A private alcohol rehab clinic offers safe detox, structured therapy, and ongoing support under medical supervision. From initial assessment to aftercare, care plans are personalized, evidence-based, and confidential.
This overview explains what patients can expect, how admission works, and how outcomes are measured, reflecting New Jersey standards and the approach used at Rolling Hills Recovery Center.
Key Takeaways
- Check New Jersey licensing and trusted accreditation; ask for a board-certified addiction medicine doctor and a 24/7 safety plan.
- Intake should cover the whole person (ASAM areas), basic labs, and a clear detox plan if withdrawal risk is high.
- Care is evidence-based: therapies like CBT & motivational interviewing, plus medicines such as naltrexone or acamprosate when right.
- Privacy and costs matter; HIPAA-safe records, small caseloads, and honest billing are essential. Plan step-down care early (PHP, IOP) with relapse prevention.
What an Alcohol Rehab Private Clinic Covers: Scope of Care, Therapies, Mental Health, Family, and Privacy
Private alcohol rehabs in New Jersey are designed to deliver medical safety, discretion, and measurable progress. Rolling Hills Recovery Center combines evidence-based care with attentive service, small caseloads, and confidentiality that meets HIPAA standards.
Most private programs offer a full continuum, from medically supervised detox through outpatient services, so individuals move through the right level of care at the right time without breaks in treatment.
Levels of Care: From Detox to Outpatient
A private setting typically supports the following levels of care. Programs adjust intensity using standardized placement criteria such as the ASAM Criteria.
| Level of Care | Setting and Length | Clinical Focus | Best For |
|---|---|---|---|
| Medical Detox | Individual therapy, medication management, and recovery check-ins | Withdrawal stabilization, medications, hydration, nutritional support | Individuals at risk for moderate to severe withdrawal or with medical comorbidity |
| Inpatient/Residential | Live-in; 24-hour nursing; typically 14–30+ days | Step-down intensity, therapies, and medical monitoring without overnight stay | Those needing high structure, co-occurring stabilization, or repeated relapse |
| Partial Hospitalization (PHP) | Day program; 5–7 days/week; 6+ hours/day | Individual therapy, medication management, and recovery check-ins | Ready for community-based care but needing daily structure |
| Intensive Outpatient (IOP) | 3–5 days/week; 9–15 hours/week | Ongoing therapy, relapse prevention, life-skills, return-to-work planning | Transition from higher levels or as initial care for lower severity |
| Outpatient/Continuing Care | 1–3 hours/week | Individual therapy, medication management, recovery check-ins | Long-term maintenance and relapse prevention |
Rolling Hills Recovery Center offers medical detox placement and step-down treatment with evidence-based therapies, along with holistic supports, so care can be individualized across these levels.
Evidence-Based Therapies: CBT, MI, and Medication-Assisted Treatment
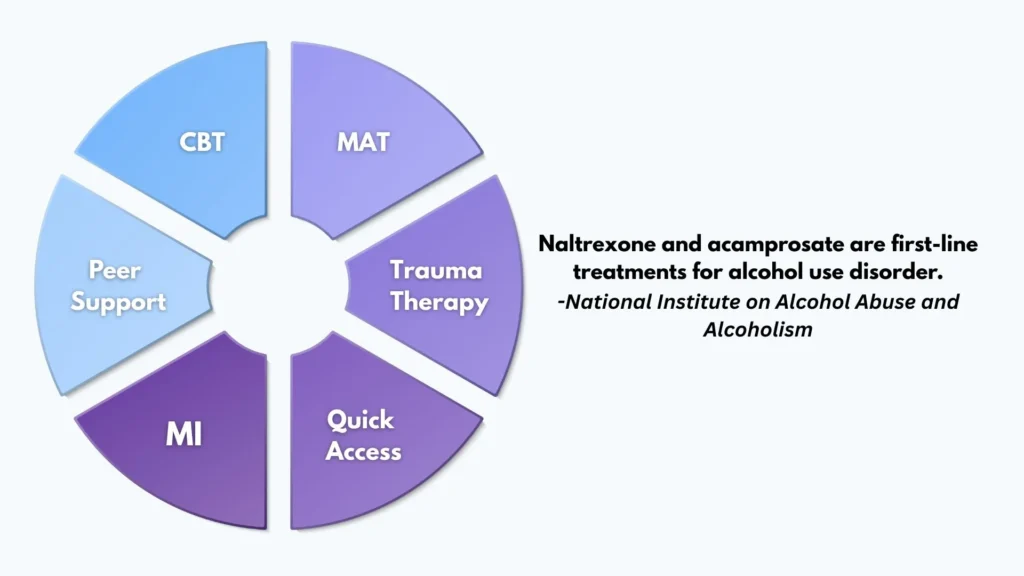
Private clinics emphasize approaches with strong research support:
- Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI): CBT helps patients identify triggers and reframe thinking patterns; MI strengthens internal motivation and commitment to change in a nonjudgmental way.
- Medication-assisted treatment for alcohol use disorder: Naltrexone (oral or extended-release injectable) reduces heavy drinking risk; acamprosate supports abstinence maintenance. Medication decisions follow a medical evaluation, liver function testing, and a discussion of goals, side effects, and contraindications. Disulfiram may be considered when close supervision is feasible and patient preference supports it.
- Skills training and relapse prevention: Cue exposure and coping strategies, drink refusal skills, sleep and stress management, and structured relapse prevention planning using personalized triggers and recovery supports.
- Education and self-assessment tools: Programs often incorporate resources such as the NIAAA’s “Rethinking Drinking” to help patients understand their drinking patterns, risks, and individualized changes.
Medication is integrated into a broader plan that includes therapy, social support, and health behavior change. When used, medication is monitored with scheduled follow-ups and lab checks when indicated.
Co-Occurring Mental Health Care
Alcohol use disorder often overlaps with depression, anxiety, PTSD, bipolar spectrum conditions, ADHD, sleep disorders, and trauma-related symptoms.
A private clinic should deliver integrated care: psychiatric evaluation, appropriate medication management (e.g., SSRIs for depression/anxiety when clinically indicated), psychotherapy tailored to co-occurring conditions, and safety planning.
Coordination between addiction medicine and psychiatry ensures medications are selected and titrated with the substance use picture in view.
Trauma-Informed Practices
Trauma-informed care is standard for private settings. Staff avoid re-traumatization by prioritizing:
- Emotional and physical safety
- Clear boundaries and consent for treatment activities
- Patient choice and collaboration
- Cultural humility and respect
- Evidence-based trauma therapies (e.g., trauma-focused CBT elements when appropriate)
Family Involvement and Aftercare Planning

Families are offered education on alcohol use disorder as a chronic, treatable health condition, with options for structured family sessions and boundary-setting.
Programs commonly include family systems work, communication skills, and recovery-support coaching. Before discharge, a written aftercare plan links the patient to:
- Medication follow-up with an addiction-informed prescriber
- Ongoing therapy or IOP
- Peer recovery support
- Primary care and mental health services
Privacy, Small Caseloads, and Concierge Coordination
Private clinics emphasize confidentiality and data security. Staff follow the HHS – HIPAA Summary, role-based access, and secure EHR practices. Small caseloads permit more individual work and faster adjustments to care plans.
Concierge-style coordination commonly includes appointment scheduling, transportation assistance, collaboration with employers when authorized, and discreet communication preferences.
In New Jersey, clinics should maintain state licensure and meet standards overseen by the Division of Mental Health and Addiction Services (DMHAS).
Patients or families can review NJ DMHAS – Licensing and Standards to verify standing and expectations.
Accreditation Expectations in New Jersey
While licensing is state-specific, high-quality private programs also seek national accreditation (e.g., The Joint Commission or CARF). Accreditation signals adherence to safety, clinical quality, and continuous improvement.
In New Jersey, programs should align staffing, medication practices, and data reporting with DMHAS requirements, and they should honor parity protections that ensure behavioral health benefits are comparable to medical/surgical benefits.
Clinical choices are always individualized, and safety comes first, particularly during withdrawal and early stabilization.
Programs also educate on public health frameworks, such as the CDC’s Alcohol and Public Health guidelines, which outline risk thresholds and health impacts to guide shared decision-making.
Admission, Assessment, and Stabilization

Private admission should be predictable and respectful, with clear next steps and transparent costs.
Step-by-Step: From Verification to First Dose
- Confirm licensing and accreditation
- Verify State of New Jersey licensure via NJ DMHAS – Licensing and Standards.
- Ask about national accreditation (The Joint Commission, CARF) and the most recent survey results.
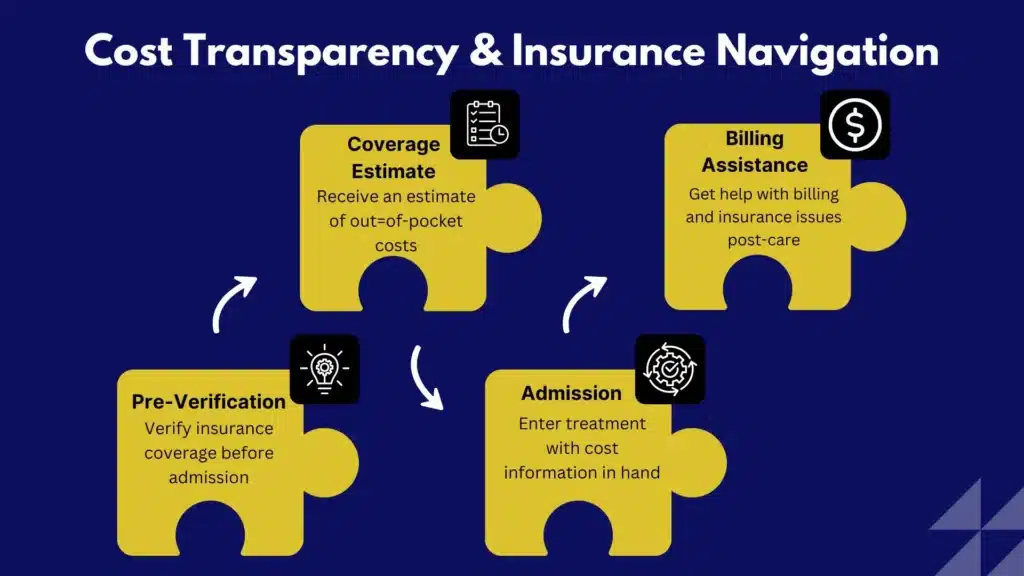
- Verify insurance benefits and out-of-pocket costs
- The intake team should run a real-time benefits check, explain in-network status, deductibles, copays, and coinsurance, and outline parity protections under state and federal law. Patients should receive a written estimate before admission and ongoing updates if the length of stay changes.
- Complete biopsychosocial and ASAM multidimensional assessment
- A licensed clinician conducts a comprehensive assessment that covers the six ASAM dimensions: acute intoxication/withdrawal potential; biomedical conditions; emotional/behavioral conditions; readiness to change; relapse/continued use risk; and recovery environment. This places the patient at the right level of care and guides initial goals.
- Lab work and withdrawal risk scoring
- Baseline labs often include CBC, CMP, liver enzymes, bilirubin, coagulation if indicated, electrolytes (including magnesium and phosphate), pregnancy testing when relevant, and blood alcohol level if recent use. Vital signs, CIWA-Ar scoring for alcohol withdrawal severity, and physical exam guide safety measures. Thiamine is administered before glucose when the Wernicke risk is present; folate and multivitamins are common.
- Medications for withdrawal and craving management
- Benzodiazepines (e.g., diazepam, lorazepam) are used for moderate to severe withdrawal, following symptom-triggered or fixed-dose protocols under physician orders. Adjuncts may include gabapentin, clonidine, or beta-blockers for autonomic symptoms; antipsychotics are used cautiously for severe agitation. Seizure precautions and escalation pathways are standard. After stabilization, medication to support recovery, naltrexone or acamprosate, is discussed with shared decision-making and lab review.
- Safety, privacy, and orientation
- Patients receive a privacy notice, consent forms, release of information options, and a safety orientation that includes fall prevention, sharps policies, and medication storage. A personal treatment plan is drafted within the first 24–72 hours with measurable, time-bound goals.
For individuals seeking a discrete, medically supervised start, Rolling Hills Recovery Center has New Jersey alcohol detox partners align stabilization with the person’s longer-term treatment plan from day one.
