CPT, Prolonged Exposure, EMDR; CBT-I for sleep. Non-opioid pain care and gentle movement, veteran peer mentors, and some telehealth to fill gaps.
- Safety & privacy every step. Naloxone and overdose education; lethal-means safety; 988 and Veterans Crisis Line. HIPAA and 42 CFR Part 2 still apply.
- Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches. Our team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
Overview of Veteran-Specific Needs
Co-Occurring PTSD, TBI, and Moral Injury
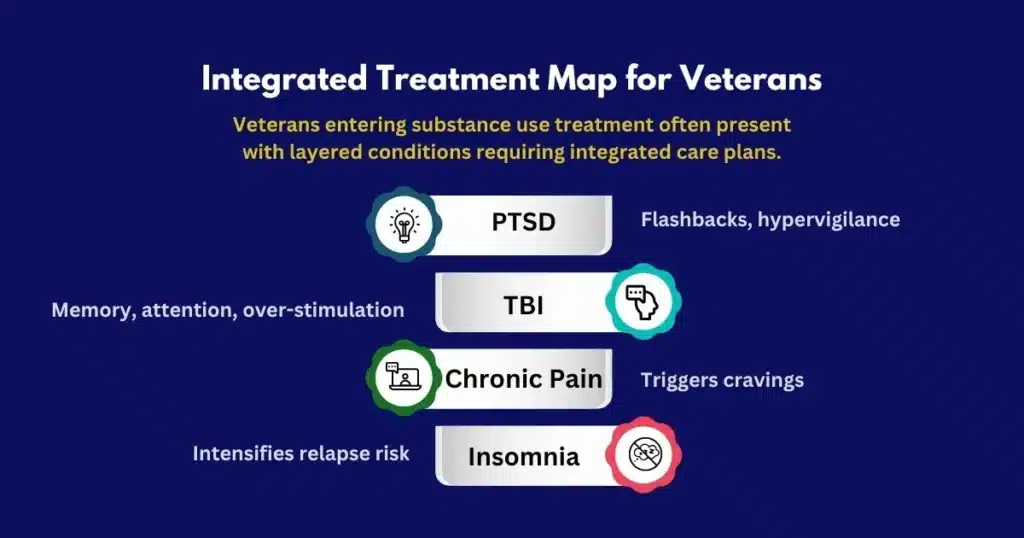
Veterans entering substance use treatment often present with layered conditions:
- Posttraumatic stress disorder (PTSD): re-experiencing, hyperarousal, avoidance, and negative mood changes that can drive alcohol or drug use as coping.
- Traumatic brain injury (TBI): headaches, irritability, memory and attention problems that complicate therapy engagement; avoiding overstimulation and breaking tasks into small steps can help.
- Moral injury: guilt, shame, or betrayal that is not always PTSD, yet deeply impacts recovery. Treatment should include space for values, forgiveness, and spiritual care if desired.
PTSD treatment alongside addiction care plans is most effective when TBI-related accommodations, PTSD stabilization, and moral injury work are integrated rather than siloed. Coordination with neurology or brain injury specialists adds safety.
Chronic Pain and Sleep Disturbance
Many veterans manage chronic pain (musculoskeletal, neuropathic, post-surgical) and long-term sleep disturbance. Pain and insomnia worsen cravings and reduce resilience. Effective rehab considers:
- Non-opioid analgesic ladders; adjuvant agents (gabapentinoids, SNRIs when appropriate)
- Physical therapy, graded activity, and pacing
- Mind-body skills (breathing, biofeedback, mindfulness, gentle yoga)
- Cognitive behavioral therapy for insomnia (CBT-I), with stimulus control and sleep restriction
- Coordinating pain and sleep care to reduce reliance on sedatives
Stigma, Mission-First Culture, and Delayed Help-Seeking
Veterans may underreport symptoms or delay care due to unit cohesion, fear of letting others down, and concerns about privacy. Treatment should:
- Normalize help-seeking as strength
- Offer clear confidentiality rules upfront
- Allow self-paced disclosure
- Use plain language; avoid jargon-heavy advice that feels judgmental
Peer mentors with military experience reduce stigma and increase engagement.
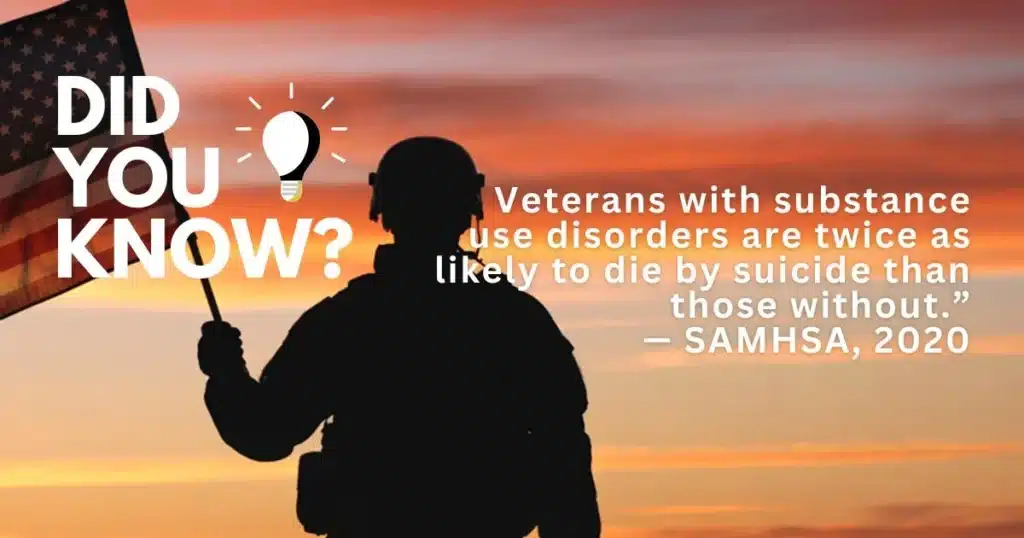
Suicide Risk Screening and Lethal Means Safety
Because suicide risk can be elevated in veteran populations, teams screen at intake and during care. A practical flow:
- Brief screen for suicidal ideation, intent, and past attempts.
- Ask about firearms, medications, and other means at home.
- Create a safety plan; practice it.
- Offer Veterans Crisis Line and 988 information, and verify understanding.
Lethal means safety can include:
- Temporary out-of-home firearm storage, locking devices, or code-sharing for safes
- Smaller medication fills, blister packs, and naloxone on hand
- Daily check-ins during higher-risk periods (post-discharge, anniversaries, acute stress)
Safe Opioid Tapering and Harm Reduction With Naloxone
Safe tapering is gradual and collaborative:
- Stabilize first: address pain, anxiety, and sleep
- Reduce in small steps (5–10% every 2–4 weeks, individualized)
- Monitor withdrawal; treat with clonidine/lofexidine, antiemetics, sleep support
- Offer medications for opioid use disorder (MOUD): buprenorphine, naltrexone; methadone when indicated via OTPs
- Provide naloxone training to patients and families, with practice sessions to reduce hesitation
Harm reduction includes overdose education, using test doses after periods of abstinence, and avoiding mixing opioids with benzodiazepines or alcohol.
New Jersey Access Considerations
In New Jersey, veterans can blend VA and community care options to reduce wait times or access specific evidence-based services.
Rolling Hills Recovery Center coordinates with the VA and TRICARE when eligible, offers a range of outpatient treatment services, and utilizes telehealth when necessary.
Transportation and scheduling support are available; weekend or evening appointments can minimize work and family disruption.
Evidence-Based Treatment Approaches
Assessment: AUDIT-C, DAST-10, and PCL-5
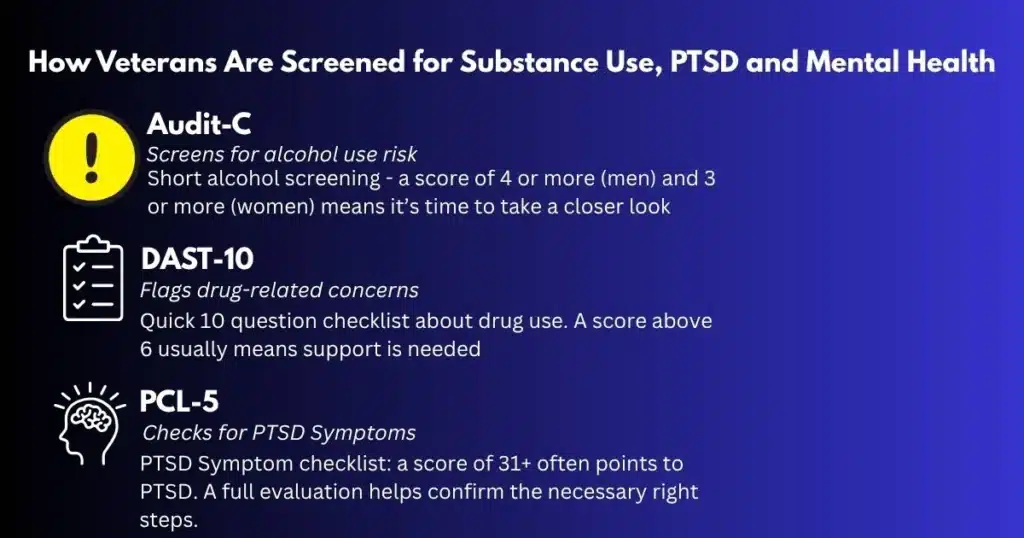
At admission, a structured assessment sets the course:
- AUDIT-C (3 items): identifies risky alcohol use. Scores ≥4 for men or ≥3 for women typically warrant further evaluation.
- DAST-10: screens drug use consequences. Scores 3–5 suggest moderate issues; 6–8 substantial; 9–10 severe.
- PCL-5: assesses PTSD symptoms. A score ≥31–33 indicates probable PTSD; clinical interview confirms.
Step-by-step intake flow:
- Medical and psychiatric history, TBI screen, medication review.
- AUDIT-C, DAST-10, PCL-5 completion; depression/anxiety screen (PHQ-9/GAD-7).
- Suicide and violence risk assessment.
- Pain, sleep, and functional goals.
- Collaborative plan: level of care, medications, psychotherapies, and family involvement.
Templates to use:
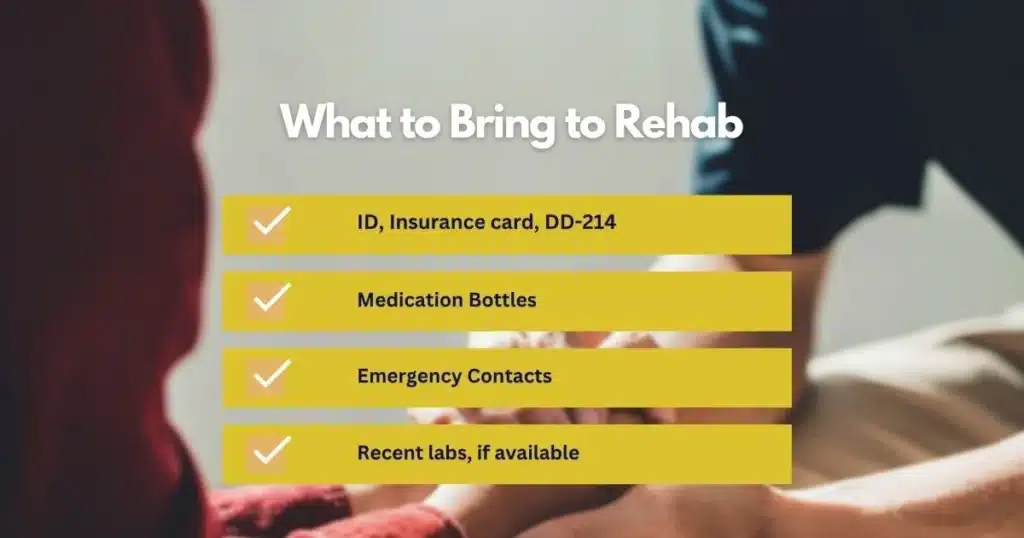
- Intake prep checklist: ID, insurance card, DD-214 if available, medication bottles, emergency contacts, primary care and VA contacts, and recent labs if any.
- Medication list: name, dose, when taken, prescriber, intended purpose, side effects noted.
- Sleep log: bedtime, wake time, awakenings, naps, caffeine, pain level, and next-day mood.
Medically Supervised Withdrawal (Detox)
Withdrawal management is chosen based on substances and medical risk:
- Alcohol: CIWA-Ar guided benzodiazepine or phenobarbital protocols, thiamine to prevent Wernicke’s, fluids, electrolytes.
- Opioids: buprenorphine induction when in moderate withdrawal, symptomatic meds; methadone if indicated via OTPs; later transition to maintenance or naltrexone if appropriate.
- Benzodiazepines: slow, scheduled taper; avoid abrupt stops.
- Stimulants: monitor sleep, mood, and cardiovascular status; treat agitation or depression; nutrition support.
Vital signs, hydration, and mental status are monitored. Plans pivot quickly when complications arise.
Medications for Addiction Treatment and Relapse Prevention
MOUD and relapse prevention medications improve survival, retention, and outcomes. Selection is individualized.
Medication comparison at a glance:
| Medication | Primary Use | Not suitable if opioid analgesia is needed soon | Key Advantages | Considerations |
|---|---|---|---|---|
| Buprenorphine | Opioid use disorder | Start in moderate withdrawal | Reduces cravings; office-based; ceiling effect | Avoid precipitated withdrawal; monitor interactions |
| Naltrexone (oral/extended-release) | Opioid or alcohol use disorders | Opioid-free period required; alcohol no washout | Non-addictive; extended-release monthly option | Not suitable if opioid analgesia needed soon |
| Acamprosate | Alcohol use disorder | Post-acute withdrawal | Helps protracted symptoms; minimal interactions | TID dosing; renal dosing |
| Disulfiram | Alcohol use disorder | After sobriety | Behavioral deterrent | Requires motivation, liver monitoring |
Veterans with chronic pain benefit from buprenorphine’s analgesic properties in certain cases. When opioids are needed temporarily for acute injuries, coordination with prescribers is essential.
For opioid-focused care pathways in New Jersey, see this discussion of rehab for opioid addiction.
Trauma-Focused Psychotherapies: CPT, EMDR, PE
- Cognitive Processing Therapy (CPT): restructures stuck thoughts about trauma, moral injury, and self-blame. Often 12 sessions; homework is key.
- Prolonged Exposure (PE): imaginal and in-vivo exposures reduce avoidance and hyperarousal; careful titration in SUD treatment to prevent overwhelm.
- Eye Movement Desensitization and Reprocessing (EMDR): adaptive information processing to reduce trauma reactivity. Stabilization first, then reprocessing.
- When SUD is active, combine trauma work with craving management and relapse prevention; ensure safety plans and coping skills are practiced weekly.
CBT for Insomnia and Pain
CBT-I pillars:
- Consistent wake time
- Sleep restriction based on average sleep time
- Stimulus control: bed only for sleep and intimacy
- Cognitive work: reduce catastrophic sleep thoughts
- Relaxation training and sleep hygiene
CBT for chronic pain:
- Activity pacing and graded exposure to movement
- Thought reframing about pain danger
- Flare plans: heat/ice, breath work, gentle stretching, short walks
- Aligning goals around function, not pain elimination
Tools:
- Sleep window calculator (based on 2-week sleep log)
- Pain flare card: “Stop-Breathe-Plan” steps and preferred tactics
Integrated Care for Depression and Anxiety
Substance use often masks or worsens mood disorders:
- Antidepressants (SSRIs/SNRIs) are used alongside therapy
- Anxiety management without heavy reliance on benzodiazepines; consider hydroxyzine, buspirone, or gabapentin when appropriate
- Behavioral activation, exposure, and skills-based therapies
Pacing is important in TBI or severe insomnia. Consider neuropsychological input for attention/executive function support.
Peer Support With Veteran Mentors and Telehealth When Needed
Peer specialists with service experience help translate between military culture and civilian healthcare teams. Veterans often accept feedback faster from those who have “worn the boots.”
Telehealth:
- Secure video visits for therapy, med management, and family sessions
- Evening tele-visits to maintain work schedules
- Safety planning and crisis protocols adapted for virtual sessions
How Rolling Hills Recovery Center Aligns Care
Rolling Hills Recovery Center blends evidence-based treatment with holistic supports, mindfulness, movement, nutrition, and family involvement. Veterans receive:
- Structured assessment and personalized care plans
- MAT when indicated, alongside trauma-focused care
- Pain and sleep programs; telehealth and peer support
- Coordination with VA and TRICARE for benefits and continuity
- Flexible outpatient options for those not needing residential care; learn more about our outpatient programs
Navigating Coverage and Care Pathways in NJ
VA Eligibility and Community Care Referrals
Many veterans qualify for VA health benefits. To access community care under the VA’s Community Care Program:
- Confirm VA eligibility and enrollment (by phone or online portal).
- Discuss local access with a VA provider; if VA can’t provide care timely or locally, a Community Care referral can be initiated.
- VA authorizes approved services and duration; obtain the authorization letter.
- Share authorization with the community provider; ensure scheduling aligns with the authorized timeframe.
- Provide updates to the VA clinician to maintain coverage continuity.
Tips:
- Keep copies of DD-214, VA ID, and authorization letters
- Verify if substance use treatment, meds, and lab work are included in the authorization
- Ask about transportation allowances, where available
TRICARE Coordination
For active-duty, Guard/Reserve, or certain retirees and families:
- Identify plan type (Prime, Select, Reserve Select)
- Obtain referral/authorization if required for residential or intensive outpatient
- Verify network status and copays
- Coordinate with command (if active-duty) for duty limitations and privacy considerations
Rolling Hills helps verify coverage and can coordinate with TRICARE care managers as needed.
Verifying Benefits, Documentation, and Costs
A simple benefits check process:
- Call the admissions team with your insurance card details.
- Provide any VA Community Care authorization if applicable.
- Share a list of current medications and prescribers.
- Receive a written summary of covered services, estimated out-of-pocket costs, and timelines.
- Clarify prior authorization requirements for MAT or specialty therapies.
For more details on coverage and next steps, see our page on insurance for drug rehab in NJ.
Documents to bring:
- Photo ID, insurance card(s), VA or TRICARE authorization
- DD-214 if available, medication bottles, emergency contacts
- Names and contact info for VA PCP, mental health clinician, or case manager
Transportation and Practical Support
- Ask about shuttle options, mileage reimbursement, and parking
- NJ Transit planning support; consider off-peak appointments
- Telehealth for days with limited mobility, family duties, or weather concerns
- For mobility devices or service animals, coordinate in advance so rooms and therapy spaces are prepared
Collaboration Between Community Clinicians and VA Providers
Continuity reduces relapse risk. Best practices:
- Consent forms signed up front for VA and community care exchange (42 CFR Part 2-compliant)
- Share treatment plan, medication changes, and safety plans within 72 hours of major changes
- Monthly brief updates to VA or TRICARE care managers
- Warm handoffs back to VA services for specialty follow-up (e.g., TBI clinic, pain management, PTSD programs)
Discharge Planning Back to VA or Primary Care
Start discharge planning at admission:
- Schedule follow-up with VA or primary care within 7 days
- 30-day supply of medications or enough until next appointment
- Recovery plan: relapse prevention, safety plan, crisis contacts
- Referral to alumni or local veteran peer groups
- Confirm transportation for the first two aftercare visits
Checklist items:
- Printed med list and MOUD appointment date/time
- Therapy schedule and telehealth links
- Naloxone provided and practiced
- Family session completed or scheduled
Family Involvement & Recovery Supports
Family Therapy, Boundaries, and Communication Skills
Family involvement often improves outcomes:
- Education on addiction as a chronic condition
- Boundary-setting that supports recovery without enabling
- Communication skills: reflective listening, “I” statements, time-outs during conflict
- Joint safety planning for crisis signals and steps
Short family sessions can be offered via telehealth when distance is a barrier.
Spiritual and Moral Injury Work
For veterans experiencing moral injury:
- Values clarification exercises
- Chaplain or spiritual care referral if desired
- Practices for self-forgiveness and meaning-making
- Peer groups focused on service stories and identity in civilian life
These interventions are optional and tailored to individual beliefs.
Housing and Employment Linkages
Recovery stabilizes when basic needs are met:
- Referrals to veteran-preference housing programs, where applicable
- Coordination with vocational rehab, job placement, or education benefits
- Letters documenting treatment participation are useful for housing courts or employers (with consent)
Sober Social Connection and Contingency Plans
Social recovery steps:
- Buddy system for meetings; veteran-specific peer groups
- Activity list: hiking, fitness, community volunteering
- Digital boundaries: remove dealer contacts; block numbers; change routines
Contingency plan for high-risk triggers:
- Identify top 3 triggers (pain spike, insomnia, anniversary dates)
- Early warning signs (restlessness, isolation, anger)
- Fast actions: call peer, use grounding skills, take a walk, review values card
- Medication adherence check and naloxone location
- If risk escalates: call 988 or Veterans Crisis Line, or present to the nearest ED
Templates:
- Trigger-response card (wallet size)
- 3-step crave plan: Delay, Distract, Decide
- Pain flare protocol: 15-minute pacing cycle and coping menu
- Sleep reset: 20-minute get-out-of-bed plan
Crisis Resources: 988 and Veterans Crisis Line
- Dial 988, then press 1 for the Veterans Crisis Line. You can also text 838255 or chat online.
- Store these contacts in your phone under ‘ICE’ (In Case of Emergency).
- Family members should learn how to start the conversation: “I’m worried about your safety; can we call together?”
Safety, Privacy, and Legal Protections
HIPAA & 42 CFR Part 2
- HIPAA protects health information; 42 CFR Part 2 adds extra safeguards for substance use treatment records.
- Written consent is needed to share SUD treatment details with specified recipients and time limits.
- Veterans can authorize limited information sharing with VA, TRICARE, or specific clinicians to streamline care and still keep sensitive details private.
- Patients can revoke consent at any time; document changes clearly.
Lethal Means Safety and Overdose Education
- Discuss firearms storage options respectfully; acknowledge training and responsibility culture within the military.
- Offer lockboxes, cable locks, and safe-storage education; encourage distance and delay during high-risk periods.
- Naloxone kits for anyone at risk of opioid exposure; teach recognition of overdose (unresponsive, slow or no breathing, pinpoint pupils) and rescue steps.
- Emphasize not using alone; if alone, use check-in systems or call lines.
Overdose response steps:
- Call 911.
- Administer naloxone; repeat in 2–3 minutes if no response.
- Rescue breathing if not breathing; chest compressions if no pulse.
- Stay with the person until help arrives.
Trauma-Informed and Culturally Competent Care
- Assume trauma exposure; avoid unnecessary triggers (loud noises, closed doors without consent).
- Offer seating choices; explain each step before starting; ask for consent routinely.
- Respect service era, branch, MOS, and deployment history. Avoid stereotypes. Let the veteran define their experience.
- Encourage strengths-based language: resilience, skills, values, and team mindset.
Practical How-To Steps and Tools
Starting Treatment This Week
- Call admissions to confirm availability and level of care.
- Gather ID, insurance, and relevant VA paperwork.
- Prepare a medication list and symptom priorities (top 3).
- Arrange transport; ask about telehealth if needed.
- Plan for first 72 hours: sleep schedule, meals, and family communication.
A Simple Safety Plan Template
- Warning signs: list 3 thoughts, feelings, or behaviors.
- Internal coping: breath work, grounding, brief walk, music.
- Social supports: names and numbers of 2 people.
- Professional supports include therapists, clinic lines, 988, and the Veterans Crisis Line.
- Environmental safety: lockbox locations, naloxone location, medication management.
- Reasons for living: two values or future goals.
Daily Recovery Routine Template
- Morning: meds, hydration, 10 minutes of movement
- Midday: peer check-in or brief skill practice
- Evening: CBT-I wind-down routine; no screens 1 hour before bed
- Weekly: therapy session, group, and family call
- Monthly: treatment team review, VA/PCP follow-up
Pain and Sleep Tools
- Pain log: intensity (0–10), trigger, action taken, result.
- Sleep log: bed/wake times, awakenings, caffeine, next-day function.
- Flare kit: heat pack, stretching card, paced breathing steps, distraction list.
When Outpatient Care Fits
Not all veterans need residential treatment. Intensive outpatient or standard outpatient may be right when:
- Home is safe
- No severe withdrawal risk
- Supportive family or peer network available
- Work or school can continue with adjustments
Flexible options keep life stable while care proceeds. See more about local outpatient approaches through our outpatient programs.
Helpful References for Clinicians and Families
- U.S. Department of Veterans Affairs: VA Substance Use Programs
- National Center for PTSD: PTSD resources and treatments
- National Institute on Drug Abuse: Substance Use and Military Life (overview and research)
- Department of Defense Psychological Health Center of Excellence: PHCoE
- Centers for Disease Control and Prevention: Opioid Overdose Prevention
For those focusing on opioid-related recovery in New Jersey, Rolling Hills Recovery Center offers multidisciplinary care, medication treatment when indicated, and coordination with VA and TRICARE. Learn more about our approach to rehab for opioid addiction.
Conclusion
Recovery for veterans works best when addiction and related PTSD, pain, and sleep issues are treated together. Top points: solid assessment and MAT when needed; trauma care with family support; tight coordination for safety.
Rolling Hills Recovery Center is a luxury rehab center in New Jersey offering evidence-based and holistic care.
Our experienced team helps people overcome substance abuse and reach lasting results. Start today, call & explore our programs.
Frequently Asked Questions (FAQs)
What is Drug Rehab for Veterans, and Why Must PTSD and Addiction be Treated Together?
Drug rehab for veterans addresses substance use along with service-related conditions like PTSD, traumatic brain injury, chronic pain, and sleep problems.
Treating PTSD and addiction together reduces relapse risk, improves mood and sleep, and helps the brain relearn safer coping.
Care is trauma‑informed, evidence‑based, and paced so stabilization, therapy, and medications work in sync.
How Do Clinicians Start Addiction Care for Veterans with PTSD?
Care begins with a thorough assessment: substance history, PTSD symptoms, depression and anxiety screens, pain and sleep review, meds, labs, and safety.
If needed, medically supervised withdrawal comes first; then medication for addiction (for example, buprenorphine or naltrexone) and for PTSD or sleep as appropriate.
Next steps include trauma therapies timed to stability, skills for cravings and stress, non‑opioid pain strategies, and a relapse‑prevention plan. Coordination with VA benefits or TRICARE in New Jersey helps keep care continuous.
Which Therapies and Medicines are Used for Veterans?
Clinicians commonly use trauma‑focused therapies such as Cognitive Processing Therapy, Prolonged Exposure, and EMDR, plus CBT skills, mindfulness, and CBT‑I for insomnia.
For addiction, medication may include buprenorphine or methadone for opioid use disorder, naltrexone or acamprosate for alcohol use disorder; for PTSD, SSRIs like sertraline or paroxetine, and prazosin for nightmares.
Benzodiazepines are usually avoided in PTSD with substance use. Plans are individualized and monitored closely, safety first.
How Can Family and Community Support Recovery for Veterans Facing Addiction?
Family therapy teaches boundaries, calm communication, and how to spot triggers without blame. Peer support from veteran mentors helps translate military culture into recovery skills.
Safety planning covers lethal means safety and overdose education, including naloxone. Simple routines around sleep, pain management, and movement matter more than people think. If suicidal thoughts arise, seek help right away…
What makes Rolling Hills Recovery Center a Strong Choice for Veterans with PTSD and Addiction in New Jersey?
Rolling Hills Recovery Center is a drug and alcohol rehab and addiction treatment center in New Jersey that offers evidence-based addiction treatment and holistic approaches.
The team of experienced professionals is dedicated to helping individuals overcome substance abuse and achieve lasting results.
Veterans can expect comprehensive assessment, trauma‑informed care, medication‑assisted treatment when appropriate, integrated PTSD therapies, and coordinated discharge planning.
Privacy is protected under HIPAA and 42 CFR Part 2, and care is aligned with each veteran’s values and goals.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












