Seeking a chemical dependency evaluation near you can feel urgent and confusing. This brief, structured assessment, completed by licensed clinicians, clarifies substance use concerns, safety risks, and the right level of care.
Expect respectful questions, evidence-based screening tools, understanding addiction basics, and clear next steps, including withdrawal risk, co-occurring symptoms & practical recommendations tailored to New Jersey resources.
Key Takeaways
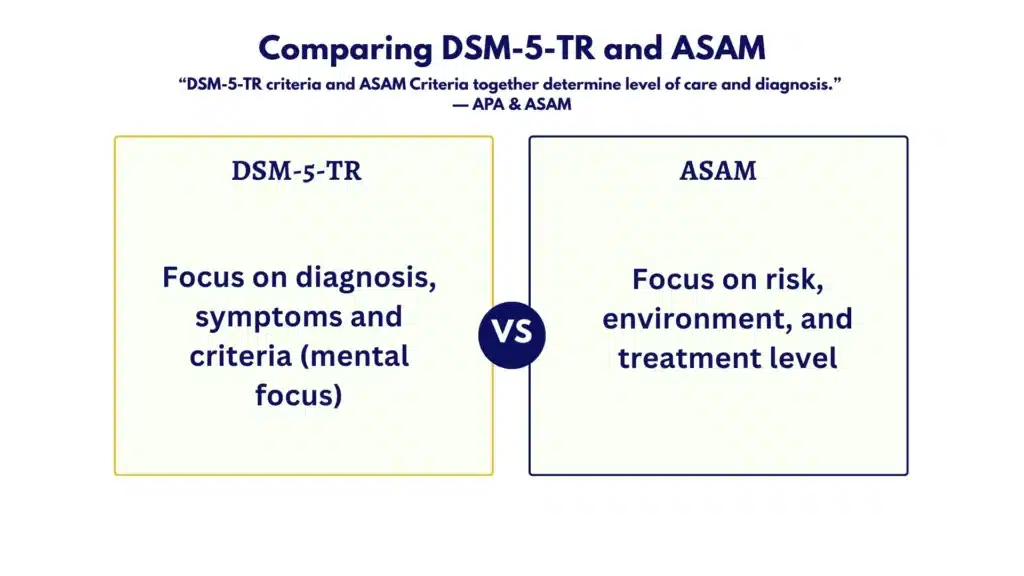
- A chemical dependency evaluation is a structured clinical assessment using DSM‑5‑TR & ASAM to confirm diagnosis, gauge severity, and match the safest level of care.
- Expect about 60–90 minutes: consent, medical and mental health history, substance timeline, withdrawal risk, and, when indicated, labs or tox; clear written recommendations follow.
- Preparation matters: bring ID, insurance, medication list, prior records & any legal paperwork; arrange safe transport if withdrawal is possible.
- Coverage is common in New Jersey; many plans and NJ FamilyCare/Medicaid cover initial evaluations, copays vary, telehealth is often okay; avoid “pass” guarantees or no listed credentials.
What “Chemical Dependency Evaluation Near Me” Means: Scope, Who Performs It, and Core Standards
A chemical dependency evaluation is a structured clinical assessment to confirm whether a substance use disorder (SUD) is present, how severe it is, and what risks or needs exist right now. It also identifies the most appropriate level of care using standardized criteria. The process is evidence‑based and time‑limited, typically 60–90 minutes, with space for additional collateral information if needed.
Who performs the evaluation?
- Physicians with addiction training (MD/DO), including those with board certification in Addiction Medicine or Psychiatry
- Licensed Clinical Social Workers (LCSW)
- Licensed Professional Counselors (LPC)
- Licensed/Certified Alcohol and Drug Counselors (LCADC/CADC)
- Nurse practitioners and physician assistants with SUD experience, where state scope allows
Core clinical standards used
- DSM‑5‑TR: Diagnostic criteria to determine SUD presence and severity (mild, moderate, severe)
- ASAM Criteria: Six assessment dimensions to determine level of care and placement
- 1: Acute intoxication and withdrawal potential
- 2: Biomedical conditions and complications
- 3: Emotional, behavioral, or cognitive conditions
- 4: Readiness to change
- 5: Relapse, continued use, or continued problem potential
- 6: Recovery and living environment
- Validated screening tools to support clinical judgment
- AUDIT (alcohol), DAST‑10 (drugs), ASSIST (alcohol, smoking, and substance involvement)
- PHQ‑9 (depression), GAD‑7 (anxiety) for co‑occurring symptoms
- When withdrawal is a concern: CIWA‑Ar (alcohol) or COWS (opioids)
What tools may be included
- Structured interview and symptom checklists
- Self‑report questionnaires
- Optional urine toxicology or breath alcohol testing when clinically indicated, and only with consent
- Optional labs (LFTs, CBC, pregnancy test) when medically relevant or requested
- Collateral information (with signed releases) from family, probation, employers, or medical providers
Privacy and consent
- HIPAA and, in many cases, 42 CFR Part 2 confidentiality rules apply
- Informed consent covers what information is collected, how it’s used, and to whom it may be disclosed
- Clear explanations of limits to confidentiality: threats to safety, suspected abuse, and court orders
Most relevant takeaways
- A qualified clinician uses DSM‑5‑TR to diagnose, the ASAM Criteria to match level of care, and standard tools to reduce bias
- The evaluation is collaborative; consent and privacy are front‑and‑center
- A same‑day summary and follow‑up plan are typical, especially when timely documentation is required
Rolling Hills Recovery Center in New Jersey follows these standards and combines evidence‑based treatment with whole‑person approaches. The team’s priority is accuracy, safety, and practical next steps that actually fit the person’s life.
What to Expect Step‑by‑Step
The flow may vary a little by clinic, but the steps below are consistent with best practice and New Jersey standards.
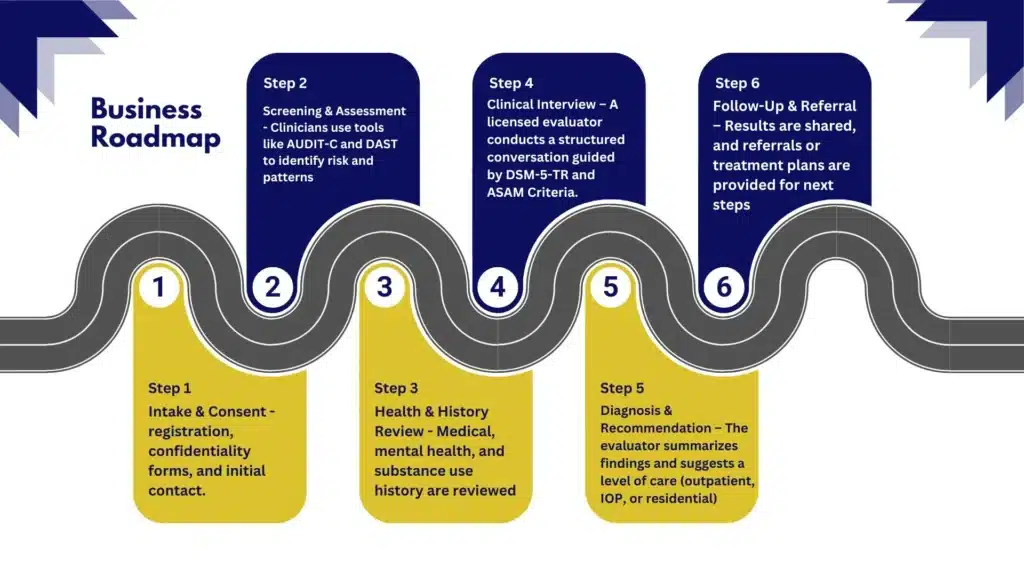
Step 1: Intake, Registration, and Consent
- Photo ID is verified, and basic demographics are collected
- Insurance details or self‑pay arrangements clarified
- Informed consent signed, including HIPAA acknowledgments and any releases of information (ROIs)
- Reason for the evaluation noted (self‑referral, family concern, legal/employer request)
Step 2: Immediate Safety and Withdrawal Check
- Screening for acute intoxication, suicidal ideation, or medical instability
- If sedative or alcohol withdrawal is possible, CIWA‑Ar screening is done; opioid withdrawal risk uses COWS
- If urgent medical needs exist, stabilization or referral for withdrawal management happens first; safe transport may be arranged
Step 3: Medical and Mental Health History
- Current conditions, medications, allergies, and past surgeries
- Past psychiatric diagnoses, symptoms, and hospitalizations
- Family history of SUD, mental health, and medical conditions
- For women of childbearing potential, pregnancy status may be discussed or tested with consent
Step 4: Substance Use Timeline
- What substances are used, how much, how often, how taken (oral, IV, smoked, snorted)
- Age of first use, longest abstinence, last use, and any prior treatment
- Episodes of overdose, blackouts, seizures, or delirium tremens
- Triggers and patterns (weekends, after work, with certain people)
- Consequences across work, school, family, legal, and health
Practical tip: Bringing a simple, handwritten timeline with dates, substances, quantities, and key events saves time and improves accuracy.
Step 5: Validated Screening Tools
- AUDIT, DAST‑10, or ASSIST completed and scored
- PHQ‑9 and GAD‑7 to screen for depression and anxiety; other brief screens if PTSD, ADHD, bipolar disorder, or other dual-diagnosis are suspected
- If nicotine use is present, a brief tobacco assessment helps integrate cessation or harm‑reduction options
Step 6: Physical Symptoms and Risk Assessment
- Sleep, appetite, pain, GI issues, and any infectious disease risks are reviewed
- Overdose history, access to naloxone, and safety in the home environment
- Access to firearms, domestic violence concerns, and transportation barriers
Step 7: Readiness to Change
- Motivation discussed openly: ambivalence is common
- Brief interventions like motivational interviewing can help identify a starting point, even if change feels far away
- Harm‑reduction and safety steps are offered when full abstinence isn’t the immediate goal
A helpful article that many clients review before or after the visit is the piece on whether drugs or alcohol are making day‑to‑day life unmanageable.
Step 8: Optional Urine Toxicology or Breath Alcohol Test
- Only performed with consent and when results will change clinical decisions or meet a legal requirement
- Testing methods and limitations are explained plainly
- Results are interpreted within context; false positives and detection windows are discussed when relevant
Step 9: Scoring and Clinical Formulation
- DSM‑5‑TR symptoms are checked systematically to determine SUD diagnosis and severity
- ASAM’s six dimensions are reviewed to understand risks, supports, and placement needs
- Co‑occurring mental health or medical issues are summarized
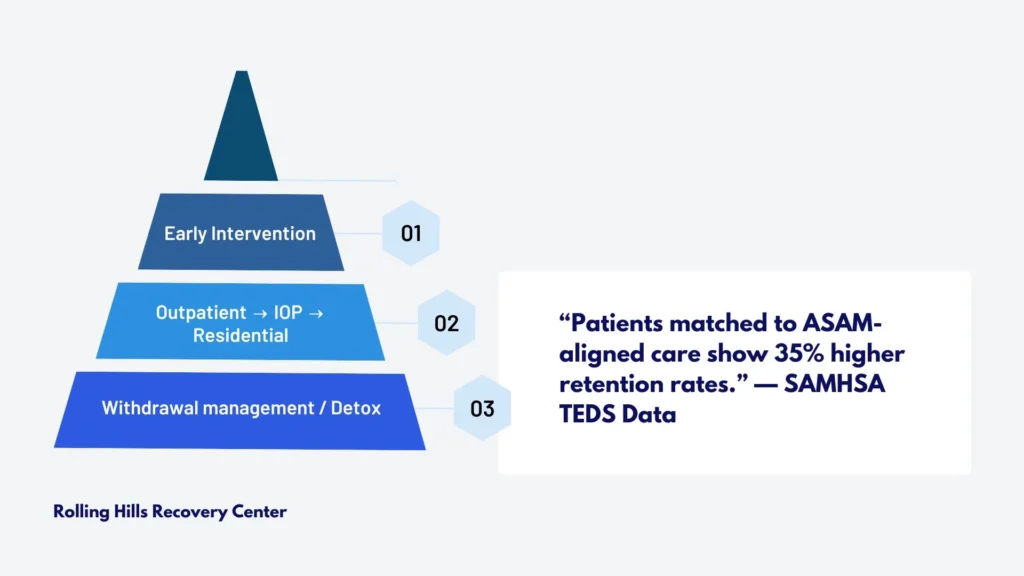
Step 10: Level‑of‑Care Match and Recommended Plan
- Early intervention/education, outpatient (1–9 hrs/wk), intensive outpatient (9–19+ hrs/wk), residential, or withdrawal management are considered
- FDA‑approved medications (for alcohol or opioid use disorders) are discussed when indicated
- Psychotherapy, peer support, family involvement, and case management are tailored to practical needs
Step 11: Same‑Day Summary and Documentation
- A brief written summary is typically provided the same day, with the full report soon after
- With signed ROIs, documentation can be sent to courts, employers, or referring providers
- Limits of confidentiality are restated, including what must be disclosed under the law
Step 12: Scheduling and Follow‑Up
- Near‑term appointments are set (medical visit for medications, therapy, group intake)
- A re‑assessment date is planned to track progress and adjust care
How to Prepare and What to Bring
Bringing the right items and details makes the evaluation smoother, especially when timelines are tight (court, work).
Bring these items
- Photo ID and insurance card (or self‑pay method)
- Medication list with doses; allergies written down
- Names and contact info for current providers
- Prior treatment records, discharge summaries, and toxicology results, if available
- Legal paperwork (DUI, probation requirements, employer letters)
- Emergency contacts
- A list of substances used, amounts, frequency, route, and last use date/time
- Questions about treatment options, goals, and concerns
If withdrawal is possible (alcohol, benzos, opioids), arrange safe transport. Avoid driving if impaired. If unsure whether medically supervised detox is needed, review local options and speak to a clinician.
For adolescents
- Involve parents or legal guardians; bring custody papers if relevant
- Age‑appropriate consent and privacy are reviewed so the teen understands what stays confidential and what does not
- School coordination happens only with guardian consent
Templates to help you prepare
- Medication and allergy list: name, dose, frequency, prescriber, pharmacy
- Substance timeline: date or period, substance, quantity, route, setting, consequences
- Questions to ask: therapy options, medication choices, expected time commitment, cost, transportation, evening/weekend sessions
Insurance, Cost, and Access in New Jersey
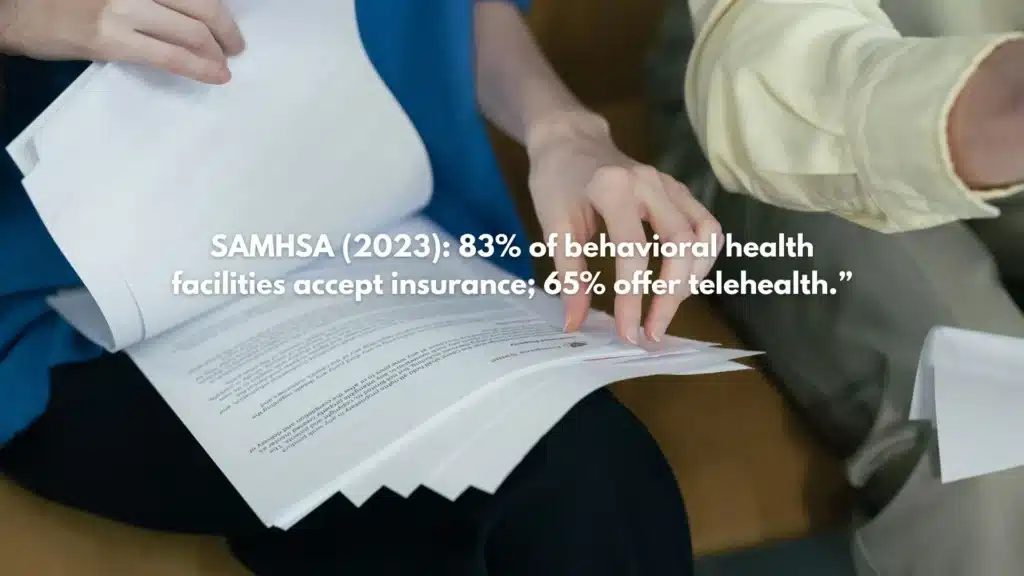
Most commercial plans and many Medicaid plans in New Jersey cover an initial behavioral health evaluation. Coverage specifics vary by plan.
Common billing codes
- 90791: Diagnostic evaluation (without medical services)
- 90792: Diagnostic evaluation with medical services (used by prescribers)
- H0001: Alcohol and/or drug assessment
What to expect financially
- Copays and deductibles vary; call the number on the back of the insurance card for behavioral health benefits
- Prior authorization is not usually required for the initial evaluation, though it may be required for certain levels of care afterward
- Self‑pay rates should be transparent and provided in writing; receipts are standard
Telehealth access
- Telehealth evaluations are often acceptable under New Jersey and plan rules, especially for follow‑up or non‑urgent needs
- Some legal or occupational cases still require in‑person identity verification or testing; ask upfront
Documentation for courts or employers
- When requested and with appropriate consent, a written summary can include DSM‑5‑TR diagnosis (if present), ASAM level recommendation, attendance, and testing results if performed
- Turnaround times can be expedited for DUI or mandated work cases; providing paperwork in advance helps
NJ Medicaid and parity protections
- Eligible NJ FamilyCare/Medicaid members have access to SUD evaluations and treatment; the state supports parity laws that require behavioral health coverage to be comparable to medical/surgical benefits
Red flags to avoid
- No credentials listed, or the evaluator cannot describe licensure
- Cash‑only with no receipts or itemized statements
- Promises to “pass” or “erase” an evaluation
- No mention of DSM‑5‑TR criteria, ASAM level‑of‑care, or HIPAA/42 CFR Part 2 processes
- Refusal to provide a written report upon request
Finding Qualified Help Near You (Without Confusion)
Selecting an evaluator is easier with a short checklist.
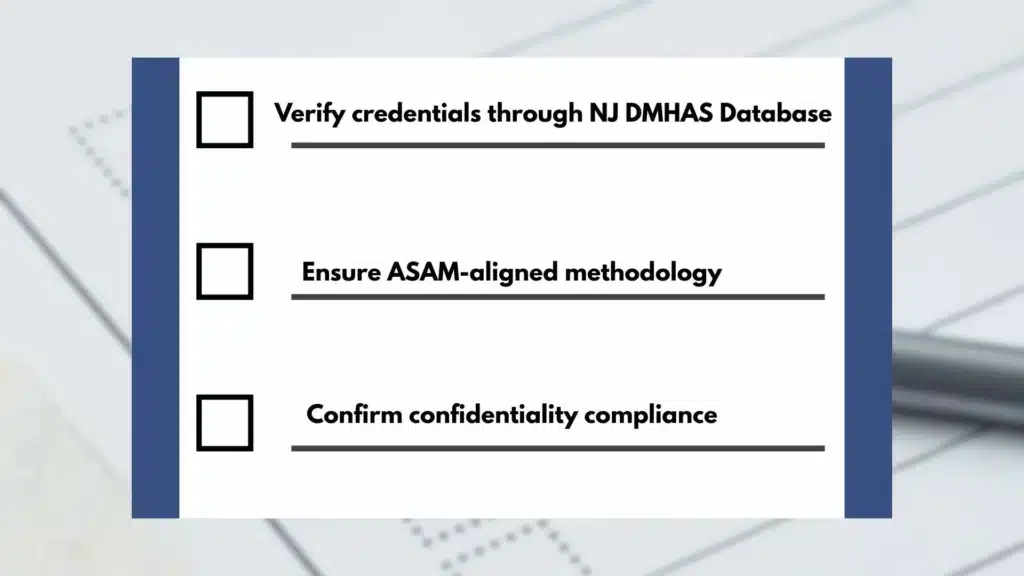
Verification and standards
- Confirm licensure: LCSW, LPC, LCADC/CADC, psychologist, physician, or qualified APN/PA
- Ask about ASAM‑informed practice and how DSM‑5‑TR is used to diagnose
- Confirm HIPAA and, when applicable, 42 CFR Part 2 protections
- Request a sample outline of the written evaluation to ensure it includes:
- DSM‑5‑TR diagnosis or “no diagnosis”
- ASAM six-dimensional summary and level‑of‑care recommendation
- Safety considerations and follow‑up plan
Releases and communication
- Expect clear ROIs for any third‑party communications; nothing should be sent without consent except where the law requires
- Ask how quickly the summary will be available if you have a deadline
In New Jersey
- The New Jersey Division of Mental Health and Addiction Services (DMHAS) offers statewide resources and consumer protections; credential status can be verified through state licensing boards
- Rolling Hills Recovery Center uses ASAM‑aligned evaluations and can coordinate next steps to outpatient, intensive outpatient, residential, or detox, depending on clinical need
Co‑occurring conditions matter
- If attention‑deficit/hyperactivity disorder or other conditions are suspected, make sure the evaluator can screen and coordinate care. More on this topic here: ADHD and addiction.
After the Evaluation: What Happens Next, Care Navigation & Follow‑Up
A good evaluation ends with a workable plan and a clear point of contact.
Levels of care and referrals
- Early intervention/education: Brief counseling, psychoeducation, and monitoring for those not meeting SUD criteria or with mild risk
- Outpatient services (Level 1): Individual and group therapy 1–9 hours weekly, relapse prevention, family work
- Intensive Outpatient/Partial Hospitalization (Level 2): 9–19+ hours weekly; structure for moderate to severe SUD with medical/psychiatric coordination
- Residential/Inpatient (Level 3): 24‑hour structure; indicated when outpatient settings aren’t safe or effective
- Withdrawal management (Level 1–4 WM): From ambulatory detox to medically supervised inpatient detox, depending on risk
Medication options, when indicated
- Alcohol use disorder: Naltrexone (oral or XR), acamprosate, disulfiram; discuss liver function and patient preference
- Opioid use disorder: Buprenorphine, methadone, extended‑release naltrexone; naloxone for overdose reversal
- Nicotine use disorder: Varenicline, bupropion SR, nicotine replacement therapy
- Co‑occurring mental health: SSRIs/SNRIs, mood stabilizers, or other treatments as appropriate
Psychosocial supports
- Cognitive‑behavioral therapy, contingency management, and relapse prevention skills
- Family sessions to improve communication and boundaries
- Peer recovery supports and mutual‑help options
- Case management for housing, transportation, ID replacement, or legal coordination
Safety planning
- Overdose prevention education and naloxone access
- Strategies to manage cravings, high‑risk people/places, and early warning signs
- Crisis contacts and after‑hours instructions
Care coordination
- With consent, the evaluator sends the report to the treating clinician(s)
- For those entering detox or residential care, handoffs include medication lists and recent labs if available
- Practical scheduling: evening or weekend groups, telehealth options, and transportation planning when needed
Re‑assessment and measurement‑based care
- Progress reviews at 30, 60, and 90 days (or sooner) to update ASAM dimensions
- Repeat brief screens (AUDIT‑C, GAD‑7, PHQ‑9) to measure symptom change
- Fluid step‑up or step‑down in care based on risk and function
Work and legal considerations
- If the evaluation is tied to employment or court, the plan will include objective attendance tracking, testing frequency if required, and timelines for progress reports
- Written updates are provided only with proper consent, while keeping clinical details appropriate to the audience
Holistic and whole‑person supports
- Nutrition, sleep, movement, and mindfulness approaches improve outcomes
- Trauma‑informed care respects past experiences and builds safety
- Cultural and spiritual preferences are incorporated whenever possible
Helpful References
- SAMHSA National Helpline: 1‑800‑662‑HELP (4357) for 24/7 confidential information and referrals. Online resource: SAMHSA National Helpline
- Levels of care and placement framework: American Society of Addiction Medicine (ASAM): The ASAM Criteria
- Diagnostic standards used in evaluations: American Psychiatric Association’s DSM‑5‑TR (Diagnostic and Statistical Manual of Mental Disorders, Text Revision)
- Validated screening instruments and practical tools for clinicians: NIDA: Screening and Assessment Tools
If there’s any uncertainty about withdrawal risk, placement level, or how to coordinate next steps quickly, contacting a program that provides both evaluation and treatment in one place can reduce delays and improve safety. Rolling Hills Recovery Center’s approach blends evidence‑based care and holistic supports so patients move from evaluation to action with less friction.
Conclusion
A chemical dependency evaluation clarifies needs, risks, and next steps. Key takeaways: know what to bring, expect respectful questions, and understand privacy & safety limits. Act early; honest screening leads to the right level of care in New Jersey. Call to schedule an evaluation and bring your records.
Frequently Asked Questions (FAQs)
What is a Chemical Dependency Evaluation Near Me?
A chemical dependency evaluation near me is a structured clinical assessment that checks for substance use problems, how severe they are, and any safety risks.
Licensed clinicians, such as physicians, nurse practitioners, LCSWs, LPCs, and LCADCs/CADCs, use DSM‑5‑TR criteria and the ASAM multidimensional framework to assess current use, withdrawal risks, medical and mental health needs, and readiness for change.
It helps match a person to the right level of care, from early intervention to outpatient, IOP, residential, or withdrawal management when needed.
What Happens During a Chemical Dependency Evaluation and How Long Does it Take?
Most evaluations take about 60–90 minutes. Expect consent and privacy review; medical and mental health history; a timeline of substance use (what, how much, last use); screening for depression and anxiety; a safety check; and sometimes a urine toxicology test. Clinicians often use brief tools like AUDIT, DAST, ASSIST, PHQ‑9, and GAD‑7.
Results are summarized the same day or within 24–48 hours, with a written report, DSM‑5‑TR diagnosis if present, and an ASAM level recommendation. No trick questions, just clear, respectful discussion.
What Should I Bring to a Chemical Dependency Evaluation, and Will it be Confidential?
Bring photo ID, insurance card, a list of medications and allergies, any prior treatment records, legal or job paperwork, and emergency contacts. If court or work sent you… bring the letter.
For teens, a parent or guardian usually participates. Your information is protected by HIPAA & state law. Limits to confidentiality are explained at the start (for example, immediate danger to self or others, suspected abuse, or specific court orders).
Ask for a copy of your consent and the final evaluation, and keep them for your records.
How Much Does a Chemical Dependency Evaluation Cost in New Jersey, and is it Covered?
Costs vary by setting and credentials. Common billing codes include 90791, 90792, and H0001. Many commercial plans and NJ FamilyCare/Medicaid cover a chemical dependency evaluation near me when medically necessary.
Telehealth is often allowed. Expect to pay a copay or coinsurance if applicable.
Red flags: no written report, cash‑only with no receipt, or anyone promising you will “pass.” If an employer, court, or DMV needs documentation, confirm the report will meet those requirements before the visit.
How Does Rolling Hills Recovery Center Handle a Chemical Dependency Evaluation?
Evaluations are performed by licensed clinicians using DSM‑5‑TR and ASAM criteria, with practical recommendations tailored to safety, medical, and mental health needs, and daily life.
Next steps may include outpatient therapy, IOP, recovery support, medications for alcohol or opioid use disorders when appropriate, and a clear follow‑up plan.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts