New Jersey residents deserve clear, medically accurate information about drug rehabilitation. This article explains evidence-based care across levels, medical detox, inpatient, PHP, IOP & outpatient, plus admissions, insurance, MAT options, and safety.
Readers will learn what to expect, how programs coordinate mental health support, and how aftercare strengthens recovery while honoring privacy, licensure, and patient rights.
Key Takeaways
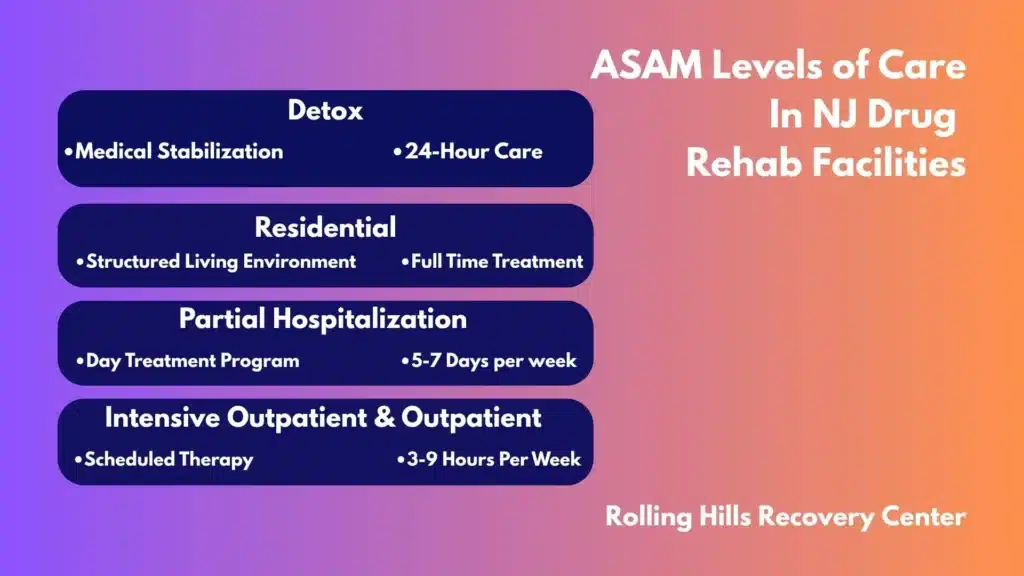
- Match the level of care to safety, withdrawal risk, and home support; options include detox, residential, PHP, IOP, and standard outpatient. Clinicians use the ASAM criteria to make that call.
- Care works best when it blends therapy & medications: CBT, motivational interviewing, and simple rewards‑based approaches; plus buprenorphine, methadone, or naltrexone when needed.
- Expect a clear intake: a brief phone screen, medical and mental health assessments, insurance verification, and a Good Faith Estimate; bring ID and a current medication list.
- Plan early for aftercare—relapse‑prevention skills, family involvement, steady refills, links to primary care and psychiatry, naloxone on hand, and 988 for crisis.
Overview of Drug Rehabilitation Facilities in New Jersey
Drug rehabilitation facilities in New Jersey deliver a continuum of care that ranges from medical detox to outpatient counseling.
The aim is clinical stabilization, reduction of harm, and long‑term recovery. Centers like Rolling Hills Recovery Center combine evidence‑based treatment with holistic supports to address body, mind, and social health.
What These Facilities Provide
- Medical detoxification (withdrawal management): 24/7 nursing, physician oversight, medication to manage withdrawal safely.
- Inpatient/residential: live‑in setting with structured therapy, medication management, and recovery skills.
- Partial hospitalization (PHP): full‑day programming, 5–7 days/week, patient sleeps at home or supportive housing.
- Intensive outpatient (IOP): 3–4 days/week, multiple therapy groups plus individual sessions.
- Standard outpatient (OP): 1–2 sessions/week for therapy, medication management, and relapse prevention.
- Recovery support: family education, peer services, case management, vocational or academic support, and alumni programs.
A concise comparison:
| Level of care | Typical setting | Medical monitoring | Time intensity | Common goals |
|---|---|---|---|---|
| Medical detox (3.7‑WM/4‑WM) | Inpatient unit | 24/7 | 3–10 days | Safe withdrawal & stabilization |
| Residential (3.1–3.7) | Live‑in facility | Daily/24‑hr depending on level | 2–6 weeks+ | Skill building, co‑occurring care |
| PHP (2.5) | Outpatient clinic | Daily medical availability | 20–30 hrs/week | Step‑down stabilization |
| IOP (2.1) | Outpatient clinic | Weekly medical visits | 9–19 hrs/week | Relapse prevention & therapy |
| OP (1.0) | Clinic/telehealth | As needed | 1–8 hrs/week | Maintenance & recovery coaching |
New Jersey facilities are expected to use evidence‑based practices (e.g., CBT, motivational interviewing, contingency management), include dual‑diagnosis capability for co‑occurring mental health disorders, and operate with a trauma‑informed approach.
These standards align with national guidance from NIDA and the ASAM Criteria.
Dual‑Diagnosis and Trauma‑Informed Care
Co‑occurring disorders, such as depression, PTSD, anxiety, and bipolar disorder, are common. Programs should be staffed by clinicians trained to assess and treat both conditions in parallel. Trauma‑informed care emphasizes safety, choice, collaboration, trust, and empowerment. That means:

- Screening for trauma and PTSD
- Offering evidence‑based trauma therapies when appropriate
- Avoiding coercion, shaming, or punitive approaches
- Building coping skills for sleep, anxiety, and mood
Accreditation and Licensure in NJ
In New Jersey, substance use disorder (SUD) programs must be licensed by the Division of Mental Health and Addiction Services (DMHAS). Residential programs fall under N.J.A.C. 10:161A; outpatient programs under N.J.A.C. 10:161B.
Many high‑quality facilities also hold national accreditation through The Joint Commission’s Behavioral Health Care and Human Services program or CARF.
Accreditation indicates independent review of clinical quality and safety.
Check state licensing information via New Jersey DMHAS and quality benchmarks through The Joint Commission Behavioral Health Care Accreditation.
Privacy and Patient Rights
Rehabilitation facilities follow HIPAA & 42 CFR Part 2 confidentiality requirements. Patients can expect:
- Informed consent for treatment and medications
- Confidential records with limited disclosure
- Access to one’s own medical record
- A written patient rights statement
- Respectful, non‑discriminatory care
- Grievance processes that are transparent and timely
For those wondering how addiction is defined and diagnosed, see the overview of what drug addiction is.
Admissions, Assessment, and Cost
Step‑by‑Step Admissions
- Initial call or online inquiry
- Brief screening: substances used, last use, medical risks, and insurance type.
- Safety check: suicidal ideation, overdose risk, and domestic violence risks.
- Insurance verification and benefits check
- Collect insurance card, date of birth, and address.
- Confirm deductibles, co‑pays, out‑of‑pocket maximums, and preauthorization rules.
- Pre‑admission clinical triage
- Review withdrawal risk, medical comorbidities, and psychiatric history.
- Determine if detox is indicated; if urgent, coordinate same‑day or next‑day admission.
- Scheduling and logistics
- Provide packing list, arrival time, and medication list from current prescribers.
- Obtain releases so the team can coordinate with primary care and psychiatrists.
- On‑arrival evaluation
- Medical and psychiatric assessments, toxicology screen, pregnancy test when indicated.
- ASAM level‑of‑care placement, safety plan, and initial treatment plan.
What to have ready:
- Photo ID, insurance card
- A 30‑day supply of current meds in original bottles, or prescriber info
- Names of emergency contacts
- Any recent labs or hospital discharge paperwork
Medical and Psychiatric Evaluation with ASAM Placement
Clinicians use the ASAM multidimensional assessment to match care intensity to need across six dimensions (acute intoxication/withdrawal, biomedical, emotional/behavioral, readiness to change, relapse potential, recovery environment).
In New Jersey, ASAM‑based placement is standard practice for level‑of‑care determinations.
Medication‑Assisted Treatment Options (MAT/MOUD)
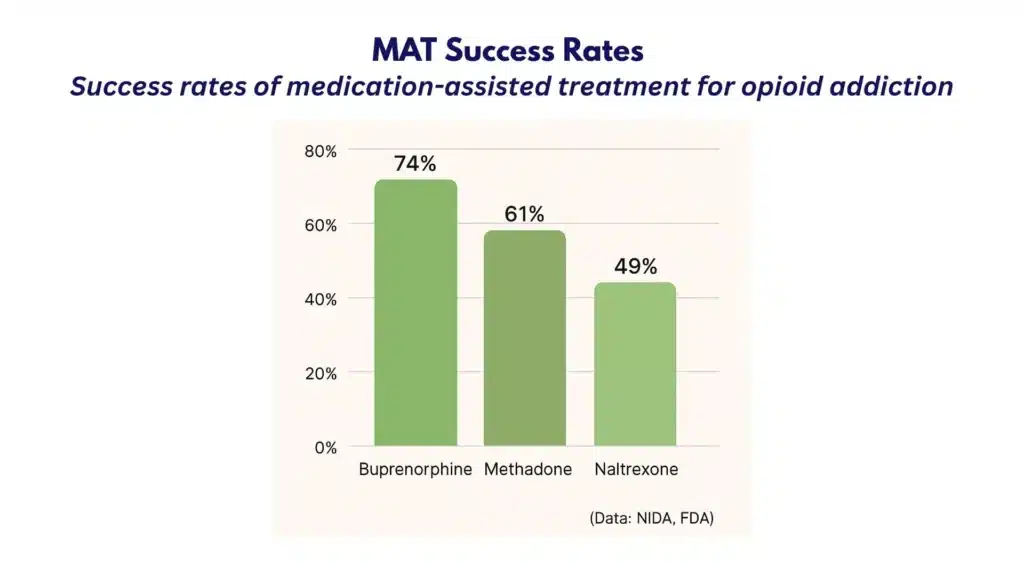
Evidence supports medications for opioid use disorder and alcohol use disorder. Common options include:
| Medication | Primary use | How it helps | Setting | Notes |
|---|---|---|---|---|
| Buprenorphine | Opioid use disorder | Reduces withdrawal & cravings | Office‑based/Outpatient | Partial agonist; can start after mild‑moderate withdrawal |
| Methadone | Opioid use disorder | Prevents withdrawal, stabilizes | OTP clinic (daily dosing initially) | Full agonist; highly regulated |
| Naltrexone (oral/extended‑release) | Opioid & alcohol use disorders | Blocks opioid effects; reduces alcohol craving | Outpatient | Requires opioid‑free period before start |
| Acamprosate | Alcohol use disorder | Supports abstinence maintenance | Outpatient | Dose adjustment for renal function |
| Disulfiram | Alcohol use disorder | Aversion approach with supervision | Outpatient | Requires adherence and medical oversight |
Medication is paired with therapy for the best outcomes. Discuss plan options openly; patients should understand risks, benefits, and alternatives.
Withdrawal Timelines (Typical Ranges; Vary by Person)
- Alcohol
- Onset: 6–12 hours after last drink (tremor, anxiety)
- Peak: 24–72 hours (blood pressure, tachycardia, agitation)
- Severe risks: seizures 12–48 hours; delirium tremens 48–96 hours, sometimes up to 5 days
- Short‑acting opioids (e.g., heroin, oxycodone)
- Onset: 8–24 hours
- Peak: 48–72 hours
- Duration: 4–10 days; post‑acute symptoms can persist
- Long‑acting opioids (e.g., methadone)
- Onset: 24–48 hours
- Duration: up to 10–20 days, sometimes longer
- Benzodiazepines
- Short‑acting onset: 1–2 days; long‑acting onset: 2–7 days
- Peak: 1–2 weeks; symptoms can linger for weeks
- Risks: seizures and rebound anxiety/insomnia; tapering is usually required
Any history of severe withdrawal, seizures, delirium, or major medical illness increases risk and may necessitate inpatient detox.
Insurance Verification and Good‑Faith Estimates
- Ask the facility to verify benefits and obtain prior authorization when required.
- Request a Good‑Faith Estimate (No Surprises Act) if uninsured or choosing self‑pay. This should list:
- Level of care and expected days
- Professional fees (physician, therapy), facility fees, labs, medications
- Potential extra costs (transportation, specialty consults)
- Clarify out‑of‑network policies, single case agreements, and payment plans.
- Keep written copies for your records & budgeting.
Simple cost worksheet template:
- Insurance plan/deductible/out‑of‑pocket max:
- In‑network? Y/N
- Preauthorization required? Y/N
- Estimated daily rate:
- Estimated length of stay:
- Medications/labs estimate:
- Patient responsibility estimate:
- Contact person for billing questions:
Family Involvement and Safety Planning
Facilities should offer:
- Family orientation and education on addiction science
- Structured family therapy or conjoint sessions
- Weekly updates (with consent)
- A written safety plan covering overdose risk, crisis steps, firearm safety, and domestic violence resources
- Parenting and caregiver supports when applicable
Practical Tools and Templates
- Pre‑admission checklist: ID, insurance card, medications, contact list, comfort items, weather‑appropriate clothes.
- Questions to ask insurance: in‑network status, authorizations, behavioral health carve‑out, telehealth coverage, out‑of‑network benefits.
- Release of information (ROI) list: primary care, psychiatrist, therapist, probation officer (if applicable), supportive family member.
- Personal goals sheet: “Top 3 concerns,” “Triggers I know,” “Supports I can call,” “Barriers to care (transport, child care).”
For educational clarity on diagnosis language, see drug dependence vs. drug addiction.
Care Delivery and Outcomes in Drug Rehabilitation Facilities
Day‑to‑Day Structure
Expect a mix of medical and therapeutic services:
- Physician or advanced practice clinician oversight at least weekly (more frequent in higher levels)
- Nursing checks: vitals, medication administration, withdrawal scoring
- Individual therapy: weekly or more often
- Group therapy: skills, relapse prevention, psychoeducation
- Family therapy: as indicated
- Case management: benefits, housing, employment, legal issues
- Recovery meetings/peer support
- Random toxicology testing for accountability and safety
Therapeutic approaches commonly include CBT, motivational interviewing (MI), contingency management, community reinforcement, and problem‑solving therapy.
For many patients, these are blended with holistic supports: sleep scheduling, nutrition support, exercise planning, mindfulness or yoga, and recreational therapy.
Culturally Responsive Care
Programs should tailor treatment to cultural background, gender, age, language, religion, sexual orientation, and military service. This can include:
- Individualized trauma screening for women, including safety planning for intimate partner violence
- Veteran‑informed care that addresses military stressors, MST, and moral injury; see options for drug rehab for veterans in NJ
- Language access and interpreters
- LGBTQ+ affirmative care and safe housing options
- Flexible family involvement that respects cultural roles
Co‑Occurring Disorder Treatment
Integrated care addresses both SUD and mental health simultaneously:
- Psychiatric evaluation and medication management (SSRIs/SNRIs, mood stabilizers, antipsychotics as needed)
- Evidence‑based therapies for mood and trauma (e.g., ACT, EMDR when appropriate)
- Suicide risk screening with ongoing monitoring
- Coordination with outside psychiatrists and therapists
Adjunct Wellness: Sleep, Nutrition, Exercise
- Sleep: establish a structured sleep window, limit caffeine late in the day, cognitive strategies for insomnia; medication only when indicated.
- Nutrition: hydration, balanced meals, repletion of vitamins (thiamine in alcohol use disorder), and registered dietitian input when available.
- Exercise: progressive plans that fit medical status; even brief daily walks improve mood and sleep.
Harm‑Reduction Education and Overdose Prevention
- Naloxone training and distribution, with education on fentanyl contamination and xylazine risks. Refer to CDC Overdose Prevention for up‑to‑date safety information.
- Linkage to syringe services programs where legal, and testing strips education where permitted.
- Education on safer use, never using alone, and tolerance changes after detox.
- Medication storage safety and childproofing.
What Realistic Outcomes Look Like (Not Hype)
Recovery is a process, and evidence shows success is multi‑dimensional. Validated measures include:
- Treatment engagement and retention (attendance, completion of phase goals)
- Reduction in substance use (self‑report corroborated by toxicology when appropriate)
- Health improvements (fewer ED visits/hospitalizations, stabilized chronic conditions)
- Functioning (employment/school participation, housing stability)
- Mental health symptoms (PHQ‑9, GAD‑7, PTSD checklists)
- Patient‑reported outcomes (Brief Addiction Monitor, craving scales, quality of life ratings)
Facilities should share aggregate outcomes transparently, with clear definitions and without “100% cure” claims. Readmission rates, follow‑up within 7–30 days, and medication continuity are useful program metrics.
Aftercare, Relapse Prevention, and Continuity
Discharge Planning
Discharge begins on day one and should culminate in a written plan that includes:
- Next level of care and appointment dates (e.g., step‑down to IOP then OP)
- Prescriptions and refills for MOUD or psychiatric meds
- Crisis and relapse prevention plan with triggers, early warning signs, and coping steps
- Releases of information for care coordination
- Transportation plan and backup options
Medication continuity matters. Missed doses of buprenorphine or methadone increase risk; ensure warm handoffs, bridge prescriptions when clinically appropriate, and OTP scheduling prior to discharge.
Recovery Capital Building
Recovery capital refers to internal and external resources that support sustained recovery:

- Health: primary care follow‑up, dental, vaccinations
- Home: safe, stable housing; consider recovery residences with oversight
- Purpose: work readiness, education, volunteering
- Community: positive relationships, family repair, mentorship
Case managers can connect patients to benefits, ID replacement, legal aid, vocational supports, and recovery‑friendly employers.
Peer Support and Community Resources That Don’t Replace Clinical Care
- 12‑step (AA/NA), SMART Recovery, Refuge Recovery, Women for Sobriety, Celebrate Recovery
- Peer recovery specialists and alumni networks
- Family supports: Al‑Anon, Nar‑Anon, SMART Family & Friends
- These enhance, but do not replace, medical or psychiatric care.
Access to naloxone should be standard. Encourage patients and families to carry it; many pharmacies in NJ can dispense without an individual prescription. In any mental health crisis, call or text 988 for immediate support.
Coordination with Primary Care and Psychiatry
- Send discharge summaries securely to primary care and mental health clinicians.
- Reconcile medications to minimize interactions and duplicate therapies.
- Agree on lab monitoring (e.g., liver enzymes for naltrexone, ECG if indicated).
- Plan follow‑up intervals and who manages which medications to avoid fragmentation.
- Use HIPAA‑compliant & 42 CFR Part 2‑compliant releases to enable needed communication.
Practical Aftercare Templates
- Weekly structure template: work/school blocks, therapy, peer meetings, exercise, sleep.
- Medication schedule card: medication name, dose, time, prescriber, pharmacy.
- Relapse prevention card: “My top 3 triggers,” “My top 5 coping tools,” “People I will call,” “Emergency steps.”
- Appointment tracker: date, provider, location/telehealth link, transportation plan.
Choosing High‑Quality Drug Rehabilitation Facilities Ethically in NJ
Selecting a program can feel rushed, especially during a crisis. A quick, ethical vetting process helps families decide safely.
Verify State Licensure and Survey History

- Confirm active licensure through New Jersey DMHAS.
- Ask the facility for the most recent state survey or accreditation report highlights.
- Clarify the licensed levels of care they actually provide onsite (e.g., 3.7‑WM detox, 3.5 residential, 2.1 IOP).
Look for Recognized Accreditation
- The Joint Commission Behavioral Health Care and Human Services accreditation (or CARF).
- Ask: Are outcome measures reported externally? Are staff trained in ASAM placement and trauma‑informed care?
- Review policies on adverse events, sentinel event reporting, and continuous quality improvement.
Trained Interdisciplinary Staff
- Board‑certified addiction medicine or psychiatry oversight
- Nurse coverage that matches the acuity (24/7 for detox/residential)
- Licensed therapists (LCSW, LPC, LMFT) trained in CBT/MI/CM, with supervision
- Peer recovery specialists with standardized training and supervision
- Dietitian, case manager, and family therapist availability
Reasonable caseloads matter. Ask for the average therapist caseload and the average group size.
Transparent Policies, Safe Prescribing, and HIPAA Compliance
- Written medication policies for MOUD, benzodiazepines, stimulants, and sleep aids
- Clear lab testing policies (what, how often, confirmatory testing)
- Privacy: HIPAA and 42 CFR Part 2 adherence, staff training, secure EHR, encrypted telehealth
- Emergency protocols: management of severe withdrawal, medical transfer pathways, naloxone on site, fire and disaster drills
- Access to on‑call medical providers after hours
Red Flags to Avoid
- Guaranteed cures or “100% success”
- Vague or shifting pricing; refusal to give a Good‑Faith Estimate
- Patient brokering, kickbacks, or cash payments for referrals
- No discussion of MAT or policies that ban MOUD across the board
- No individualized treatment plans (cookie‑cutter care)
- Pressure to travel unnecessarily long distances when local, appropriate care exists
- No licensed staff onsite for higher‑acuity levels
How to Evaluate Quickly: A Simple Checklist
- Licensure verified by DMHAS: Yes/No
- Accreditation (Joint Commission/CARF): Yes/No
- Offers MOUD for OUD and AUD: Yes/No
- Uses ASAM Criteria for placement: Yes/No
- Trauma‑informed training for staff: Yes/No
- Dual‑diagnosis services with psychiatric care: Yes/No
- Family therapy and education: Yes/No
- Transparent pricing with Good‑Faith Estimate: Yes/No
- Safety protocols (naloxone, transfer plans): Yes/No
- Reasonable caseloads/group sizes: Yes/No
Questions to Ask Admissions
- What levels of care are licensed at your location?
- How do you decide between residential, PHP, IOP, and OP for a new patient?
- Which evidence‑based therapies are core to your program?
- What are your policies on buprenorphine, methadone, and naltrexone?
- How do you manage severe alcohol or benzodiazepine withdrawal?
- What validated tools do you use to track outcomes?
- How soon after discharge will follow‑up appointments be scheduled?
- How do you involve families and loved ones (with consent)?
- What cultural or population‑specific services are available (e.g., women‑focused tracks, LGBTQ+ care, veteran‑informed services)? For women‑centered programming in New Jersey, see women’s drug rehab services.
- Can you provide a written Good‑Faith Estimate before admission?
Helpful References When Evaluating Practices and Standards
- National science on addiction and treatment: NIDA
- Level‑of‑care placement framework: ASAM Criteria
- Behavioral health accreditation standards: The Joint Commission Behavioral Health Care Accreditation
- New Jersey licensing and regulations: New Jersey DMHAS
- Overdose risks and naloxone education: CDC Overdose Prevention
Conclusion
Recovery works best with clear steps and safe care. Key points: matched levels of care, evidence‑based therapy, medication support, plus aftercare & family input. Next, verify insurance and schedule an assessment… ask questions.
Frequently Asked Questions (FAQs)
What Are Drug Rehabilitation Facilities, and How Do They Help?
Drug rehab facilities provide structured, licensed care for substance use disorders.
Care often includes medical detox for withdrawal safety, medication for addiction treatment (like buprenorphine or naltrexone), individual and group therapy, and family involvement.
Programs also assess mental health needs because anxiety, depression, or trauma can complicate recovery. A discharge plan with relapse prevention and aftercare is built from day one.
The aim is safe stabilization, skill building, and steady follow‑up… not quick fixes.
How Does Someone Choose the Right Level of Care at a Drug Rehabilitation Facility?
Match care to risk and support. Drug rehabs use clinical criteria (such as ASAM levels) to decide between detox, residential, partial hospitalization, intensive outpatient, or standard outpatient.
Key factors include withdrawal risk, cravings, co‑occurring mental health conditions, medical issues, home safety, and transportation.
If there’s a high relapse risk or unsafe housing, a higher level (detox or residential) is usually recommended. When symptoms are stable and home is supportive, intensive outpatient can work well.
What Happens During Admission at a Drug Rehabilitation Facility?
Admission to a drug rehabilitation program starts with a phone screening and insurance check, followed by an in‑person or telehealth assessment.
Clinicians review substance history, prior treatment, medical conditions, medications, mental health, and safety concerns.
Vitals and labs may be ordered to guide detox and medication decisions. Consent, privacy (HIPAA), and patient rights are explained before treatment starts.
An initial plan is created the same day, so care doesn’t stall; adjustments are made as symptoms change.
How Do Insurance and Costs Work at Drug Rehabilitation Facilities?
Most drug rehabilitation centers verify benefits, explain in‑network vs out‑of‑network coverage, and obtain any prior authorization.
Patients receive expected costs, co‑pays, deductibles, and a Good Faith Estimate when applicable. Billing teams often help with paperwork, short‑term disability or FMLA notes, and payment plans if needed.
Bring your insurance card and photo ID. If uninsured, ask about state resources or sliding scale options; waiting to ask can delay care.
What Sets Rolling Hills Recovery Center Apart Among Other Drug Rehabilitation Facilities in New Jersey?
Treatment plans may include medical detox placement, medication for addiction treatment, cognitive behavioral therapy, trauma‑informed care, and family sessions.
Treatment is tailored, re‑evaluated often, and linked to aftercare for continuity. This integrated model reflects what clinicians look for: safety, ethics, and outcomes that hold up over time.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts