Fentanyl-laced drugs are driving unexpected overdoses across New Jersey. From counterfeit pills to contaminated powders, trace amounts can shut down breathing within minutes. This article explains risks, how to spot warning signs, when to use naloxone, and what evidence-based treatment looks like, drawing on clinical experience to keep individuals and families safer and supported.
Key Takeaways
- Illicit fentanyl shows up in heroin, cocaine, meth, and fake pills across NJ; it’s ultra‑potent, a few grains can stop breathing, and you can’t see or taste it.
- Lower risk: test with fentanyl test strips, don’t use alone, start low, go slow, avoid mixing opioids with benzos & alcohol, and carry naloxone at all times.
- Overdose response: watch for slow or no breathing, blue lips, gurgling; call 911 immediately (NJ Good Samaritan applies), give naloxone, rescue breathing or compressions, repeat doses every 2–3 minutes until EMS arrives.
- Prevention in NJ: pharmacies and community programs offer naloxone, secure meds at home, avoid pills from social media, use take‑back sites; keep an eye on state health alerts… simple steps save lives.
Fentanyl Laced Drugs: Scope and Why it Matters
What “Laced” Means in Day-to-Day Use
“Laced” means a drug has been mixed, intentionally or accidentally, with an additional substance. In this context, fentanyl is added to or contaminates other drugs: heroin, counterfeit pain pills, pressed benzodiazepine‑lookalikes, cocaine, methamphetamine, and “party powders.” The fentanyl that shows up in these supplies is usually illicitly manufactured fentanyl (IMF), not the medically prescribed version used in hospitals.
Dealers and illicit manufacturers may add fentanyl to increase potency or to make counterfeit pills that mimic prescription tablets. Others may contaminate products through shared surfaces or equipment. For people who have not built opioid tolerance or aren’t expecting an opioid at all, this creates a high risk of sudden overdose.
No new local New Jersey data were found in the earlier search summary; the discussion here relies on national public health alerts and warning trends from the CDC and DEA. Those advisories continue to stress the widespread presence of fentanyl in non-opioid drug supplies and counterfeit pills.
How Fentanyl Ends Up in Heroin, Powders, and Counterfeit Pills

- Heroin: IMF is often substituted for or mixed into heroin because it is cheaper to produce and easier to transport in small volumes.
- Stimulants (cocaine, meth): Cross-contamination during handling, cost-cutting, or intentional “speedballing” effects can leave stimulant users exposed to fentanyl unknowingly.
- Counterfeit pills: Blue “M30” tablets that appear to be oxycodone 30 mg are frequently pressed with fentanyl. So are fake alprazolam (Xanax) or hydrocodone pills. The pill may look legitimate, imprints, color, and shape aren’t reliable.
Why the Potency and Inconsistent Mixing Are so Dangerous
Fentanyl is about 50 times stronger than morphine and many times stronger than heroin. Microgram-level amounts can be deadly. The illicit supply is not uniform; mixing can be uneven, creating “hot spots” in powders or pills where the fentanyl dose is much higher.
A user can take the “same” amount from one bag or pill and be fine one day, and then overdose the next from a different part of the same product. This is the core reason the overdose risk has surged, and why harm reduction practices and prompt access to naloxone are vital.
Rolling Hills Recovery Center treats the behavioral consequences of fentanyl exposure daily. Clinicians see that a person’s intent, perhaps to use only a prescription-looking pill, doesn’t reliably match what’s in the supply. That mismatch drives the need for practical, step-by-step safety skills alongside treatment options.
Risks, Detection, and Safer-Use Basics
Visual Checks Don’t Work; Assume Fentanyl is Present
Fentanyl has no distinct taste, smell, or look when mixed in typical street supplies. Visual inspection is not a screening method. Counterfeit pills can look professional, and powders can appear uniform even when they aren’t. Assume potential fentanyl exposure in any non-prescribed pill or powder.
A few grains of fentanyl powder can be lethal. People without opioid tolerance face the highest risk, but even high-tolerance users can overdose when batches vary.
Common Signals in the Current Supply
- Counterfeit “M30” oxycodone‑lookalike pills are common nationally.
- Party powders at clubs, festivals, and house parties can be contaminated.
- Pressed benzodiazepine‑lookalikes sometimes contain fentanyl or other unexpected sedatives.
How to Use Fentanyl Test Strips (FTS) Correctly
Fentanyl test strips can detect fentanyl and some fentanyl analogs in a dissolved sample. They do not show dose, and they can miss hot spots if the small sample tested doesn’t contain the fentanyl particles present elsewhere. However, they’re a practical tool when used carefully.
- Dissolve a tiny sample: Place a small amount of the drug (or scrape from a pill) into clean water; more water improves detection for many strips. Stir or swirl until dissolved.
- Dip the strip: Submerge the test end to the indicated line for the time listed in the kit directions (commonly about 10–15 seconds). Remove and lay flat.
- Wait and read: Wait the instructed time (often 1–2 minutes). Follow the specific kit’s directions for “positive” versus “negative” lines.
- Retest if unclear: If the result is faint, contaminated, or uncertain, mix a fresh sample and test again. Treat unclear results as “cannot rule out fentanyl.”
- If positive: You can discard the product, use less, add a trusted person who has naloxone, and avoid mixing with depressants. Remember, a negative does not guarantee safety.
Important: FTS detects presence, not quantity. Fentanyl can still be in a portion you didn’t test.
Safer-Use Basics That Save Lives
- Don’t use alone. If using, have someone nearby who can check breathing. Consider phone check-ins or overdose monitoring hotlines.
- Start low, go slow. Use a smaller test dose and wait; treat every new batch as unknown.
- Avoid mixing fentanyl with benzodiazepines, alcohol, or other sedatives. This combination multiplies breathing suppression.
- Always carry naloxone. Nasal naloxone is easy to use. Teach friends and family where it is and how to use it.
- Plan your setting. Keep phones charged, naloxone visible, and a person ready to call 911.
Rolling Hills Recovery Center encourages anyone who’s noticed rising tolerance, withdrawal, or near-overdose events to consider a structured step toward stability, including medical detox for fentanyl when needed.
Overdose Signs and Response
What to Look for Right Away
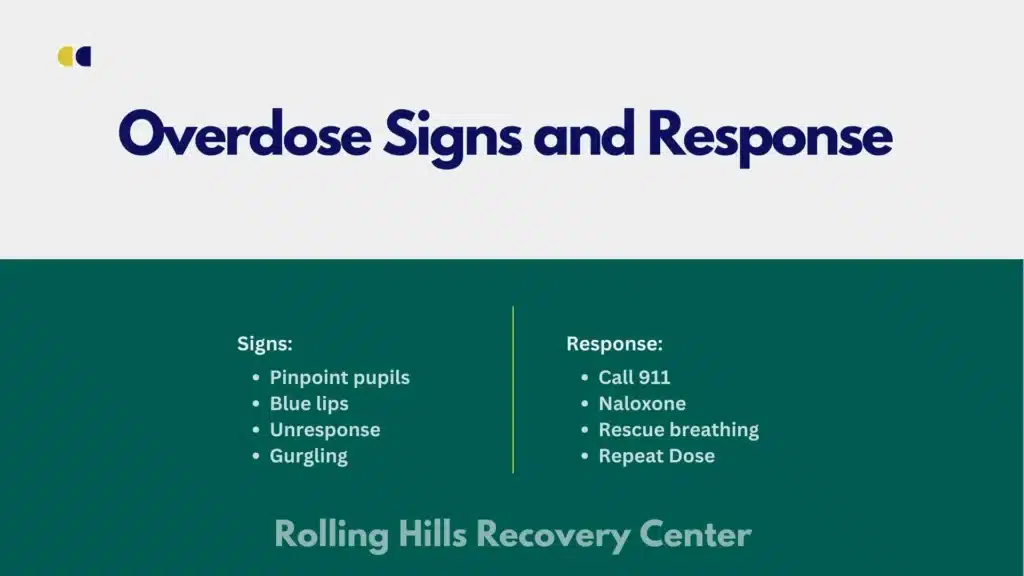
Fentanyl overdose typically slows or stops breathing. With fentanyl, the onset can be fast. Key signs:
- Pinpoint pupils
- Slowed or no breathing; shallow breaths; snoring or gurgling sounds
- Blue or gray lips and fingertips (cyanosis)
- Unresponsiveness; can’t be woken by shouting or sternal rub
- Limp body; pale, clammy skin
- Slow or faint pulse, or no pulse
In New Jersey, the Overdose Prevention Act (Good Samaritan law) provides protections for people who call for help in a suspected overdose. Don’t delay the call.
Step-by-Step Response That Works
- Call 911 immediately: Say, “Someone isn’t breathing; possible overdose; need naloxone.” Put the phone on speaker.
- Give naloxone fast: If you have a nasal spray, insert it into one nostril and depress the plunger. If you have injectable naloxone, follow the kit’s instructions. Time matters.
- Assess breathing and support it:
- If the person is not breathing or barely breathing, begin rescue breathing: tilt the head back, lift the chin, pinch the nose, give one breath every 5–6 seconds, watching for the chest to rise.
- If you cannot give rescue breaths and there’s no pulse, begin chest compressions at a rate of 100–120 per minute.
- Place in recovery position when breathing returns: Turn on side with top knee bent to prevent choking if vomiting occurs.
- Repeat naloxone every 2–3 minutes if needed: If there’s no response or breathing slows again, give an additional dose. Fentanyl can outlast naloxone’s effect.
- Stay until help arrives: Monitor breathing. Share what was taken if known. EMS can provide oxygen and longer-acting care.
Naloxone is safe to give even if the person did not use opioids; when in doubt, give it. Withdrawal symptoms after naloxone are uncomfortable but not life-threatening compared to an untreated overdose.
NJ-Focused Prevention and Access
Are Fentanyl Test Strips Allowed in New Jersey?
Yes. New Jersey allows fentanyl test strips and treats them as harm-reduction supplies. They are available through NJ Department of Health harm reduction programs and many community partners statewide. This improves access without paraphernalia concerns.

Where to Get Naloxone and How to Use Statewide Programs
- Pharmacies: New Jersey has a statewide standing order. Naloxone can be obtained without an individual prescription. The Naloxone365 initiative offers free naloxone at participating pharmacies. Ask your local pharmacy about availability.
- Community programs: Harm reduction centers and local health departments often distribute naloxone kits and provide brief training. Many provide anonymous pickup.
- Training: Quick training is available both in-person and online; practice with a demo device if possible.
Family and Community Steps That Reduce Risk
- Store medications safely: Lock up opioid pain medicines; count pills; never share prescriptions.
- Talk with adolescents and college-age adults: Explain that counterfeit pills sold on social media or by friends are not safe. One pill can contain a lethal dose.
- Be careful with social media pill sales: Counterfeit pills are common; avoid buying or taking any non-prescribed pill.
- Dispose of unknown or unused pills: Use DEA prescription take-back events or permanent drop boxes at pharmacies and police stations. Don’t flush.
- Track local advisories: Follow the NJ Department of Health and your county health department for alerts about contaminated supplies or spikes in overdoses.
- Practical NJ checklist:
- Confirm your household has at least two naloxone doses and everyone knows where they are.
- Pick up fentanyl test strips and know how to use them.
- Save 911 and your local health department’s overdose alert pages to your phone.
- If someone uses opioids, set up a check-in plan and keep naloxone in multiple places.
Rolling Hills Recovery Center integrates harm reduction into care planning. The team encourages families to carry naloxone, learn FTS use, and practice a home safety plan, whether a loved one is ready for treatment today or still on the fence.
Treatment and Recovery Essentials
Why Early Medical Evaluation Matters After Suspected Exposure
Even if an overdose is reversed, fentanyl can linger. People may experience re‑sedation after naloxone wears off. A medical evaluation helps rule out complications like aspiration, hypoxia, or co-ingestant effects. Early contact with a fentanyl treatment professional also opens the door to stabilization options that reduce the chance of another overdose.
Medications for Opioid Use Disorder (MOUD)
- Buprenorphine: A partial opioid agonist that reduces cravings and fentanyl withdrawal symptoms, with a safety ceiling that lowers overdose risk. It can be started in outpatient settings, often the same day. Buprenorphine/naloxone combinations are common.
- Methadone: A full opioid agonist provided at specialized clinics. Highly effective for people who need more structure or do better on a long-acting medication with daily check-ins.
- Naltrexone (extended-release): A monthly opioid antagonist injection for individuals who have fully detoxed from opioids and want a non-opioid option. It blocks opioid effects and can help prevent return to use, though it requires careful timing and preparation.
Whole-Person Care and Co-Occurring Mental Health Needs
Anxiety, depression, PTSD, and sleep disorders often co-occur with opioid use. Treating both at once improves outcomes. Care plans typically include:
- Evidence-based therapies (CBT, DBT-informed skills, trauma-focused approaches).
- Psychiatric evaluation with medication management when indicated.
- Sleep and nutrition support, because physiology affects cravings and mood.
- Skills for distress tolerance and trigger management.
Family Education and Involvement
Families benefit from coaching on:
- Overdose prevention at home (naloxone, FTS, safe storage).
- Communication that reduces shame and escalations.
- Boundaries that promote safety while keeping doors open.
- Understanding medications for opioid use disorder and how they work.
Rolling Hills provides structured family sessions to align expectations and reduce friction. If a loved one is ambivalent about change, share supportive resources, like when drugs and alcohol feel unmanageable, or this piece for those who want to stop using but can’t. These give language for tough conversations and describe next steps without pressure.
Relapse Prevention, Aftercare, and Harm Reduction Integration
Relapse prevention planning is specific, not generic. It includes:
- A written crisis plan: warning signs, people to call, steps to take, and a location list (urgent care, EDs, pharmacies with naloxone).
- Medication continuity: scheduled follow-ups, refills, and backup plans if a dose is missed.
- Skill practice: coping strategies for high-risk times of day, places, and social triggers.
- Contingency plans: what to do if return to use happens, carry naloxone, don’t use alone, and return to care promptly.
Harm reduction is not at odds with recovery. It keeps people alive while they progress. Many Rolling Hills clients start with stabilization goals and shift toward abstinence as health and stability return.
Practical Tools and Simple Templates That Help
- Overdose safety card: Keep a small card in a wallet listing naloxone location, dosing steps, and emergency contacts.
- Check-in text template: “Checking in. Are you okay? Reply within 5 minutes, or I’ll come by/call 911.”
- Pill/powder testing routine: A brief, repeatable checklist for FTS steps and dose sizing (start low, wait, reassess).
- Appointment anchors: Add recurring reminders for medication pick-ups and therapy sessions; share calendar invites with your support person.
Useful Resources to Cite and Read
- CDC: Fentanyl facts and overdose prevention: the national snapshot of risks, signs, and response.
- DEA: One Pill Can Kill: counterfeit pill warnings and visuals of common fakes.
- NIDA: Fentanyl: science, epidemiology, and links to current research
- SAMHSA: Naloxone and overdose response: training videos and state resources.
- NJ Department of Health: Harm reduction: locations for services, naloxone programming, and updates.
- Consider bookmarking local county health department pages for real-time advisories.
- How to use this list:
- Save links on your phone for quick reference.
- Share the naloxone training resource with at least two people in your circle.
- If you handle unknown pills or powders, review One Pill Can Kill visuals before you go out.
- Revisit NIDA pages monthly; recommendations and data get updated.
Conclusion
Fentanyl‑laced drugs are unpredictable, but prevention & quick action save lives. Focus on three steps: test first, carry naloxone, call 911 fast. Avoid mixing substances and learn overdose signs.
Frequently Asked Questions (FAQs)
What Are Fentanyl Laced Drugs, and Why Are They So Dangerous?
Fentanyl laced drugs are street pills or powders that have fentanyl mixed in, often without the person knowing. Because illicit fentanyl is extremely potent and not evenly mixed, a few grains can shut down breathing.
In New Jersey, fentanyl laced drugs have been found in heroin, cocaine, meth, and counterfeit pills that look like oxycodone “M30,” Xanax, or Adderall.
The combination of high potency and surprise exposure drives sudden overdoses.
How Can Someone Spot Fentanyl Laced Drugs Before Use?
There’s no reliable way to see, smell, or taste fentanyl in a product. Visual checks don’t work. The safer approach is to test and prepare. Fentanyl test strips can help: dissolve a tiny sample in water, dip the strip as directed, wait for a brief time, and read the result; retest if unsure.
Start low and go slow if someone still chooses to use. Don’t mix opioids with alcohol or benzodiazepines, avoid using alone, and carry naloxone. These steps reduce risk with fentanyl laced drugs, even if they don’t remove it.
What Are the Warning Signs of An Overdose From Fentanyl Laced Drugs, and What Should Be Done Right Away?
Key signs include slow or stopped breathing, bluish lips or nails, pinpoint pupils, gurgling or snoring sounds, and unresponsiveness. Act fast, call 911 immediately; New Jersey’s Good Samaritan protections apply.
Give naloxone if available, then provide rescue breathing if there’s no breathing, or chest compressions if no pulse. If there’s no response in 2–3 minutes, give another naloxone dose.
Stay with the person until EMS arrives; fentanyl laced drugs can outlast the first naloxone dose.
Are Fentanyl Laced Drugs Showing Up in Counterfeit Pills, and What Should Parents & College Students Know?
Yes. Counterfeit pills made to look like common medications are a major source of fentanyl laced drugs. Buying pills from social media or friends-of-friends is risky, contents are unknown.
Families and students should talk openly about this, store legitimate medications securely, dispose of unknown pills at take-back sites, keep naloxone on hand, and consider test strips.
On campus or at parties, never use alone and don’t mix substances; simple steps save lives.
How Does Rolling Hills Recovery Center Help People Affected by Fentanyl Laced Drugs?
Rolling Hills Recovery Center offers evidence-based addiction treatment and holistic approaches for individuals exposed to fentanyl laced drugs.
The team provides medical detox placement when needed, trauma-informed therapy, mental health care, family education, and relapse-prevention planning & aftercare.
Their experienced professionals focus on practical harm reduction during stabilization and on building lasting results through individualized treatment.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












