Functional alcoholism often hides behind steady work, family duties, and social routines. From a medical standpoint, it reflects Alcohol Use Disorder that remains concealed but carries real health & safety risks.
This introduction outlines how to spot warning signs of alcoholism, what the science says, and practical, discreet next steps for New Jersey individuals and families.
Key Takeaways
- Even when life looks stable, alcohol can disrupt sleep, blood pressure, liver, and mood; it also raises injury & crash risk. Weekend binge drinking still carries real harm.
- Functional alcoholism is Alcohol Use Disorder; not a separate diagnosis. A person may keep work and family roles yet show loss of control, tolerance, or withdrawal.
- Quick screens (AUDIT, CAGE) plus clinician review and basic labs can size up risk; red flags include morning drinks, tremor, blackouts, or mixing with sedatives, especially in routine New Jersey care.
- Safer next steps: do not detox alone; consider FDA‑approved medicines like naltrexone or acamprosate; stay hydrated and take thiamine; track triggers; set simple goals. Workplace protections in NJ may help.
Why Functional Alcohol Use Often Goes Unnoticed and Why It Still Harms
In many New Jersey households and workplaces, alcohol use blends easily into daily life. Routines, professional norms, and even cultural expectations can hide the signs of an emerging Alcohol Use Disorder (AUD), especially when someone appears to be functioning well on the surface. This “functional” pattern often delays recognition and treatment.
Consider the familiar routines: after-work drinks on the Northeast Corridor commute, client dinners in sales or finance, or a glass of wine during a caregiving break or late-night shift.
These habits feel typical and socially accepted, which makes it easier to ignore how much drinking has increased. Rationalizations like “I’ve never missed work,” or “It’s just wine on weekends” are common.
In high-pressure New Jersey industries, where performance is highly valued, these narratives can delay much-needed help.
The Hidden Health Effects of High-Functioning Drinking
Even when life seems stable, regular alcohol use can cause significant health damage. It interferes with sleep quality, often leaving people exhausted even after a full night’s rest.
Alcohol also raises blood pressure, affects heart rhythm, and harms liver function. Over time, these changes can lead to fatty liver, hepatitis, and in some cases, cirrhosis.
Digestive issues like reflux, gastritis, and pancreatitis are also common. Alcohol weakens the immune system, increasing the likelihood of infections. These effects often go unnoticed until symptoms become more serious.
For medical thresholds and evidence-based information, see trusted sources like the CDC’s Alcohol resources and the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Hidden Safety Risks That Build Over Time
Even without obvious signs of intoxication, safety risks may increase over time. Driving the next morning after drinking can still leave a person over the legal limit, especially if alcohol was consumed late at night. Combining alcohol with anxiety or sleep medications such as benzodiazepines or Z-drugs significantly raises the risk of overdose.
Other risks include injuries from falls, workplace accidents, or unsafe sexual situations. As drinking increases, people may begin relying on alcohol more often and staying out later. Blackouts can become more frequent, even if the person believes they are in control.
The Stigma That Delays Help
Stigma remains one of the biggest barriers to treatment. Many people assume that if they are working, paying bills, and caring for family, they cannot possibly have a drinking problem. This belief is incorrect. Functional AUD is still dangerous, and waiting for a “crisis” often leads to more complicated medical or legal consequences. Early support is safer and far more effective.
Why the New Jersey Lifestyle Plays a Role
New Jersey’s unique lifestyle contributes to how alcohol use develops. Post-work drinks in Hoboken or Jersey City, late-night routines among healthcare or hospitality workers, and high-stress corporate jobs all make drinking feel routine. For many, it becomes a way to decompress.
However, New Jersey has some of the strictest DWI laws in the country. Sobriety checkpoints and ignition interlock requirements can lead to lasting consequences. Many people do not realize the risk until a legal or workplace issue arises.
Fortunately, most employers offer Employee Assistance Programs (EAPs), and health insurance often covers the cost of evaluation and treatment. The New Jersey Division of Mental Health and Addiction Services (DMHAS) offers updated statewide policies and referral information for those ready to take the next steps.
Stigma and the Myth of “Not Having a Problem” When Milestones are Met

Stigma, the fear of being labeled an “alcoholic” usually keeps people from getting care. The myth says: as long as a person has a job, pays the mortgage, and shows up for family, there is no problem. Clinically, this is false. Functional AUD carries real risk; earlier support nearly always leads to safer outcomes.
Rolling Hills Recovery Center offers comprehensive care for Alcohol Use Disorder, including therapy, medication, and relapse prevention strategies. Learn more about treatment for alcoholism tailored to professionals and families across New Jersey.
New Jersey Context: Commuting, Careers, and Policy
In New Jersey, post-work drinking is common in areas like Hoboken, Jersey City, Newark, and along NJ Transit routes, which can leave individuals with lingering intoxication into the early morning hours.
Within professional services and finance, client entertainment is a routine part of business culture, and the stress of high-performance environments often fuels after-hours alcohol use.
For those in service industries and shift-based jobs such as restaurants, healthcare, or hospitality, with unusual hours and split shifts frequently lead to late-night drinking patterns that interfere with restful sleep and long-term recovery.
At the same time, New Jersey enforces some of the strictest DWI laws in the country. Sobriety checkpoints and ignition interlock devices can result in lasting legal and employment issues for those caught driving under the influence.
Fortunately, many workplaces offer Employee Assistance Programs and health insurance coverage that include evaluations for Alcohol Use Disorder. Accessing these resources early allows for discreet support before more serious consequences arise.
The New Jersey Division of Mental Health and Addiction Services maintains statewide information and policy updates: NJ DMHAS.
Screening and Diagnosis Pathways
Brief Self-Checks: CAGE and AUDIT
Self-check tools are a good first step, not a label. Two widely used tools:
- CAGE (4 questions; 2+ “yes” suggests a problem)
- Tried to Cut down?
- Annoyed by criticism of drinking?
- Felt Guilty?
- Eye-opener (drink in the morning)?
- AUDIT (Alcohol Use Disorders Identification Test; 10 items scored 0–40)
- Scores: 8+ suggests hazardous use; 16+ indicates higher risk.
- Validated by the World Health Organization; details and form at WHO: WHO AUDIT
Results from these should guide a primary care visit or addiction assessment, not self-diagnosis. A clinician can check labs, medications, mental health, and discuss options.
Helpful tip: keep a 7-day drink log before the appointment, including time, amount, context, sleep quality, and any withdrawal symptoms the next morning.
When a Primary Care Visit is Safer Than Self-Labeling
A primary care or addiction medicine visit is recommended when:
- There’s daily or near-daily drinking.
- There are blackouts, morning shakes, nausea, or sweats.
- There are chronic illnesses (hypertension, diabetes, liver disease).
- Medications could interact (benzodiazepines, sleep meds, opioids).
- A person is unsure whether to taper, stop, or seek medical detox.
Medical teams can tailor the safest plan and prescribe evidence-based medications when appropriate.
DSM-5 AUD Severity and What it Means for Care
The DSM-5 criteria include impaired control, social impairment, risky use, and pharmacologic indicators (tolerance, withdrawal). Severity levels:
- Mild AUD: 2–3 symptoms. Brief counseling, goal setting, and medication may help.
- Moderate AUD: 4–5 symptoms. Structured therapy plus medication is often needed.
- Severe AUD: 6+ symptoms. Comprehensive treatment, sometimes with medical detox, is safest.
NIAAA’s clinical guidance summarizes diagnostic features and treatment options: NIAAA.
Red Flags That Warrant Same-Week Evaluation
- Morning drinking to relieve shakes or nausea.
- History of alcohol withdrawal seizure or delirium tremens.
- Blackouts in the past month.
- Falls, head injuries, or car crashes linked to alcohol.
- Mixing alcohol with benzodiazepines, opioids, or sedative hypnotics.
- Pregnancy or trying to conceive.
- Suicidal thoughts or severe depression.
If any are present, urgent medical assessment is recommended. Do not attempt to stop suddenly without medical advice if daily heavy use is present.
Co-Occurring Anxiety and Depression Are Common
Functional AUD commonly coexists with anxiety, panic, or depressive symptoms. While alcohol can feel like short-term relief, it worsens mood and sleep, and increases anxiety rebound.
Integrated care is addressing both AUD and mental health improves outcomes. Primary care, psychiatry, and addiction specialists work together on this; medications for anxiety or sleep are chosen carefully to avoid interaction risks.
Health Risks and Safety
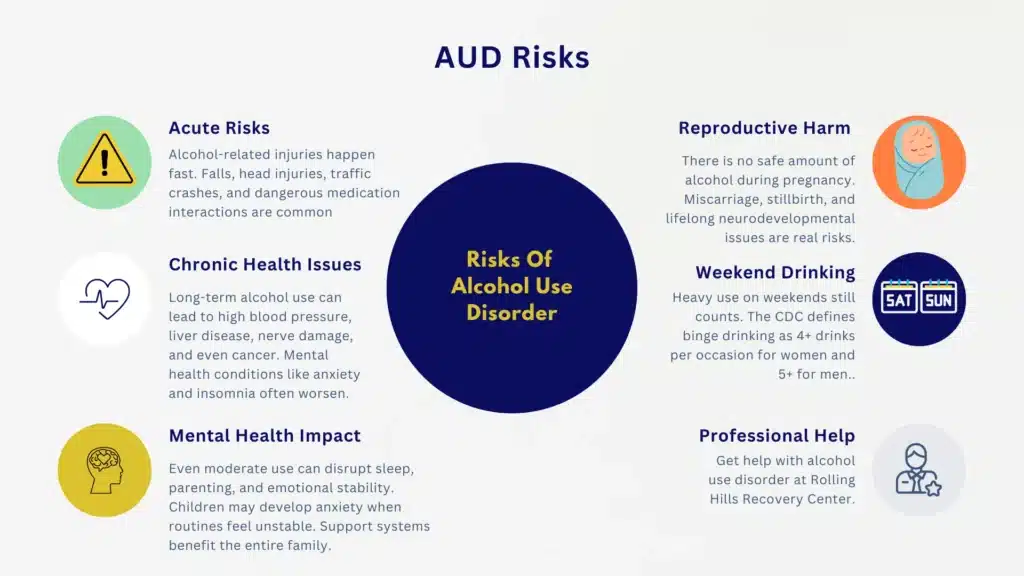
Alcohol use carries both immediate and long-term risks that may be overlooked in individuals who appear to function well in daily life. Acute dangers include an increased likelihood of falls, fractures, and head injuries, particularly in environments such as icy sidewalks or staircases.
Driving under the influence, even the morning after a night of heavy drinking, can result in accidents due to residual impairment. Alcohol also plays a role in escalating interpersonal violence, injuries, and legal problems during intoxicated states.
Mixing alcohol with medications such as benzodiazepines, opioids, or certain sleep aids increases the risk of respiratory depression and overdose. At high doses, alcohol poisoning can occur, sometimes with fatal consequences.
Chronic alcohol use affects nearly every organ system. Cardiometabolic risks include high blood pressure, irregular heart rhythms such as atrial fibrillation, weakened heart muscle (cardiomyopathy), and increased stroke risk.
Gastrointestinal issues like gastritis, ulcers, and pancreatitis may emerge over time. In the liver, conditions can progress from fatty liver to alcoholic hepatitis and cirrhosis. Long-term alcohol use is also associated with several cancers, including oral, esophageal, liver, breast, and colorectal cancer.
Neurologically, people may experience peripheral nerve damage or cognitive decline. Thiamine deficiency caused by alcohol can lead to Wernicke-Korsakoff syndrome, a serious brain disorder. Mental health also suffers, with elevated risks of depression, anxiety, and sleep disturbances.
Alcohol use during pregnancy presents its own dangers. There is no known safe amount of alcohol during pregnancy. Consuming alcohol while pregnant can lead to miscarriage, stillbirth, or fetal alcohol spectrum disorders.
People planning to become pregnant should speak with a clinician early and may benefit from medical strategies to support alcohol cessation before conception.
Alcohol’s effects are rarely limited to the individual. In family systems, even occasional heavy drinking can reduce emotional availability, increase co-parenting stress, and create inconsistency in caregiving roles.
This is especially concerning for those responsible for older adults or young children. Children in these households may develop anxiety or struggle with unpredictable routines. Counseling, mutual-help groups, and family-focused education can offer valuable support to loved ones.
It’s important to note that even weekend-only drinking can be problematic. Binge drinking is defined by the CDC as consuming five or more drinks for men or four or more for women on a single occasion, which creates risks regardless of weekday abstinence.
Heavy drinking is defined as 15 or more drinks per week for men, or 8 or more for women. These patterns can lead to dependency and deserve attention even in the absence of daily use. Binges can still meet AUD criteria if consequences or failed cutbacks are present. See definitions at CDC Alcohol.
Evidence-Based Next Steps in New Jersey
Recovery is most effective when it blends evidence-based care with local, ongoing support. Individuals navigating functional alcoholism in New Jersey have access to a wide range of resources:
- Mutual-Help Groups: Options like Alcoholics Anonymous (AA) Northern New Jersey Intergroup, SMART Recovery, or Women for Sobriety, which offer peer-based support in person or online.
- Community and Family Services: Family therapy, EAP support, and educational groups can help loved ones stay involved and reduce isolation.
- Local Support Near You: While our facility is based in Chester, we proudly serve individuals across Morris County including Morristown, NJ addiction treatment services.
Discreet Planning for a Medical Assessment
A practical, low-drama way to get evaluated in New Jersey:
- Choose a primary care clinician or addiction specialist covered by insurance. Consider an EAP referral for added confidentiality.
- Schedule a morning appointment within 7–10 days.
- Keep a 7-day drink log (see template below) and list all medications and supplements.
- Plan safe transportation on appointment day; avoid driving if there was heavy use the night before.
- Ask for blood pressure, liver enzyme tests, and an AUD screening (AUDIT or DSM-5 checklist).
- Discuss personal goals openly: reduce, stop, or “not sure yet.”
For statewide information and links to services, New Jersey residents can review NJ DMHAS.
Drink log template (copy to notes app or paper):
- Date:
- Time of first drink:
- Type and number of drinks:
- Context (alone, with coworkers, event):
- Mood before/after:
- Sleep quality:
- Morning symptoms (headache, shakes, anxiety, nausea):
- Medications taken that day:
Discussing Goals: Cut Down Versus Abstain
Many individuals start with a “cut down” goal. Clinicians can help decide what is realistic and safe.
Simple guide:
- Consider a cut-down trial if there is no history of withdrawal seizures, daily morning relief drinking, or severe liver disease, and if medications can be used to support reduction.
- Choose abstinence if there’s moderate-to-severe AUD, repeated failed cut-down attempts, health events linked to alcohol, pregnancy, or complex medication interactions.
Short comparative view:
| Decision factor | Cut down may fit when | Abstain may be safer when |
|---|---|---|
| Withdrawal risk | No morning shakes; no prior seizures | Morning relief drinking, prior withdrawal, heavy daily use |
| Health status | No severe liver, cardiac, or pancreatitis issues | Liver disease, arrhythmia, pancreatitis, pregnancy |
| History | Few failed cut-down attempts | Repeated relapses after cutting back |
| Medications | No high-risk sedatives | Benzodiazepines, opioids, or sleep meds in use |
| Safety | No DUIs, no injury history | DUI, falls, blackouts, injuries present |
If uncertain, clinicians often start with a low-risk abstinence trial for 4–6 weeks with medication support, then reassess.
Medications for Alcohol Use Disorder That Actually Work

When treating Alcohol Use Disorder (AUD), several FDA-approved medications are available that have been shown to reduce cravings and improve outcomes when used alongside therapy. Each option has specific benefits and risks, and it’s essential to discuss them with a qualified clinician before starting.
Naltrexone, available as a daily oral tablet or a monthly injection, can significantly reduce heavy-drinking days and overall cravings. However, it should be avoided in individuals with acute hepatitis or liver failure, and it cannot be used in combination with opioids.
Acamprosate is typically taken three times daily and works by stabilizing the brain’s glutamate and GABA balance, which supports abstinence. It’s considered safe for individuals with liver disease, but dose adjustments may be needed if there are kidney function concerns.
Disulfiram works differently. It causes an unpleasant physical reaction if alcohol is consumed, which makes it most effective when use is supervised. It’s often used in structured treatment programs where support systems are in place.
While these are the primary FDA-approved medications, other treatments are sometimes used off-label in clinical practice. Medications like topiramate or gabapentin may help reduce cravings and improve sleep or anxiety symptoms.
Though not officially approved for AUD, they can be appropriate in select cases based on a patient’s unique health profile and goals.
For detailed clinical information and guidance on these medications, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) offers helpful resources for both patients and providers.
Harm Reduction While Preparing for Treatment
In some cases, stopping alcohol suddenly can trigger withdrawal, especially when daily use is heavy or when symptoms like morning nausea or shaking are present. If you’re preparing for a medical visit or arranging care, there are steps that can reduce risk in the meantime.
First and foremost, never attempt to detox alone if you suspect withdrawal symptoms may occur. Medical oversight ensures safety, especially when symptoms include tremors or sleep disturbances.
Maintaining hydration and consistent meals is also important. Electrolyte drinks and balanced nutrition can support the body during early recovery.
Many clinicians recommend taking thiamine (vitamin B1) at 100 mg daily, along with a general multivitamin, particularly if appetite has been low.
If social events or routines involve alcohol, making small adjustments can help reduce harm. This might include setting a firm “stop” time earlier in the evening, spacing drinks with non-alcoholic beverages in between, and eating beforehand to slow absorption.
Reducing alcohol strength by choosing lower-ABV options also matters. It may help to secure or remove alcohol from your home, and to ask a trusted person to offer support if you’re trying to cut back.
Protecting sleep is also a key strategy. Turning off screens earlier, establishing a calming nighttime routine, and keeping a consistent bedtime can help stabilize mood and reduce cravings.
When urges spike, even a short walk, a cold shower, or a quick call to a supportive friend can help. Cravings tend to peak and pass within 20 to 30 minutes, and learning to ride those waves is a powerful recovery tool.
Using Tracking Tools to Support Progress
Many people find that tracking their behavior helps build awareness and momentum during recovery. A daily drink log is a simple way to start, even if just noting time, quantity, and setting.
Identifying high-risk situations, such as drinking after late shifts, during child bedtime routines, or in specific social environments, helps map out personal triggers.
Medication side effects and benefits can also be tracked with simple scales, like rating cravings or noting any physical changes. Some individuals also use mood or sleep quality scores to identify patterns.
Often, improved sleep is one of the first signs that recovery is taking hold, whether using a phone notes app, spreadsheet, or calendar. Consistency in tracking is more important than the method itself.
Local Resources and Considerations in New Jersey
New Jersey residents have access to a range of support systems that can make recovery more accessible. Most commercial insurance plans and NJ FamilyCare include coverage for AUD evaluation, medication, and outpatient care.
Many primary care practices in the state now offer next-week appointments specifically for substance use concerns.
Workplace support is another important area. Many employers offer Employee Assistance Programs (EAPs), which can be used confidentially without notifying supervisors. It’s a good idea to confirm EAP use policies with your HR department if you have questions.
Legal protections and risks also vary by role. Commercial drivers and certain licensed professionals in New Jersey may be subject to stricter zero-tolerance policies. Planning alternate transportation and avoiding high-risk environments are essential steps to maintaining safety and stability during recovery.
Community-based support remains a valuable layer of care. Mutual-help meetings, peer recovery centers, and family-focused support groups operate throughout the state.
The New Jersey Division of Mental Health and Addiction Services (DMHAS) maintains an up-to-date list of local programs, policies, and available services.
A 72-Hour Plan to Get Evaluated Safely
Day 1:
- Schedule a primary care or addiction consultation.
- Begin the 7-day drink log.
- Set a conservative drinking limit for the next two nights or discuss a medically guided taper with a clinician if needed.
- Remove high-ABV liquor from the home; leave lower-ABV options if tapering is necessary for safety.
Day 2:
- Take thiamine and a multivitamin.
- Confirm transportation for the appointment.
- Identify two high-risk times; create replacements (gym class, evening walk, call with a friend).
- Review medications for interactions and list them for the clinician.
Day 3:
- Sleep focus: aim for a consistent bedtime.
- Write 3 goals to discuss (e.g., fewer heavy nights, better mornings, no blackouts).
- Prepare questions about medication options.
- If withdrawal symptoms intensify (shakes, sweating, anxiety, nausea), escalate promptly to same-week evaluation.
How Rolling Hills Recovery Center Supports Functional AUD in New Jersey

Rolling Hills Recovery Center delivers evidence-based and holistic care designed specifically for individuals managing demanding careers, family obligations, and other high-functioning responsibilities. For those dealing with functional Alcohol Use Disorder (AUD), certain needs often rise to the surface.
Many clients benefit from discreet intake and assessment processes that respect their time and privacy, allowing them to seek help without disrupting work or family routines.
Medication management is frequently part of the care plan, using options such as naltrexone, acamprosate, or disulfiram alongside personalized therapy.
Treatment also emphasizes cognitive-behavioral strategies to address specific stressors, like commuting stress, client entertainment expectations, or late-night shift work. When helpful, family involvement can be incorporated to reinforce structure and communication at home.
Planning for long-term recovery goes beyond treatment sessions. Clients work with clinicians to develop step-down strategies and relapse prevention plans rooted in real-life New Jersey scenarios, holiday triggers, weekends at the shore, irregular hospitality schedules, and business travel.
For anyone stuck in the cycle of ambivalence, this common internal conflict often surfaces: “I want to stop using drugs and alcohol, but I can’t.” Rolling Hills helps individuals confront that crossroads with evidence-informed support and nonjudgmental care.
Practical Tools, Checklists, and How-to Steps
Rapid Self-Check Toolkit
- CAGE: answer the four questions; two or more “yes” answers, then plan a clinician visit.
- AUDIT: complete the 10-item form via WHO; score 8+, schedule evaluation; 16+, prioritize care promptly. Tool link: WHO AUDIT
- Red flags checklist:
- Morning relief drinking
- Shakes, sweats, nausea on waking
- Blackouts
- Injuries or DUIs
- Mixing with sedatives
- Pregnancy or trying to conceive. If any item is present, seek same-week medical evaluation.
Medication Conversation Starter (Bring to Appointment)
- Goals: reduce heavy-drinking days; abstain for 6 weeks; improve sleep; protect liver.
- History: prior attempts; any withdrawal symptoms; blackouts; injuries; family history.
- Medical: liver or kidney issues; current meds; pregnancy plans.
- Ask: Is naltrexone, acamprosate, or disulfiram appropriate? What are the pros and cons for this situation?
NIAAA’s patient materials offer accessible descriptions of these options: NIAAA.
Safer-Socializing Template (NJ Context)
- Before the event: eat a full meal; set a 2-drink maximum; arrange a ride-share from Newark Penn or a designated driver in Monmouth/Middlesex counties.
- During: alternate with water or seltzer; avoid shots; stop 90 minutes before leaving.
- After: no “nightcap” at home; prioritize sleep routine.
- Next morning: no driving until fully alert; skip if unsure.
Workplace Planning in New Jersey
- Review EAP benefits and confidentiality.
- Ask HR about time-limited medical leave if needed for treatment.
- Document performance metrics; many individuals improve productivity within weeks of cutting down or abstaining.
- Discuss scheduling flexibility during early treatment weeks if possible.
Family Alignment Steps
- One short, nonjudgmental conversation at a neutral time: “Health is a goal; an evaluation is scheduled.”
- Agree on a plan for alcohol in the home during the next 4–6 weeks.
- Share emergency steps if withdrawal worsens (urgent care/ED).
- Consider a family session with a counselor to set supportive boundaries.
For an additional perspective on functioning with substance use, Rolling Hills Recovery Center covers broader patterns here: What is drug addiction?
Evidence and References for Further Reading
- National Institute on Alcohol Abuse and Alcoholism: definitions, health effects, and medications for AUD: NIAAA
- Centers for Disease Control and Prevention: binge thresholds, population data, and health risks: CDC Alcohol
- World Health Organization AUDIT screening tool: WHO AUDIT
Conclusion
Functional alcoholism can look stable, yet it is Alcohol Use Disorder that quietly harms health and daily life. Key points: watch for rising tolerance and morning relief use, know the real medical risks & get screened, plan safer change.
For more on how high-functioning alcoholism is affecting professionals in New Jersey, read our press release: (https://www.einpresswire.com/article/861982854/high-functioning-alcoholism-in-new-jersey-a-hidden-pattern-among-professionals-raises-concern).
Frequently Asked Questions (FAQs)
What is Functional Alcoholism, and How is it Different From Other Alcohol Problems?
Functional alcoholism refers to Alcohol Use Disorder (AUD) in someone who still keeps a job & family roles, often without obvious crises.
Clinically, it still meets DSM-5 criteria: loss of control, cravings, rising tolerance, withdrawal symptoms, and ongoing use despite harm.
The difference is mostly in appearance and how life looks “together,” but health, safety, and relationships are still at risk.
What Early Signs of Functional Alcoholism Should Be Watched in Everyday Life?
Common early signs include rising tolerance (needing more to feel the same), drinking earlier in the day, blackouts or memory gaps, irritability on non-drinking days, hiding alcohol, unexplained stomach issues, sleep problems, or small work slip-ups like missed deadlines.
Occasional DUI, mixing alcohol with sleep meds, or “relief” drinks in the morning are red flags too.
Is it Safe to Cut Down or Stop Drinking Without Medical Help if Functional Alcoholism is Present?
Not always. If there are tremors, sweats, anxiety, nausea, or a history of heavy daily use, withdrawal can become dangerous and rarely seizures or delirium tremens.
Safer steps include medical evaluation first, thiamine before cutting back, hydration, and avoiding benzodiazepines or opioids with alcohol.
Urgent care or emergency services are needed if there’s confusion, vomiting that won’t stop, seizures, or chest pain. No one should detox alone at home, especially after long-term, heavy use.
What Screenings and Tests Help Confirm Functional Alcoholism During a Clinical Visit?
Clinicians often use brief screens like AUDIT or CAGE, followed by DSM-5 criteria to determine severity (mild, moderate, severe). Basic vitals and exams matter, and common labs may include AST, ALT, GGT, MCV, and sometimes CDT to look for alcohol-related changes.
A medication and mental health review is also key, since anxiety or depression can travel with AUD. In New Jersey, these can be done discreetly in primary care or specialized settings.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












