Xylazine, often called “tranq,” is increasingly found in illicit fentanyl and heroin, compounding overdose & wound risks. This overview explains what clinicians and families should know: effects, unique skin injuries, overdose response with naloxone, safer‑use basics, and pathways to evidence‑based care, so people can act fast and reduce harm. It also outlines wound care strategies and linkage to recovery support.
Key Takeaways
- Tranq (xylazine) is showing up in fentanyl & heroin; it adds deep sedation and raises overdose risk.
- Give naloxone right away for suspected overdose; it treats the opioid part, then support breathing and call 911.
- Xylazine wounds can worsen fast… clean with saline, use non‑stick dressings, avoid injecting into wounds, see a clinician early.
- Many routine drug screens miss xylazine, ask for specific testing, and connect care to OUD medicines and wound treatment.
Definition and Street Context

“Tranq” refers to xylazine, a non‑opioid veterinary sedative. It is not approved for human use. In the illicit market, xylazine is often mixed into fentanyl or heroin and sold as “tranq dope.” People who use drugs may not know xylazine is present because it has no distinct taste or smell, and standard street tests rarely detect it.
Dealers add xylazine for a few reasons:
- It can prolong the perceived effects of short‑acting fentanyl, stretching the product.
- It is inexpensive and easy to source compared with other cutting agents.
- It produces deep sedation that some people describe as “nodding,” which can be misinterpreted as stronger opioids.
Unlike opioids, xylazine does not respond to naloxone. But because it is so often combined with fentanyl, opioid toxicity is usually involved, and naloxone remains essential in a suspected overdose.
Xylazine acts primarily as an alpha‑2 adrenergic agonist. In animals and in humans who are exposed, it causes CNS depression, low blood pressure, and a slow heart rate. It also appears to reduce blood flow in small vessels and slow wound healing, which helps explain the severe skin ulcers people report, even when they do not inject into those areas.
The term “tranq” can sound casual, but the risks are not. Tranq‑contaminated fentanyl changes the overdose picture, the wound picture, and day‑to‑day functioning. For people who already live with opioid use disorder, it adds a new layer of complexity to safety and to recovery planning.
Prevalence and Supply
Xylazine has rapidly spread across the U.S. drug supply. Public health agencies and law enforcement first noted heavy presence in Puerto Rico and Philadelphia, then across the Mid‑Atlantic and New England. It is now detected in many regions, including the South and parts of the West, with ongoing increases in the Northeast and New Jersey.
Patterns in the current supply:
- Xylazine is commonly combined with illicitly manufactured fentanyl. That means overdose risk is compounded: strong opioid plus strong sedative.
- Detection in overdose deaths has climbed in multiple jurisdictions. Local trends can vary widely, but health departments and the DEA have issued alerts noting growth and geographic spread.
- Contamination is inconsistent. One bag may contain significant xylazine, while another from the same source may not. Users cannot tell by taste, smell, or color.
Because routine toxicology screens often miss xylazine, its true prevalence is likely higher than reported in clinical settings. Emergency departments and clinics in New Jersey and the broader Mid‑Atlantic increasingly encounter patients with the distinctive sedation pattern and hard‑to‑heal wounds that suggest exposure.
Community implications:
- People who use stimulants or non‑opioids primarily can be unintentionally exposed when supply chains cross‑contaminate.
- Overdose response strategies must adapt: always administer naloxone, then focus on airway and breathing because xylazine will not reverse with naloxone alone.
- Treatment providers should anticipate more complicated withdrawal and wound care needs during detox and early recovery.
For context on addiction itself, see an overview of what drug addiction is and how it affects decision‑making, tolerance, and risk.
Health Risks & Complications
The biggest dangers of xylazine‑contaminated supply come from combined depressant effects and from skin and soft‑tissue damage. The opioid‑xylazine mix can change how overdoses look and how to respond.
Major health risks:

- Respiratory and CNS depression: When xylazine is layered onto fentanyl, breathing slows further, responses are blunted, and arousal is more difficult. People may appear deeply unconscious for long periods.
- Hypotension and bradycardia: Low blood pressure and slow heart rate increase the risk of fainting, falls, and reduced organ perfusion.
- Complex wounds: People develop painful ulcers, necrotic tissue, black eschar, and slow healing. Wounds can appear on legs, arms, hands, or even areas away from injection sites.
- Infection risk: Cellulitis, abscesses, and systemic infections become more common due to impaired immunity, poor circulation, and exposure to environmental factors.
- Withdrawal and dependence: Frequent exposure can lead to xylazine dependence, layered on top of opioid dependence. Withdrawal may include anxiety, agitation, insomnia, tachycardia, hypertension, and strong cravings. There is no standardized medication protocol specific to xylazine, so care focuses on safety and symptom relief while stabilizing opioid use disorder with medications.
Why Wounds Occur
Several factors likely contribute:
- Vasoconstriction and microvascular injury reduce blood flow to skin and subcutaneous tissues.
- Sedation and unconsciousness lead to pressure injuries and forgotten site rotation.
- Acidic cuts and contaminants irritate tissues and cause repeated breaks in the skin.
- Repeated injections without time for healing, often without sterile supplies, promote bacterial and fungal infection.
- Poor pain and infection sensitivity while sedated, so damage progresses unnoticed.
Basic Wound‑Care Priorities
Core principles are not complicated, but they require consistency:

- Clean gently and regularly. Avoid harsh antiseptics that can delay healing; saline or clean water works for routine cleansing.
- Keep wounds moist, not wet, with plain petroleum jelly or a hydrogel to encourage new tissue growth. Dry scabs can trap infection and slow closure.
- Cover with clean, non‑adherent dressings. Change daily or as needed if soiled.
- Monitor for spreading redness, pus, fever, or severe pain. These are red flags for urgent care.
- Avoid injecting into or near wounds. If use is ongoing, rotate sites and consider safer options while accessing care.
Rolling Hills Recovery Center helps coordinate wound care with local clinicians while addressing substance use and withdrawal, so healing can begin even before someone has fully stopped using. Stabilization and safety come first, then longer‑term recovery work.
Overdose Response & Harm Reduction
Because tranq is usually mixed with fentanyl, treat any suspected overdose as an opioid overdose plus a sedative complication. The steps below can be taught to family, friends, and peers. Keep them simple and repeatable.
Overdose Response: What to Do Right Now
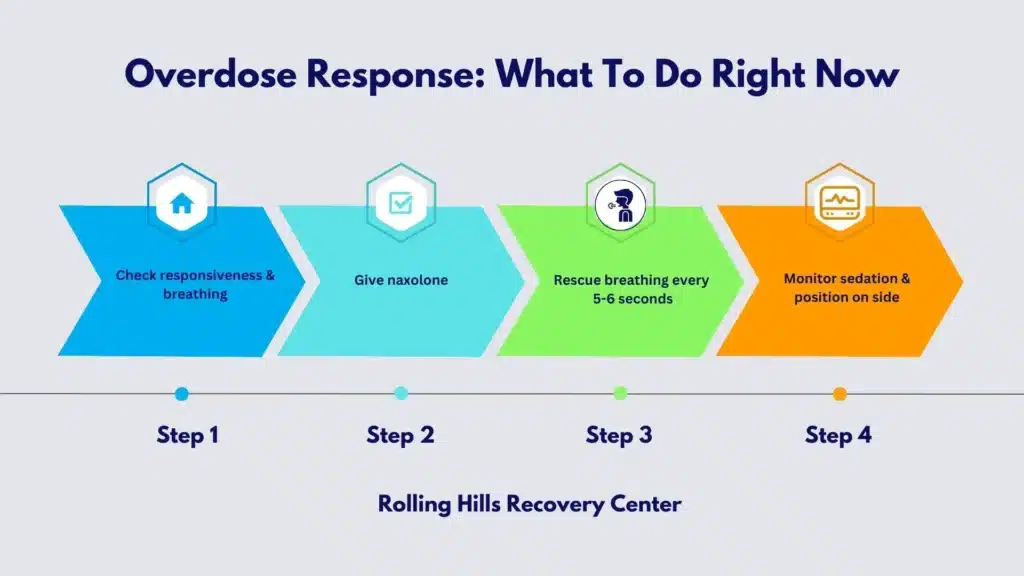
- Check responsiveness and breathing. If not breathing or very slow: call 911 immediately.
- Give naloxone. Use a nasal spray and repeat every 2–3 minutes if no response, up to the number of doses available.
- Start rescue breathing. If the person is not breathing adequately, give one breath every 5–6 seconds. Maintain an open airway, clear the mouth if needed, and use a face shield if available.
- Monitor and support. Even if the person wakes, they can slide back into sedation because xylazine will linger. Keep them on their side, warm, and supervised until EMS arrives.
Naloxone does not reverse xylazine, but it will counter the fentanyl. Oxygen and ventilation make the difference while waiting for help. Do not give more drugs or alcohol “to wake them up.” Avoid cold water or pain, it does not help and can harm.
Safer Use and Prevention Tips
- Never use alone. If using, have a partner present who knows how to respond or use a phone spotter service. Keep naloxone on hand.
- Test small amounts first. Potency and xylazine contamination are unpredictable. A small “test dose” can reduce risk.
- Carry naloxone and a basic wound kit. Include saline, clean gauze, petroleum jelly, and non‑stick dressings.
- Space doses and watch for heavy sedation. If unusually sedated after a small amount, stop and seek help; the supply may be heavily contaminated.
Wound Care Basics and When to Seek Urgent Care
- Wash hands, clean the wound with saline or clean water, apply petroleum jelly, then cover with a non‑stick pad and wrap lightly.
- Change daily or if wet/dirty. Do not pick scabs or scrape away healthy tissue; if black eschar is present, get clinical evaluation.
- Seek urgent care for fever, spreading redness, foul odor, severe pain, or if you can see a tendon, bone, or deep space.
- If antibiotics are prescribed, take the full course. Combine wound care with stabilization for opioid use disorder to promote healing.
Xylazine Test Strips: What They Can and Cannot Do
- Use strips cautiously on a small dissolved sample. Follow the manufacturer’s instructions closely.
- A positive result suggests xylazine is present. Treat the batch as high risk: use less, do not use alone, have naloxone and airway support ready.
- A negative result does not guarantee safety. Strips can miss low concentrations, and sample prep errors are common.
- Do not rely solely on strips to make dosing decisions. Combine with slower dosing and strong overdose precautions.
Simple tools help. A pocket response card with the 4 overdose steps, a small wound kit, and naloxone can save life and limb. Programs in New Jersey distribute these; treatment centers can help connect patients to supplies.
Below is a quick comparison to guide response thinking.
| Scenario | Typical features | Naloxone effect | Additional actions |
|---|---|---|---|
| Fentanyl only | Pinpoint pupils, slowed/paused breathing, unresponsive; response may require multiple naloxone doses | Usually effective when repeated and supported with breathing | Very deep sedation, snoring/gurgling, low blood pressure, and slow heart rate, prolonged drowsiness even after naloxone |
| Xylazine + fentanyl (tranq dope) | Reverses fentanyl component; partial arousal or improved breathing, but sedation persists | Airway support, EMS, and monitoring for cardiovascular depression | Keep airway open, rescue breathing, position on side, EMS evaluation for blood pressure/heart rate support |
| Xylazine only (rare) | Sedation, hypotension, bradycardia; may look alcohol‑like but deeper | Naloxone has no direct effect | Airway support, EMS, monitoring for cardiovascular depression |
Testing, Policy & Clinician Guidance
Routine hospital urine drug screens do not detect xylazine. Specialized toxicology or reference lab tests are required, and turnaround times can be slow. Clinicians should treat based on presentation, not wait for confirmation, especially when wounds or prolonged sedation suggest exposure.
Clinical points of care:
- Assume co‑exposure with fentanyl. Always administer naloxone for suspected overdose and prioritize airway management.
- Avoid stacking sedatives. Benzodiazepines and alcohol worsen respiratory depression; use only when clearly indicated and with monitoring.
- Manage hemodynamics. Hypotension and bradycardia from xylazine may respond to fluids and careful supportive care. Consult toxicology for severe cases.
- Plan for a layered withdrawal. Begin medications for opioid use disorder (MOUD) promptly for opioid dependence. Address xylazine‑related symptoms with supportive measures and close observation. Some clinicians consider alpha‑2 agonists for autonomic symptoms; approaches should be individualized and monitored.
Coordinating MOUD with Xylazine Management
Starting MOUD helps stabilize opioid use and reduces overdose risk even when the supply contains xylazine. Key considerations:
- Buprenorphine induction should account for fentanyl’s pharmacology. Micro‑induction can reduce precipitated withdrawal risk for some patients.
- Methadone may suit individuals with high opioid tolerance and heavy sedation patterns, provided monitoring is feasible.
- Naltrexone requires complete opioid detox and is generally not a first‑line choice in the context of heavy fentanyl exposure.
- Because xylazine prolongs sedation and complicates sleep, schedule check‑ins to assess daytime alertness and nighttime rest, and adjust the environment for safety if drowsiness persists.
A practical outpatient rhythm can include short, frequent visits for the first two weeks, wound checks, and a simple sleep and sedation log. Include rapid referral back to higher levels of care if hypoxia, uncontrolled infection, or severe withdrawal emerges.
Navigating Withdrawal and Sedation
There is no FDA‑approved medication specifically for xylazine withdrawal. Management focuses on stabilization and supportive care:
- Opioid withdrawal: treat with MOUD and adjuncts for nausea, diarrhea, insomnia, and pain.
- Xylazine‑related symptoms: manage anxiety, agitation, tachycardia, and hypertension with measured, individualized regimens. Avoid oversedation.
- Sleep and nutrition: sedation masks poor sleep architecture; simple, structured routines help. Basic protein and hydration support wound healing and energy.
- Mental health: depression and anxiety often worsen with irregular sleep and pain. Early behavioral health involvement improves engagement.
If heavy sedation persists days after cessation, reevaluate for co‑ingestants, liver and kidney function, and occult infection. Serial vitals and oxygen saturation checks can detect silent hypoxia.
Documentation, Coding, and Wound Care Integration
For clinicians:
- Document suspected xylazine exposure based on history and findings (prolonged sedation, characteristic wounds).
- Note that standard urine drug screens were negative for xylazine, and that diagnosis was clinical, pending any confirmatory lab results if obtained.
- Code wounds by location, size, depth, and presence of infection. Track weekly to show progress or need for escalation.
- Build a basic wound care pathway: cleanse, moist wound healing (petroleum jelly or hydrogel), non‑adherent dressing, compress for edema if appropriate, reassess in 3–7 days. Refer early for debridement if necrosis or undermining is present.
For patients who are not ready to stop using, harm reduction wound care is still valuable. Teaching how to clean and cover wounds, rotate sites, and avoid injecting into damaged tissue can prevent amputations and sepsis.
Policy and public health updates:
- The DEA issued a national alert in March 2023 about the widespread threat of fentanyl mixed with xylazine, urging naloxone carriage and heightened awareness.
- The FDA has taken action to restrict the illegal entry of xylazine into the U.S. to reduce diversion into the drug supply.
- CDC and NIDA continue to publish clinical guidance and surveillance summaries on xylazine’s spread and clinical management.
- States and localities, including those in the Mid‑Atlantic and New England, are expanding access to naloxone, wound care, and point‑of‑care education. New Jersey providers increasingly screen for xylazine exposure and offer MOUD with tailored support.
People often ask whether xylazine itself is addictive. Xylazine is not an opioid and does not produce a typical euphoria, but many develop dependence from repeated exposure because it alters sedation and autonomic function. Combined with fentanyl, it drives compulsive use cycles. As a broader context on drug reinforcement, see this overview of the most addictive drugs.
Useful References
CDC clinical guidance on xylazine: https://www.cdc.gov/overdose-prevention/media/pdfs/2024/07/Xylazine-Clinical-Management-and-Harm-Reduction.pdf
NIDA overview of xylazine in the drug supply: https://nida.nih.gov/research-topics/xylazine
DEA public safety alert on fentanyl mixed with xylazine: https://www.dea.gov/alert/dea-reports-widespread-threat-fentanyl-mixed-xylazine
FDA actions related to illegal xylazine importation and controls: https://www.fda.gov/news-events/press-announcements/fda-takes-action-restrict-unlawful-import-xylazine
Clinicians and community partners can review those resources for current recommendations. Rolling Hills Recovery Center incorporates these federal and public health guidelines into its protocols and coordinates care for patients in New Jersey who are navigating xylazine‑contaminated opioid exposure while building stability and recovery.
Conclusion
Xylazine (“tranq”) mixed with fentanyl raises overdose and severe wound risks. Remember: give naloxone, support breathing & call 911; seek early wound care; tests may miss xylazine.
Frequently Asked Questions (FAQs)
What is Tranq in the Current Drug Supply?
Tranq is the street name for xylazine, a veterinary sedative sometimes mixed into illicit fentanyl or heroin. It is not an opioid. Tranq deepens sedation and can slow breathing; people often do not know it is present. Because Tranq is frequently combined with fentanyl, the overall overdose risk goes up fast.
Does Naloxone Help During a Tranq Overdose?
Naloxone reverses opioids like fentanyl, but not Tranq (xylazine). Still, always give naloxone right away since opioids are usually involved. Then support breathing: open the airway, give rescue breaths, call 911. If there is no response, give another naloxone dose after 2–3 minutes. Stay until help arrives and monitor. Simple steps, big impact.
Why Does Tranq Cause Unusual Skin Wounds, and What Helps?
Tranq can reduce blood flow to skin and soft tissue, which raises the chance of ulcers, infections, and sometimes necrosis. Wounds may appear even away from the injection sites. Basic care includes gentle daily cleaning with saline, non‑stick dressings, keeping the area dry and covered, and not injecting through damaged skin. Seek medical care early for antibiotics or debridement if needed. Hydration and nutrition matter, too.
Can Tranq Be Found on Routine Drug Tests, and are There Test Strips?
Many routine toxicology screens do not include Tranq. Labs need to run a specific xylazine assay; ask the clinician or the lab directly. Xylazine test strips exist in some areas, but sensitivity varies, and results can be tricky. Use any strip info with caution, start with a smaller dose, never use alone, and carry naloxone and oxygen support if available.
How Does Rolling Hills Recovery Center Help People Affected by Tranq in New Jersey?
The team includes experienced professionals who understand fentanyl and Tranq exposure, and they coordinate care to address both substance use and the medical issues that come with it. Services may include thorough assessment, medication‑assisted treatment for opioid use disorder, trauma‑informed therapy, family support, relapse prevention, harm‑reduction education, plus wound care coordination with medical providers.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