What to Bring vs. What to Leave
- Bring:
- Photo ID and insurance card
- Current medication list and pharmacy information
- Comfortable clothing without strings when required; closed-toe shoes; limited toiletries in original packaging
- Contact information for approved family/support persons and outpatient providers
- Leave:
- Valuables beyond essentials, large amounts of cash
- Alcohol, substances, or vape devices
- Unapproved supplements or medications not verified by staff
- Recording devices or cameras where privacy rules restrict usage
Programs explain device and visitor policies up front, balancing connection with privacy and unit safety.
Daily Treatment Structure and Outcomes
A private clinic schedules each day to combine medical oversight, therapy, and skills practice. The structure remains steady but is tailored to clinical needs.
A Sample Day in Private Residential or PHP Treatment
| Time | Activity |
|---|---|
| 7:00–8:00 AM | Nursing check-in, vitals, medications, breakfast |
| 8:15–9:00 AM | Community meeting and mindfulness practice |
| 9:15–10:15 AM | Individual therapy (CBT/MI) or psychiatry follow-up |
| 10:30–12:00 PM | Skills group (trigger mapping, coping strategies, sleep hygiene) |
| 12:00–1:00 PM | Lunch and recovery reading/self-reflection |
| 1:15–2:15 PM | Trauma-informed group or experiential therapy |
| 2:30–3:30 PM | Family session or case management (work/school planning, legal, FMLA) |
| 3:45–4:45 PM | Physical wellness or yoga; stress reduction practices |
| 5:00–6:00 PM | Dinner |
| 6:15–7:00 PM | Peer support meeting or relapse prevention group |
| 7:15–8:00 PM | Journaling, recovery assignments, quiet hours |
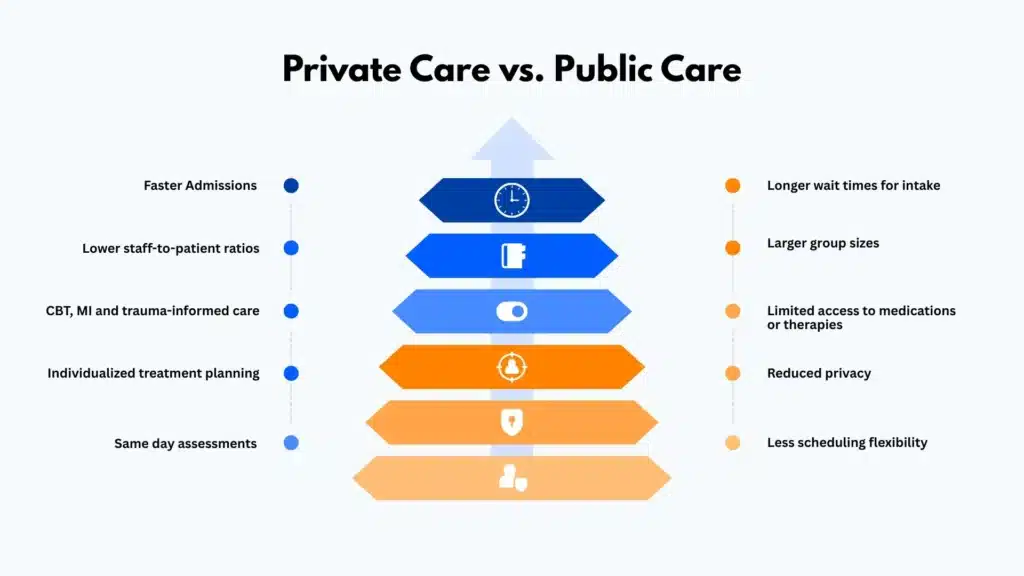
Medical rounds occur daily in higher-intensity settings; in outpatient settings, medical follow-ups are typically weekly or biweekly. The frequency of individual therapy is higher in private settings due to smaller caseloads.
Recovery Capital and Measurable Goals
Recovery capital represents the personal, social, and community resources that support sustained recovery. Private clinics often create a recovery capital plan with specific aims such as:
- Housing stability and a sober living option if needed
- Employment or education re-entry timeline
- Primary care connection and management of medical conditions (e.g., hypertension, liver health)
- Social support mapping (peer recovery, family, and community)
Goals should be specific, measurable, attainable, relevant, and time-bound, for example:
- “Reduce Penn Alcohol Craving Scale score by 50% within 4 weeks”
- “Attend 3 peer-support meetings weekly for 8 weeks”
- “Demonstrate 4 coping strategies for high-risk triggers by week 3”
Discharge Criteria and Continuing Care
Discharge is based on ASAM criteria, not arbitrary dates. Criteria commonly include:
- Medical stabilization and managed withdrawal risks
- Demonstrated coping skills for identified triggers
- A medication plan is in place for upcoming appointments
- Documented linkages: therapy, IOP, peer supports, and primary care
- Safe housing and transportation plan
The team builds a written relapse prevention plan with warning signs, crisis steps, and support contacts. For many, a step-down to IOP is recommended; Rolling Hills provides a seamless transition to structured outpatient supports.
Realistic Timelines and Compassionate Messaging
Alcohol use disorder is a chronic condition for many, and recovery is a process; relapse can occur and is not a moral failing.
Private programs set realistic timelines: detox may take days; stabilization in inpatient or PHP may take several weeks; medication optimization and therapy continue for months; and recovery maintenance often continues for a year or longer.
Measured improvements in sleep, mood, liver markers, and social functioning are celebrated. The tone stays compassionate and stigma-free, with the message that help works when it is persistent and matched to need.
NJ-Specific Oversight and Parity Protections
In New Jersey, DMHAS oversight guides licensing and safety requirements, while federal and state mental health parity laws require equitable coverage for substance use treatment.
Billing teams in private clinics should advocate for medically necessary lengths of stay and explain appeal processes if coverage is denied.
Patients receive clear financial updates and copies of all utilization review communications upon request.
How to Choose a Private Clinic Safely
Selecting a private alcohol rehab should be methodical and evidence-focused.
Verify Credentials and Clinical Governance
- Credentials and staff composition
- Look for board-certified addiction medicine physicians (ABPM or ABAM), psychiatrists with addiction subspecialty training, licensed therapists (LCSW, LPC, LMFT), and 24/7 nursing in higher-acuity settings.
- Ask who writes orders for detox medications, who manages alcohol use disorder pharmacotherapy, and how on-call coverage works.
- Evidence-based modalities
- Confirm use of CBT, MI, and medication-assisted treatment with naltrexone or acamprosate (as appropriate). Request sample curricula for groups and relapse prevention. Ask how co-occurring disorders are treated, including trauma-informed approaches.
- Program metrics
- Reputable clinics can discuss de-identified outcomes and quality indicators such as completion rates, 30- and 90-day follow-up engagement, medication adherence, and readmission rates. Methodology should be clear; guarantees are not credible given the chronic nature of the condition.
- Safety and emergency protocols
- Ask about CIWA-Ar protocol use, seizure management, rapid transfer agreements with hospitals, and how medical emergencies are handled. Inquire about infection control, medication reconciliation, and adverse event reporting.
- Medication management and lab monitoring
- Review how labs are used to inform medication choices, how side effects are monitored, and how coordination occurs with primary care and specialists.
- Secure data and privacy practices
- Confirm HIPAA-compliant EHR, role-based permissions, encrypted communications, and how photos or devices are managed on-site. Patients should receive a Notice of Privacy Practices and have options to restrict disclosures. Reference: HHS – HIPAA Summary.
- Transparent cost and insurance navigation
- The clinic should provide a written financial agreement, itemized billing, and clear policies for refunds, single-case agreements, and authorizations. Parity education should be part of the financial discussion.
For those prioritizing a private, low-stimulation environment with attentive service, amenities should support clinical work but not replace it.
Rolling Hills Recovery Center meets clinical needs first and also offers comfort-forward settings; see this article on luxury rehab centers in NJ for details on privacy and supportive amenities integrated with evidence-based care.
Red Flags to Avoid
- “Guaranteed cure,” fixed success rates without methodology, or promises of fast recovery regardless of history
- Vague pricing or refusal to provide itemized cost estimates in writing
- No named medical director, unclear detox protocols, or lack of 24/7 medical coverage where withdrawal is treated
- No discussion of medications for alcohol use disorder, or outright dismissal of evidence-based pharmacotherapy
- Limited family communication policies without respect for privacy law and patient preference
- No published patient rights, safety policies, or clear complaint procedures
- Pressure tactics to enroll immediately without a professional assessment
Putting it Together in Practice at a Private Clinic
A typical pathway at a private clinic such as Rolling Hills Recovery Center will look like this:
Assessment and Placement
An intake specialist gathers medical and substance use history, screens for withdrawal risk, and schedules immediate admission if safety requires.
Once on-site, a clinician completes the biopsychosocial and ASAM assessment and develops a personalized treatment plan that covers both alcohol use and mental health needs.
Family supports are engaged with patient consent.
Stabilization with Medical Oversight
If alcohol withdrawal is expected, a symptom-triggered benzodiazepine protocol is initiated with CIWA-Ar monitoring, thiamine is given, hydration and nutrition are supported, and safety rounding is frequent.
Psychiatric consultation occurs quickly for co-occurring conditions.
Therapy and Skill-Building
Daily CBT and MI sessions focus on triggers, cravings, decision balance, self-efficacy, and coping skills. Group work covers relapse prevention, stress regulation, and relationships.
When clinically appropriate, medications such as naltrexone or acamprosate are started with lab-informed dosing and education on benefits and side effects.
Family and Social Supports
With consent, family sessions address communication patterns, boundaries, and practical support.
Case managers coordinate work or school notes, FMLA, legal needs, and housing stability. Recovery capital building continues each week.
Step-Down and Ongoing Care
As withdrawal risks resolve and coping skills improve, many transition to PHP, then IOP, or directly to IOP from detox when safe.
Outpatient therapy and medication management continue; peer support and community health connections are reinforced.
Rolling Hills Recovery Center links patients seamlessly to structured outpatient programming through outpatient alcohol rehab centers in NJ when indicated.
Outcomes and Quality Monitoring
Progress is tracked using craving scales, symptom measures, attendance, medication adherence, and patient-reported outcomes.
Discharge planning includes written relapse prevention, scheduled follow-ups, and emergency instructions. Post-discharge check-ins promote continuity and early intervention if risks increase.
Private alcohol rehab programs in New Jersey succeed when they combine medical rigor, person-centered therapy, and strong privacy protections.
Patients should expect clear standards, honest communication, and a care plan that evolves with their needs, not the other way around.
Conclusion
This article reviewed the path to private alcohol rehab in NJ, assessment, detox, therapy, medication, privacy, and aftercare. Key points: start early, combine medical care & counseling, plan insurance, and discharge.
Frequently Asked Questions (FAQs)
What Happens During Medical Detox at a Private Alcohol Rehab Clinic in New Jersey?
In an alcohol rehab clinic, medical detox is supervised by licensed clinicians who track withdrawal symptoms, check vitals, and use standardized tools to rate risk.
When indicated, medications are started to reduce withdrawal discomfort and prevent complications like seizures.
Care usually includes quiet rooms, hydration, sleep support, and monitoring day and night. If anxiety or insomnia appears, the team adjusts the plan promptly.
The goal is safe stabilization so therapy can begin, not just “toughing it out.”
How Long Does Treatment Last at a Private Alcohol Rehab Clinic, and What Levels of Care Are Typical?
Length varies based on clinical need and progress. In an alcohol rehab, detox often lasts 3–7 days, residential treatment may run 2–4 weeks (sometimes 30+ days), partial hospitalization (PHP) about 2–4 weeks, and intensive outpatient (IOP) 6–12 weeks.
Some people step down through levels of care, while others begin in IOP when safe. The care plan is individualized, reviewed weekly, and adjusted so gains are real & lasting.
How Private is a Private Alcohol Rehab Clinic in NJ, and What Protects Confidentiality?
An alcohol rehab clinic follows HIPAA privacy rules and New Jersey regulations, with strict limits on who can access records.
With written consent, the team may share need-to-know details with a chosen family member or physician; without consent, they do not.
Discreet admissions, secure data systems, and small clinical caseloads help protect identity. Many clinics also use first-name only policies on-site—simple steps, strong boundaries.
How Do Costs and Insurance Work at a Private Alcohol Rehab Clinic in New Jersey?
Before admission, an alcohol rehab typically verifies benefits, explains in-network or out-of-network coverage, and estimates out-of-pocket costs.
Deductibles, co-pays, and length of stay all affect the final bill. Financial counselors help with payment plans and letters of medical necessity when needed.
Patients are encouraged to ask for clear written summaries, no surprises, plain numbers, and honest timelines.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts