Understanding the stages of alcoholism helps families and patients spot problems earlier and choose safer care. This overview explains how risky drinking can progress, what signs matter in each stage, and when medical help is essential. It draws on evidence-based standards, clarifies withdrawal risks, and outlines practical steps for compassionate, effective support & recovery.
Key Takeaways
- Alcohol use disorder moves in patterns; DSM‑5 uses 11 criteria to rate severity, while “early, middle, late” stages describe real‑world changes like craving, loss of control, tolerance, and withdrawal
- Early signs matter: rising tolerance, drinking after stress, secrecy, blackouts, morning “relief” drinks; don’t stop suddenly if dependent, withdrawal can cause seizures & delirium tremens
- Screening and next steps: quick tools (AUDIT‑C, CAGE), look for anxiety or depression, consider brief intervention early; when use is heavier, evidence‑based care like CBT, contingency management, plus FDA‑approved medicines (naltrexone, acamprosate, or disulfiram) help
- Safety first: medical detox for moderate to severe dependence; monitor symptoms (CIWA‑Ar), support sleep & nutrition, avoid driving during withdrawal; family support improves outcomes
Definition and Models of “Stages of Alcoholism” (AUD)
DSM‑5 Alcohol Use Disorder Framework
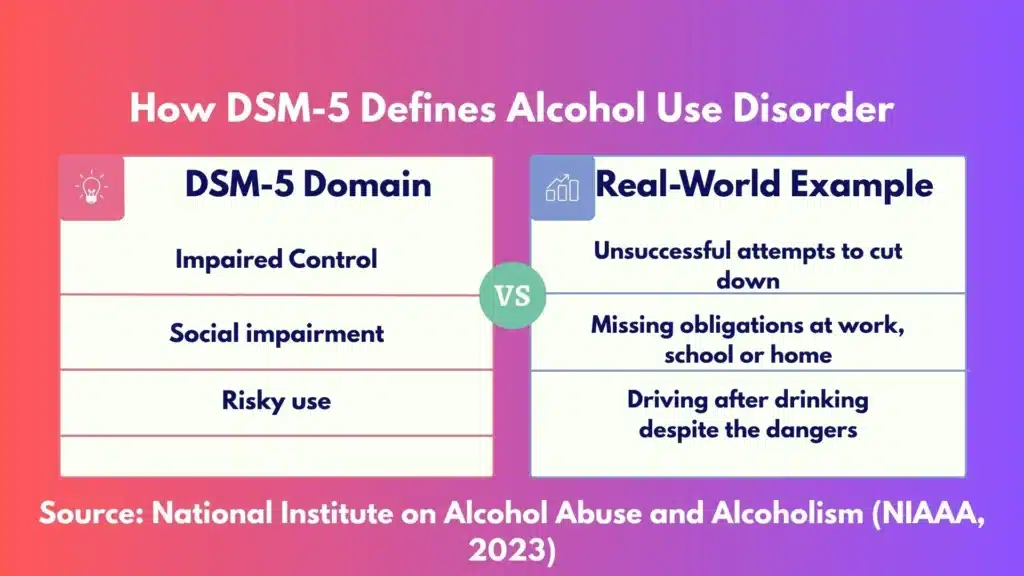
Clinicians diagnose Alcohol Use Disorder (AUD) using DSM‑5 criteria, 11 items that capture impaired control, social impairment, risky use, and pharmacologic indicators (tolerance and withdrawal). Severity is based on how many criteria are met:
- Mild: 2–3 criteria
- Moderate: 4–5 criteria
- Severe: 6+ criteria
This model emphasizes a spectrum rather than fixed stages. People move forward and back on that spectrum over time. Remission is common with proper care.
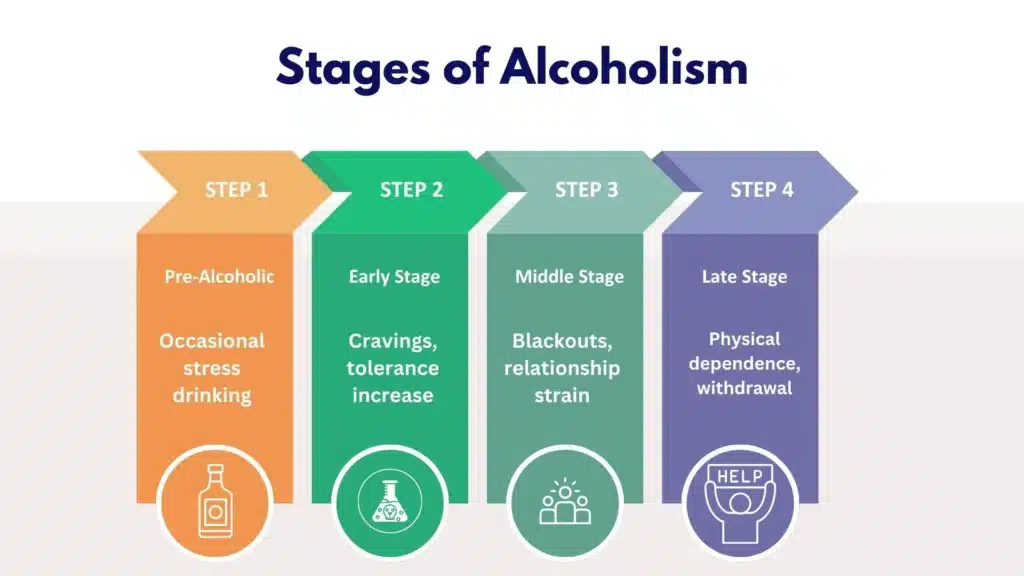
Public‑Facing Stage Models (Jellinek Pattern)
Outside the clinic, many articles describe a four‑stage progression: pre‑alcoholic or at‑risk, early, middle, and late/chronic. That framework comes from Jellinek’s observations and is useful for education.
It highlights how patterns escalate and how consequences accumulate. Still, life doesn’t always follow a neat sequence. People can pause in one stage, skip ahead, or enter remission with help.
Shared Core Concepts
Using either model, certain themes are consistent:
- Tolerance rises: more alcohol is needed for the same effect.
- Loss of control appears: drinking more or longer than intended, failed cut‑downs.
- Craving increases: strong urge or preoccupation with alcohol.
- Withdrawal emerges: tremor, nausea, sweating, anxiety, or seizures when alcohol is reduced or stopped.
- Life domains are affected: conflicts at home, poor work performance, legal and financial strain, mood and sleep disturbances.
At Rolling Hills Recovery Center in New Jersey, clinicians combine the diagnostic clarity of DSM‑5 with the approachable language of stages to explain risk and plan care that is practical.
Evidence‑based therapies are paired with holistic supports that address stress and family repair.
Stages with Key Signs and Symptoms
Pre‑Alcoholic or At‑Risk Stage
This phase is often overlooked. Drinking is socially acceptable and may not seem “problematic.” Common signs:
- Drinking primarily to relax, sleep, cope with stress, or reduce anxiety
- Rising tolerance, needing an extra drink to unwind or feel the effects
- Occasional over‑drinking at events; mild next‑day regrets
- No major life consequences yet, but subtle shifts: less interest in alcohol‑free activities; thinking about the next opportunity to drink
These patterns often correspond to one DSM‑5 criterion, drinking more or longer than intended, or to risky use without clear impairment. A person might not meet AUD yet, or might be mild.
Early Stage
Red flags start to appear:
- Blackouts or partial memory gaps after drinking
- Binge drinking alcohol in excessive amounts
- Hiding alcohol or minimizing amounts to others
- Morning “eye‑openers” to steady nerves or ease a hangover
- First failed attempts to cut down; drinking takes more time than planned
- Sleep fragmentation, irritability, and anxiety on days without alcohol
At this point, two to three DSM‑5 criteria are common: impaired control, craving, and risky use. The pattern signals mild AUD and calls for early intervention.
Middle Stage
Consequences become less avoidable and more frequent:
- Repeated failed cut‑downs despite good intentions
- More time spent obtaining, using, and recovering from alcohol
- Conflict with family or co‑workers; poor focus; late or missed days
- Gastrointestinal issues (gastritis, heartburn), night sweats, tremor
- Sleep problems, mood swings, depressive symptoms, or elevated anxiety
Here, four or more DSM‑5 criteria are often present. Moderate AUD is common, and withdrawal symptoms may start after short abstinence. Medical assessment is important.
Late or Chronic Stage
Physical dependence and complications dominate:
- Strong withdrawal with reduced intake: tremor, sweating, agitation, nausea; severe cases can include seizures or delirium tremens (confusion, fever, unstable vital signs)
- Organ damage: alcoholic hepatitis, cirrhosis signs (jaundice, fluid retention), pancreatitis, impaired immunity, neuropathy
- Cognitive changes: poor concentration, memory problems; risky behaviors to maintain use
- Social failure points: job loss, legal issues, relationship rupture
Six or more DSM‑5 criteria typically apply. Severe AUD requires comprehensive care; stopping suddenly can be dangerous, and sometimes alcohol withdrawal is life‑threatening.
Mapping Stages to DSM‑5 Domains
- Impaired control: early failed cut‑downs, escalating amounts, craving; prominent from early through late stages.
- Social impairment: conflict at home or work, withdrawal from hobbies; increases in the middle stage.
- Risky use: drinking before driving, combining with sedatives, use despite health warnings; often early and persistent.
- Pharmacologic indicators: tolerance appears in the pre‑alcoholic/early stage; withdrawal emerges in the middle and late stages.
A brief comparative view to orient patients and families:
| Public stage (Jellinek pattern) | Common signs | DSM‑5 severity tendency | Notes |
|---|---|---|---|
| Pre‑alcoholic / At‑risk | Stress‑drinking, rising tolerance, planning around alcohol | No AUD or Mild (0–2 criteria) | Best window for prevention and education |
| Early | Blackouts, hiding use, morning relief | Mild (2–3 criteria) | Strong response to brief intervention |
| Middle | Failed cut‑downs, GI symptoms, mood swings | Moderate (4–5 criteria) | Withdrawal risk begins; structured care needed |
| Late / Chronic | Physical dependence, organ damage, cognitive decline | Severe (6+ criteria) | High withdrawal risk; medical detox and integrated care |
Screening and Diagnosis
Quick Self‑Checks You Can Do Now
Brief tools help decide whether to seek a professional assessment. Use them honestly; they are starting points, not labels.
- AUDIT (Alcohol Use Disorders Identification Test): 10 questions, score 0–40. Scores of 8+ suggest hazardous or harmful use; 16+ indicates high risk; 20+ often signals possible dependence that warrants specialist care.
- AUDIT‑C: 3 questions focusing on frequency and quantity. Positive screens typically: 4+ for men, 3+ for women or adults over 65. Higher is higher risk.
- CAGE: 4 Yes/No items (Cut down, Annoyed, Guilty, Eye‑opener). A score of 2+ suggests clinically significant risk; 3–4 is very concerning.
If scores are positive, schedule a conversation with a clinician or an addiction specialist. If withdrawal symptoms have ever happened, seek medical care first.
When to See a Clinician and What They Assess
A clinician will review:
- Drinking pattern (daily and weekly), contexts, and consequences
- DSM‑5 criteria count and severity
- Past withdrawals, seizures, or delirium
- Medical history (liver, pancreas, heart, pregnancy status), medications, and supplements
- Mental health (anxiety, depression, PTSD), sleep, pain, and trauma history
- Safety risks such as driving, falls, or mixing alcohol with sedatives (benzodiazepines, opioids)
Professional diagnosis supports the right level of care. It also clarifies whether outpatient support is safe or if inpatient detox is the safer start.
Labs and Withdrawal Risk Tools
Bloodwork can show patterns linked to heavy drinking. Common findings include macrocytosis (elevated MCV), elevated GGT, and AST greater than ALT (often >2:1 in alcoholic liver disease).
Folate deficiency may be present. Not everyone shows lab changes, especially early on.
In clinical settings, withdrawal severity is measured with the CIWA‑Ar scale. Scores under 10 suggest mild withdrawal; 10–18 moderate; over 18 severe and higher risk of complications such as seizures or delirium.
High‑risk features include prior severe withdrawal, older age, very heavy daily intake, co‑use of sedatives, fever, or unstable vital signs. Do not attempt to detox at home if serious withdrawal is possible.
Co‑Occurring Conditions to Consider
Anxiety, depression, bipolar disorder, ADHD, and trauma‑related disorders frequently overlap with AUD and can drive relapse if left untreated. Sleep apnea, chronic pain, and GI disorders also deserve attention.
Coordinating care across these areas, with a single plan and shared goals, improves outcomes.
Stepwise Help by Stage

If in the Pre‑Alcoholic or Early Stage
Brief interventions can be enough to change course.
- SBIRT model: Screening, Brief Intervention, and Referral to Treatment. A 10–15 minute motivational conversation can lower risky use.
- Motivational interviewing: explores ambivalence, aligns change with personal values, and sets goals that feel doable.
- Harm‑reduction goals: set safer limits, alternate with alcohol‑free days, avoid drinking before driving or when on sedating medications.
A simple plan:
- Write down a two‑week target (for example, no more than 2 drinks per day and no more than 7 per week for women or adults over 65; no more than 3 per day and 14 per week for most men, adapted from national guidelines). 2) Schedule at least three alcohol‑free days weekly. 3) Track drinks with a tally card or phone note. 4) If targets are missed twice, consider stepping up care rather than trying harder alone.
If blackouts, morning relief drinking, or rising tolerance appear, speak with a clinician. Early use of naltrexone (daily or targeted to high‑risk situations) reduces heavy‑drinking days for many people, especially those without dependence.
If in the Middle Stage
Medical safety comes first. If withdrawal has occurred, ask about monitored detox. For many, intensive outpatient or partial hospitalization programs are appropriate; others may need inpatient stabilization if medical or psychiatric risks are high.
Evidence‑based therapies:
- Cognitive Behavioral Therapy (CBT) to map triggers and build coping skills
- Contingency Management (CM) to reinforce progress with tangible rewards
- Motivational interviewing throughout care to keep change personalized
Medications for AUD:
- Naltrexone (oral daily or monthly extended‑release injection) to reduce craving and heavy‑drinking days; avoid if on opioids or with acute hepatitis; monitor liver function
- Acamprosate to support abstinence and reduce post‑acute withdrawal symptoms; adjust for kidney function; take three times daily
- Disulfiram as an aversive agent for selected, highly motivated patients, with monitoring and clear education
Practical steps: arrange medical evaluation, discuss medication options, set weekly therapy appointments, and write a relapse prevention plan that lists triggers, warning signs, and early actions.
If in the Late or Chronic Stage
Do not stop abruptly without medical guidance. The risk of seizures or delirium tremens is serious. A physician can supervise detox with benzodiazepine protocols, vitamins (thiamine to prevent Wernicke’s encephalopathy), fluids, and electrolyte correction.
Co‑occurring conditions, depression, trauma, and liver disease, need parallel attention.
After stabilization, longer‑term rehabilitation helps rebuild health, work, and relationships. Combining medications, structured therapy, peer recovery, and family engagement yields the best odds.
Nutrition support, sleep treatment, and physical therapy can help with neuropathy and fatigue.
Ongoing Recovery Supports and Relapse Prevention
Mutual‑help groups such as AA, SMART Recovery, Refuge Recovery, and other peer communities can complement professional care. The fit matters more than the name.
Digital recovery apps and check‑ins can support daily accountability.
Relapse prevention is a living document. Include high‑risk people, places, and times; alternate plans (leaving early, a call list, a ride share); medication adherence; and a 72‑hour recovery action plan if a slip occurs.
Small lapses do not erase progress; rapid course‑correction does.
Family Involvement and Workplace Considerations
Family members can learn to set clear, compassionate boundaries and stop inadvertently enabling. Structured family sessions reduce blame and increase practical support.
At work, consider confidential conversations with HR about leave or accommodation if treatment will disrupt schedules. Returning to work with a plan, breaks, support calls, and medical follow‑up improves stability.
Safety Notes
- Do not detox alone if moderate or severe symptoms are likely.
- Never mix alcohol with benzodiazepines, sleep medications, or opioids.
- If there is suicidal thinking, chest pain, severe confusion, or seizure, call emergency services right away.
- Pregnant individuals should avoid alcohol entirely and seek prenatal and addiction care promptly.
Practical Tools and Templates
Drink‑log template (paper or phone note): Date, start time, place, who with, number of standard drinks, what helped you stop or slow down, mood before and after, hours of sleep.
Total drinks per day at the bottom; weekly total on Sundays. Standard drink count matters: 12 oz beer (5%), 5 oz wine (12%), 1.5 oz spirits (40%).
Change plan template (one page):
- Personal reasons to change (health, family, work, money, sleep).
- Goal for the next 2 weeks (abstinence or reduced use with specific numbers).
- Triggers to avoid (list top three) and coping actions (two per trigger).
- Support team (people, times to call or text, meetings).
- Medication plan (which, dose, start date, who prescribes, side‑effect plan).
- Early warning signs (craving spikes, isolation, skipping meals) and first steps if noticed (call therapist, attend a meeting, reschedule a high‑risk event).
- Reward for meeting the two‑week goal (healthy, meaningful).
How to do a safer trial change:
- Pick a start date that avoids major stressors. 2) Tell two people who will check in. 3) Remove alcohol from the home and plan non-alcoholic alternatives you like. 4) Eat regular meals and hydrate; poor nutrition amplifies withdrawal and craving. 5) If tremor, sweating, significant anxiety, or nausea appear, pause and contact a clinician, medical support may be required.
Workplace script (if needed): “I’m addressing a health issue and following my doctor’s plan. I may need temporary schedule adjustments to attend appointments. I’m committed to my role and will keep you updated within policy.”
Treatment at Rolling Hills Recovery Center (NJ)
Rolling Hills Recovery Center blends evidence‑based treatment with holistic care to address every stage of AUD. Patients are assessed with DSM‑5 criteria and medical screeners to match the level of care, from outpatient therapy to higher‑intensity supports.
Core services include CBT, Motivational Interviewing, and DBT, paired with individual counseling, family sessions, and relapse prevention planning.
When appropriate, medications for AUD (naltrexone, acamprosate, disulfiram) are offered through an outside provider with close monitoring and coordination with primary care or specialists.
For an overview of program options and integrated supports, see our alcoholism treatment facility.
If a medical start is needed, our team outlines safe medical treatment for alcoholism, including supervised detox with our partners and step‑down care.
To understand how comprehensive care fits together across settings, explore the role of substance abuse clinics and how collaboration boosts long‑term results.
Patients and families receive clear education, steady encouragement, and concrete tools that make day‑to‑day recovery workable.
Screening and Stage‑Specific “How‑To” Actions at a Glance
- Pre‑alcoholic/At‑risk: Do AUDIT‑C and set a 2‑week trial limit; schedule alcohol‑free days; experiment with targeted naltrexone if indicated and prescribed; track with a daily log.
- Early stage: Add CBT skills training; write a relapse prevention plan; consider daily or targeted naltrexone; join a supportive peer meeting; review sleep and anxiety care.
- Middle stage: Get medical assessment for withdrawal risk; consider structured outpatient or partial hospitalization; start medication‑assisted treatment; family sessions to reset boundaries; protect work functioning.
- Late stage: Medically supervised detox; treat co‑occurring conditions; consider inpatient or intensive step‑down; nutrition and thiamine; strong relapse prevention plan; ongoing medication and therapy follow‑up.
Health Impacts Worth Noting: Why Earlier is Better

Alcohol affects nearly every organ. Even before cirrhosis, fatty liver and alcoholic hepatitis can progress silently. Pancreatitis can be severe and recur; blood pressure rises; atrial fibrillation risk increases after heavy episodes.
Cancer risk climbs with higher intake, oral cavity, throat, esophagus, liver, colon, and breast. Sleep quality suffers; mood disorders worsen; injuries and accidents are more likely.
Early behavior change reduces these risks quickly, and many organ systems improve within weeks to months.
For Clinicians and Informed Patients: Practical Mapping to DSM‑5
A quick mental model helps in visits:
- 0–1 DSM‑5 criteria: risky use; brief intervention and monitoring.
- 2–3 criteria: mild AUD; MI, CBT skills, trial of medication if clinically indicated.
- 4–5 criteria: moderate AUD; assess withdrawal; structured program and medication.
- 6+ criteria: severe AUD; evaluate for medical detox; integrated, multi‑modal plan.
Tie each newly met criterion to a specific care step. For example, if “time spent using or recovering” shows up, add contingency management and scheduling tools; if “social role failure” appears, fold in family sessions and workplace planning.
Common Pitfalls and How to Avoid Them
- Waiting for a “rock bottom.” In practice, outcomes are better with early and moderate‑stage care.
- Stopping suddenly after heavy daily use. This can be dangerous; pre‑plan with a clinician.
- Skipping nutrition. Balanced meals and hydration lower withdrawal severity and craving.
- Ignoring sleep and anxiety. Treating these directly reduces relapse risk.
- Over‑relying on willpower alone. Skills, supports, and sometimes medication make the difference.
Search Recap and Trusted References
An earlier search returned empty ([]), so this outline relies on consensus clinical sources and current public health guidance familiar to addiction specialists. Key references include:
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Core Resource on Alcohol Use Disorder– DSM‑5 criteria, progression, and treatment principles
- NIAAA “Rethinking Drinking”– risk limits, standard drink sizes, and change tools
- Substance Abuse and Mental Health Services Administration (SAMHSA) on SBIRT – screening and early intervention
- Centers for Disease Control and Prevention (CDC) Alcohol and Public Health – health impacts and data
- World Health Organization (WHO) alcohol fact sheet – global harms and policy measures
Citations above are provided for context and patient education. For diagnosis and treatment, a direct clinical evaluation is essential.
Conclusion
Alcohol problems progress in patterns, yet recovery is possible. Key takeaways: know early signs & risks, use simple screens, and don’t stop suddenly if dependence is likely, seek medical help.
Frequently Asked Questions (FAQs)
What Are the Stages of Alcoholism, and How Do They Usually Progress?
The stages of alcoholism are commonly described as early, middle, and late, moving from risky or heavy drinking to alcohol dependence.
In the early stage, rising tolerance and drinking to cope with stress show up. The middle stage brings loss of control, failed cut‑downs, blackouts, sleep problems, and growing impact at home and work.
The late stage involves physical dependence, withdrawal symptoms, and medical harm such as liver or pancreatic issues.
While the stages of alcoholism suggest a pattern, people can move forward or backward; remission is possible with care.
Which Early Signs in the Stages of Alcoholism Should Families Watch For?
In the early stages of alcoholism, watch for drinking more to feel the same effect (tolerance), using alcohol to unwind after stress, hiding or minimizing use, and memory gaps after drinking.
Mood swings, missed duties, and changing friend groups can follow if someone is in later stages of alcoholism, morning drinking, tremors, or needing a “relief” drink point to dependence.
These signs do not mean someone is “bad” or weak; they reflect changes in the brain & body that deserve medical attention.
Is it Safe to Quit Suddenly in the Later Stages of Alcoholism?
In the later stages of alcoholism, stopping suddenly can be unsafe. People who are physically dependent risk severe withdrawal, including seizures or delirium tremens.
Warning signs include shakes, sweating, fast pulse, nausea, anxiety, or confusion after cutting back. If dependence is likely, do not stop cold turkey; it can be dangerous, even life‑threatening.
Medical detox and close monitoring reduce risks and improve comfort during any stage of alcoholism.
Which Treatments Work Best at Different Stages of Alcoholism?
Treatment should match the stages of alcoholism. Early stage: brief counseling, motivational interviewing, and practical change plans may be enough.
Middle stage: structured therapy such as cognitive behavioral therapy, contingency management, family involvement, and medications like naltrexone or acamprosate.
Late stage: medically supervised detox first, then ongoing therapy, medication management, mental health care, and recovery support.
Across all stages of alcoholism, a personalized plan and steady follow‑up help maintain gains and prevent relapse.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts