Narcan, the brand name for naloxone, quickly reverses opioid overdoses, including those involving fentanyl, by restoring breathing. It is safe, has few risks, and is now sold over the counter in New Jersey pharmacies. This article explains when to use it, how to give it, and what to do next to protect health and recovery.
Key Takeaways
- Narcan (naloxone) quickly reverses opioid overdose by restoring breathing; it works on fentanyl, is safe in pregnancy and for youth; no effect if opioids aren’t present.
- Act fast: call 911 & give the 4 mg nasal spray right away; repeat every 2–3 minutes if no response; stay with the person, monitor for at least 2 hours.
- Signs to watch: unresponsive, slow or no breathing, bluish lips or nails, pinpoint pupils; New Jersey’s Good Samaritan protections support those who call for help.
- Safety and limits: effects last 30–90 minutes, withdrawal can happen (nausea, vomiting, agitation); store at room temp, check dates, but use what you have in an emergency.
What is Narcan?
Narcan is the brand name for naloxone, a fast-acting opioid antagonist that can rapidly reverse an opioid overdose, including overdoses involving fentanyl. It works by displacing opioids from the brain’s mu-opioid receptors. This blocks opioids from depressing the respiratory center, which allows breathing to return. When used quickly and correctly, Narcan can restore breathing in about 2–3 minutes.
Narcan’s effect is temporary. The reversal usually lasts 30–90 minutes. Because many opioids, especially fentanyl and long-acting medications, can last longer than naloxone, repeat doses may be required, and medical follow-up is important.
Narcan is safe to use during pregnancy and in children. If opioids are not present, Narcan does not cause intoxication or dependence. It simply has no pharmacologic effect. This is why public health authorities encourage lay responders to carry and use Narcan when an overdose is suspected. The risk of harm from giving Narcan unnecessarily is very low, while the potential benefit is life-saving.
Rolling Hills Recovery Center supports broad naloxone access across New Jersey as part of a comprehensive response to the overdose crisis. Narcan is a bridge back to breathing, and often, to care.
Core Facts to Keep in Mind
- Narcan reverses life-threatening respiratory depression from opioids by displacing them from receptors.
- Onset is about 2–3 minutes after nasal spray; effects last 30–90 minutes.
- It’s safe for pregnant people and for children. No effect if opioids aren’t present.
- Multiple doses may be needed with potent opioids like fentanyl or with contaminated drug supplies.
- Always call 911; Narcan is not a substitute for medical care.
When to Use Narcan and What to Look For
Opioid overdose is primarily a breathing emergency. Oxygen deprivation causes brain injury and death within minutes, so recognizing the signs and acting immediately is critical.
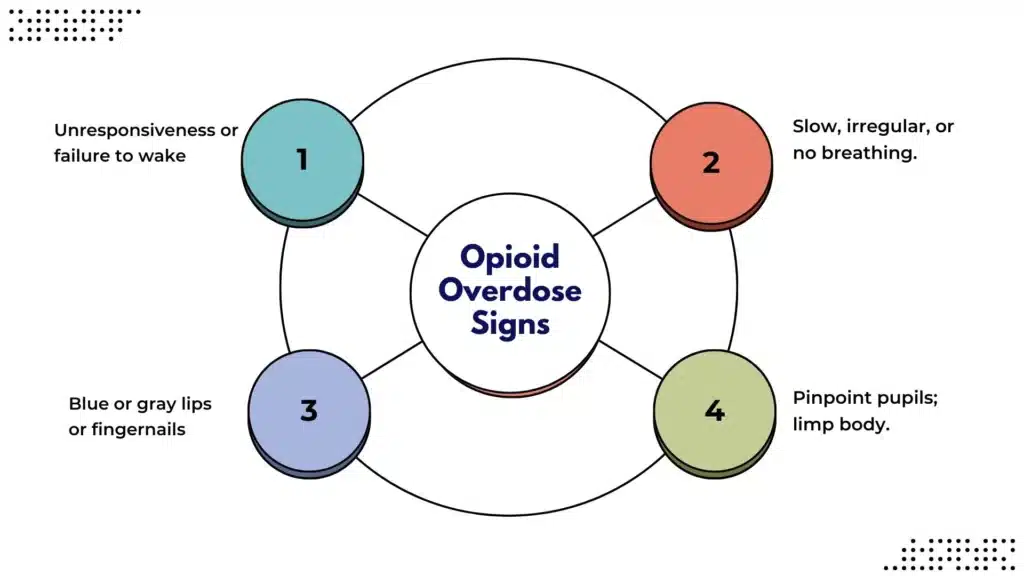
Common overdose signs and when to use Narcan:
- Unresponsiveness: cannot be woken with shouting or a firm sternum rub.
- Slow, irregular, or no breathing: fewer than 8 breaths per minute, snoring or gurgling, long pauses.
- Blue or gray lips or fingernails; cool, clammy skin.
- Pinpoint pupils; limp body; vomiting; very pale or ashen face.
If any of the signs above are present and an opioid overdose is possible, even if other drugs are involved, give Narcan.
Immediate Steps: Call, Support Breathing, Give Narcan, Repeat if Needed
- Call 911 first. Say there is an unresponsive person not breathing normally. In New Jersey, Good Samaritan protections generally shield callers and overdose victims from certain charges when seeking help in good faith.
- Position the person on their back. If there is a lot of vomiting, roll onto their side to keep the airway clear.
- Clear the airway. Remove obvious obstructions. If trained, start rescue breathing (details below). If there is no pulse and you’re trained, begin CPR.
- Administer Narcan nasal spray (4 mg) into one nostril. See the precise steps in the section below.
- Monitor and support breathing. If there is no response in 2–3 minutes, give a second dose in the other nostril.
- Keep repeating every 2–3 minutes if there is no response or if breathing slows again. Stay with the person until EMS arrives.
- When the person starts breathing and waking up, place them on their side (recovery position) to prevent choking.
Rolling Hills Recovery Center sees many families who acted fast with Narcan and saved a life. Quick action matters.
Forms, Dosing and How to Administer
Naloxone comes in several forms. The over-the-counter (OTC) 4 mg nasal spray (Narcan) is the most common for community use because it is simple, compact, and requires no needles.

Over-the-Counter 4 mg Nasal Spray: Peel, Place, Press
Nasal spray is designed for use by non-medical responders. One device equals one dose. No priming, no assembly, no measuring.
Step-by-step administration:
- Peel: Remove the device from the blister pack. Hold it with your thumb on the bottom of the plunger and two fingers on the nozzle.
- Place: Tilt the head back. Support the neck. Gently insert the nozzle into one nostril until your fingers touch the nose.
- Press: Press the plunger firmly to release the full dose. The spray is atomized; it absorbs through the nasal mucosa.
After the first dose:
- Watch for breathing to improve within 2–3 minutes.
- If no response or if breathing remains shallow/slow, give a second dose in the other nostril.
- Continue rescue breathing if needed. Keep EMS on the way.
- Expect the person to be drowsy as they wake. Protect their airway and keep them on their side if vomiting occurs.
Storage and practical tips:
- Store at room temperature; avoid extreme heat or freezing. Keep out of direct sunlight.
- Check expiration dates periodically. However, if all you have is an expired unit during a suspected overdose, use it; some potency may remain, and there’s no known harm from trying.
- Do not delay administration due to fear of “doing it wrong.” The device is designed to be simple. Time is critical.
- Keep two or more doses with you; fentanyl-contaminated supplies can require multiple doses.
Intramuscular Vials and Auto-Injectors
Naloxone is also available in injectable forms. These are useful in clinical settings or programs with training. Auto-injectors were designed for lay use, though availability can vary over time.
Comparison of common forms:
| Form | Typical community dose | How it’s given | Ease of use | Where found |
|---|---|---|---|---|
| OTC nasal spray (Narcan) | 4 mg per spray (1 device) | Spray into one nostril; repeat every 2–3 minutes if needed | Easiest; no assembly | Pharmacies OTC; community programs |
| Intramuscular (IM) vial | Inject into the outer thigh; voice prompts on some devices | Draw into syringe, inject into thigh or shoulder | Requires training and supplies | Clinics, harm reduction programs |
| Pre-filled syringe or auto-injector | Doses vary by product | Simple, but product availability varies | Simple but product availability varies | Select programs; availability changes |
For IM administration:
- Use a clean syringe and needle if available.
- Inject into the large muscle of the thigh (through clothing if necessary).
- Dose can be repeated every 2–3 minutes, similar to a nasal spray, until breathing improves.
Because nasal spray is painless to use and widely accessible, it remains the first choice for most families and bystanders.
Safety, Side Effects, and Limits
Naloxone has a strong safety profile. It has been used in hospitals for decades, for adults, children, and during pregnancy.
Possible side effects:
- Short-lived withdrawal symptoms in people who use opioids regularly. Nausea, vomiting, sweating, gooseflesh, agitation, body aches, anxiety. These are uncomfortable but not life-threatening.
- Rare reactions: elevated blood pressure or fast heart rate; typically self-limited.
Important limits:
- Narcan treats opioid overdose only. It will not reverse overdoses from non-opioid drugs like benzodiazepines or xylazine. However, many overdoses involve multiple substances, and opioids often drive the breathing problem. Give Narcan anyway and support breathing.
- With potent opioids (fentanyl and analogs), more than one dose may be needed. If breathing improves and then slows again, repeat dosing.
- Xylazine, a non-opioid sedative appearing in the drug supply, will not respond to naloxone. Still give Narcan because opioids may be present, and give sustained rescue breathing until EMS arrives.
- Narcan is not a substitute for full medical care. The person can fall back into overdose after naloxone wears off. Monitor for at least 2 hours, longer if long-acting opioids are suspected.
Airway and breathing always come first. Even when Narcan works, continue to watch the person’s breathing. If they were using a long-acting opioid, or if the supply is unknown, consider that effects can recur after 30–90 minutes.
How to Provide Rescue Breathing and Basic CPR Support
If the person is not breathing or is breathing poorly, ventilation is crucial. It can be done with or without airway equipment.
Rescue breathing basics:
- Place the person on their back; tilt the head back and lift the chin.
- Pinch the nose shut; give one breath into the mouth every 5–6 seconds, enough to see the chest rise.
- If a face shield is available, use it. If not, you can still give breaths; this is a respiratory emergency.
- If there is no pulse and you’re trained, begin chest compressions at a rate of 100–120 per minute, depth 2 inches for adults. Alternate 30 compressions with 2 breaths.
Reassess every 2–3 minutes. Give additional Narcan if there is no improvement in breathing or if breathing worsens. Continue until EMS arrives.
Access in New Jersey, Cost and Training
New Jersey has expanded access to naloxone through multiple channels. Narcan 4 mg nasal spray is FDA-approved for over-the-counter purchase and is stocked by many pharmacies statewide. Most retailers can sell it without a prescription, and some offer it behind the pharmacy counter to answer usage questions.
Prices vary by brand and pharmacy; consumers can use discount cards or manufacturer coupons. Some insurers reimburse OTC naloxone, though coverage policies differ. Community-based organizations and health departments often host free distribution events.
The New Jersey Naloxone365 initiative increases year-round access. Many participating pharmacies and community partners can provide no-cost naloxone or facilitate training.
Additional access and training considerations:
- Pharmacies: Ask for OTC Narcan 4 mg nasal spray; most chains and many independent pharmacies stock it. If it is out of stock, request next-day ordering.
- Community programs: Harm reduction centers, local health departments, and certain EMS or fire departments may offer no-cost naloxone and training.
- Workplaces, schools, and housing: Encourage adding naloxone to AED and first-aid kits. Many organizations now include naloxone in emergency response plans.
Rolling Hills Recovery Center encourages families affected by substance use to carry naloxone. For people at increased risk, such as those who have recently detoxed or been released from jail, mixing opioids with benzodiazepines or alcohol, using alone, or using powders/pills from informal sources, having Narcan on hand can prevent a tragedy.
After a Reversal: What to Do Next
Returning to breathing is the first win. The next step is stabilizing health and pursuing care that reduces the risk of another overdose. Evidence-based care for opioid use disorder includes medications and wraparound support.
Effective medications for opioid use disorder (MOUD):
- Buprenorphine: partial opioid agonist that reduces cravings and withdrawal, lowers overdose risk, and can be started quickly, even the same day.
- Methadone: full agonist in a structured program; highly effective for those with long histories of opioid dependence.
- Extended-release naltrexone: an opioid antagonist that can help prevent relapse after a period of abstinence.
Rolling Hills Recovery Center provides individualized care plans and integrates medical and behavioral therapies with holistic supports. Therapy for co-occurring conditions, family services, and relapse prevention planning all play a role. No single path works for everyone, and care should be tailored.
New Jersey’s drug supply has become unpredictable, with counterfeit pills and non-opioid adulterants. People who do not meet stereotypes, such as students, professionals, and older adults, can be affected; some may hide their use or appear “functional” to others. For perspective on hidden or high-functioning patterns, see this resource on what is a functional addict.
If you or a loved one needs a refresher on the difference between misuse, dependence, and addiction, review our article on what drug addiction is to better understand how medical teams approach care.
Harm Reduction Supports to Add Alongside Narcan
- Fentanyl test strips and, where available, xylazine test strips can offer limited risk checks before use. Not perfect, but helpful data.
- Never use alone if possible. Consider virtual spotting services or a trusted partner who holds naloxone.
- Avoid mixing opioids with alcohol, benzodiazepines, or gabapentinoids. The combination magnifies breathing risks.
- After any non-fatal overdose, prioritize same-day access to MOUD. The risk of another overdose is highest in the days that follow.
Special Situations
Pregnancy and Postpartum
Naloxone can be safely administered during pregnancy in suspected overdose. The primary threat is maternal hypoxia; restoring oxygenation helps both parent and fetus. EMS should evaluate promptly. If the pregnant person is on medication for opioid use disorder, coordinate care to minimize withdrawal risks while ensuring safety.
Children and Adolescents
Accidental exposures in children require immediate action. Use the same steps: call 911, support breathing, administer Narcan. Pediatric naloxone dosing is safe; with the nasal spray, the standard device is appropriate. Report exposures to poison control after EMS is engaged.
Older Adults and People on Prescription Opioids
Patients on opioid pain medications, especially when combined with sedatives or sleep aids, benefit from at-home naloxone. Clinicians routinely co-prescribe naloxone for higher-risk prescriptions. Families should store it with other emergency items and review how to use it. Teach caregivers the peel–place–press steps.
Xylazine and Evolving Drug Supply
Xylazine is a veterinary sedative appearing in the illicit supply. It is not an opioid, so naloxone will not reverse xylazine sedation. However, opioids are commonly co-present. The recommended response remains the same: give Narcan, provide rescue breathing, and seek medical care. Wounds related to xylazine require professional attention; delaying wound care increases infection risk.
Practical Planning: A Simple Overdose Response Card
It helps to keep a short, written checklist with each naloxone kit. A wallet-sized card or a phone note works:
- Check responsiveness → no response, slow/abnormal breathing.
- Call 911; describe breathing problem, give location.
- Tilt head; clear airway; give 1st Narcan dose in one nostril.
- If not breathing, give rescue breaths every 5–6 seconds.
- Reassess at 2–3 minutes → repeat Narcan in other nostril if needed.
- Recovery position when breathing returns; stay until EMS arrives.
This can be printed and taped to the inside of a Narcan box. Families often learn best by practice; consider a short role-play with housemates so everyone knows their role.
Storage, Replacement, and Kit Readiness
Keep naloxone where it’s accessible, near the front door, in a backpack, or with other emergency items. Avoid leaving it in cars where heat and cold can degrade it. Replace it before the expiration date when possible, and attach a sticky note on the box with the date for easy tracking. If the spray seems cloudy or the device is cracked, get a new box.
Add simple tools to your kit:
- A face shield for rescue breathing.
- A pair of gloves.
- A small reminder card with the steps and the address of your location (helpful in a crisis).
These are not required to save a life, but can make the response smoother.
Common Myths and Plain Facts
Myth: Narcan encourages drug use.
Fact: Research does not support this claim. Naloxone access programs reduce deaths and do not increase substance use. People who survive an overdose are more likely to enter treatment afterward, especially when navigators connect them directly to care.
Myth: Giving Narcan can kill someone who “only” used stimulants.
Fact: If opioids are not present, naloxone does not cause overdose. It will have no effect. Many stimulant supplies now contain fentanyl, so it is safer to give Narcan when in doubt.
Myth: One dose always fixes it.
Fact: Not always. Potent or long-acting opioids and mixed-substance overdoses can outlast naloxone. Be ready to administer repeated doses every 2–3 minutes until breathing is normal and EMS arrives.
Myth: Laypeople can’t do this safely.
Fact: The nasal spray was developed so non-medical helpers can respond fast. Training improves confidence, but the device is intuitive. Peel, place, press.
Documentation and Reporting After an Overdose
If feasible, note what substances might have been used and at what time, along with how many naloxone doses were given. Hand this information to EMS. If syringes or paraphernalia are present, leave them for responders to handle safely; do not place yourself at risk for needle injuries.
Some programs ask lay responders to submit anonymous reports of naloxone use to track community impact. This helps public health and improves the allocation of resources. Participation is optional, but valuable.
Legal Considerations: New Jersey Good Samaritan Protections
New Jersey law offers Good Samaritan protections for people who, in good faith, call for help during an overdose. The intent is to remove the fear of arrest for simple possession or use when someone seeks medical aid. Do not leave the scene; stay with the person until help arrives if it is safe to do so. This legal protection aims to prioritize saving lives.
Many workplaces and schools also have policies that allow staff to use naloxone in emergencies, similar to AEDs and EpiPens. Ask administrators to include naloxone in emergency drills and ensure the devices are not locked away.
Training Opportunities and Helpful Resources
Even brief training increases confidence and response speed. Rolling Hills Recovery Center encourages families to take a 10–15 minute naloxone overview from a pharmacist or community trainer. More in-depth courses often include hands-on practice with trainer devices.
Trusted resources:
- FDA naloxone overview: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/information-about-naloxone-and-nalmefene
- CDC naloxone facts: https://www.cdc.gov/overdose-prevention/media/pdfs/2024/04/Naloxone-Fact-Sheet_FamilyandCaregivers_HowandWhen_4_11_2024.pdf
- NIDA naloxone DrugFacts: https://nida.nih.gov/publications/drugfacts/naloxone
- New Jersey Naloxone365: https://nj.gov/humanservices/resources/Naloxone365_OnePager_v1.pdf
These sources are updated regularly and reflect current best practices.
How Narcan Fits Into Comprehensive Care at Rolling Hills Recovery Center
Naloxone is immediate life support. It does not treat the underlying medical condition, opioid use disorder, or other substance problems, but it creates the opportunity to engage. Rolling Hills Recovery Center provides evidence-based opioid and fentanyl addiction treatment backed by medical and behavioral teams. Treatment plans often include:
- Rapid access to MOUD (buprenorphine, methadone coordination, or naltrexone).
- Therapy focused on relapse prevention, trauma, and coping skills.
- Family involvement when appropriate, because support at home affects outcomes.
- Holistic modalities, such as mindfulness and exercise plans, help stabilize sleep, mood, and stress.
- Discharge planning with naloxone-on-hand, overdose education, and linkage to community supports.
People recover on different timelines. Setbacks happen. It is vital to ensure that Narcan is available throughout treatment and during transitions, such as after detox or residential care. The risk of overdose is higher after periods of reduced tolerance. Comprehensive planning reduces that risk.
Final Reminders That Save Lives
- When in doubt, give Narcan; it will not cause harm if opioids are absent.
- Breathing support is as important as the medication. Rescue breaths can be the difference while Narcan takes effect.
- Re-dose every 2–3 minutes if no response or if breathing worsens again.
- Stay with the person. Overdose can return as naloxone wears off.
- Keep Narcan accessible and check the expiration date, but use any available product in an emergency.
Narcan makes community members first responders in the most important way, restoring breath. Rolling Hills Recovery Center continues to partner with individuals and families across New Jersey to build safer plans, expand access to naloxone, and connect those at risk with proven care.
Conclusion
Narcan saves lives by restoring breathing fast; the key is to recognize overdose signs & act. Call 911, give the nasal spray, repeat if needed, then monitor… Keep a kit on hand and teach the family.
Frequently Asked Practical Questions
What if the Person Becomes Agitated After Narcan?
This can occur because of sudden opioid withdrawal. Keep the environment calm. Explain that they were not breathing and that EMS is on the way. If the person wants to leave, encourage them to at least wait for a few minutes of monitoring. Safety first, for them and for you.
Can Narcan Be Used on Pets?
Naloxone is used in veterinary settings for opioid toxicity, but community responders should prioritize human emergencies and follow veterinary guidance for animals. Consult a veterinarian for pet exposures.
What if the Nasal Spray Seems Clogged?
The device is single-use and sealed. There is no priming. If a dose appears ineffective and you suspect device failure, use another device immediately.
Should I Keep Narcan if No One in My Home Uses Opioids?
Yes. Accidental exposures, counterfeit pills, and community overdose events happen. Carrying Narcan is similar to having a fire extinguisher, a basic safety step.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












