A medical addiction specialist explains that heroin use disorder is a treatable medical condition. With fentanyl in the supply, quick, evidence-based care saves lives. This article walks through recognizing warning signs, starting medications like buprenorphine or methadone, choosing the right level of care, and steps to find help safely & fast near home.
Key Takeaways
- Heroin use disorder is medical and treatable; urgent safety steps matter now: carry naloxone, avoid using alone, call 911 for overdose signs.
- Medications for opioid use disorder (buprenorphine, methadone, and extended‑release naltrexone) cut cravings & overdose risk; pairing meds with counseling improves stability.
- Match level of care to need: medical detox for acute withdrawal, residential for higher risk, intensive outpatient or outpatient when stable supports exist; confirm MOUD access, privacy protections, and same‑day starts when possible.
- Practical basics help recovery stick: craving tools, sleep, nutrition, family involvement, a simple return‑to‑use plan, and regular follow‑ups with the care team.
Understanding Heroin Addiction and Urgency of Care
Heroin use disorder is a chronic medical condition where opioid use drives changes in brain reward, stress, and self-control systems. It becomes hard to stop even when someone wants to. Cravings, withdrawal, and tolerance keep the cycle going.
The information below leans on gold‑standard, peer‑reviewed guidance because local search results can be inconsistent. Core, evidence‑based sources include the National Institute on Drug Abuse (NIDA), the CDC, the FDA, the American Society of Addiction Medicine (ASAM), and the SAMHSA Treatment Locator.
What Heroin Use Disorder Looks Like
Signs often include strong cravings; using more or longer than intended; failed attempts to cut down; spending a lot of time getting or using heroin; neglecting work, school, or family; using despite health or legal issues; tolerance; and withdrawal when not using.
People may also switch to fentanyl‑containing supplies without knowing. In today’s drug supply, fentanyl is common and highly potent, which increases overdose risk (NIDA: Heroin).
Physical clues: small pupils, slowed breathing, constipation, drowsiness, track marks or skin infections, repeated “nodding off,” and reduced pain sensitivity. Psychological clues: anxiety, depression, irritability, and cognitive fog. Social clues: isolation, missed obligations, or risky behaviors.
Overdose Risks Today

Overdose occurs when opioids slow breathing so much that oxygen drops to dangerous levels. With fentanyl prevalent, overdose can happen faster and with smaller amounts. Combining opioids with benzodiazepines, alcohol, or other sedatives further increases risk.
Using alone, recent detox or incarceration (lost tolerance), and shifts in supply potency are high‑risk moments. Keep naloxone at home and where you spend time; train family or friends to use it. The CDC’s overdose prevention guidance is a trusted resource (CDC: Overdose Prevention).
Warning signs of overdose: very slow or stopped breathing, bluish lips or fingertips, pinpoint pupils, unresponsiveness, snoring or gurgling. Call 911, start rescue breathing if trained, and give naloxone.
Withdrawal Basics and Immediate Safety Plan
Opioid withdrawal is uncomfortable but usually not life‑threatening by itself. Common symptoms start 8–24 hours after last use (varies with fentanyl and method of use): muscle and bone aches, nausea, diarrhea, sweating, gooseflesh, yawning, anxiety, insomnia, chills, and dilated pupils. Risk spikes when people relapse after a short period off opioids, because tolerance drops.
A fast safety plan helps:
- Obtain naloxone and teach someone nearby how to use it.
- Avoid mixing opioids with sedatives or alcohol.
- If using, avoid using alone; consider a trusted check‑in or a virtual “spotter.”
- Hydrate, maintain electrolytes, and prepare for induction onto medications for opioid use disorder (MOUD) as soon as possible.
- Identify a local program that can start MOUD within hours to days.
For New Jersey residents, a facility like Rolling Hills Recovery Center can coordinate a same‑day assessment and discuss MOUD access, withdrawal support, and follow‑up therapy. If inpatient withdrawal support is needed, explore medical detox services near you.
Evidence‑Based Treatment Options Near Me
Medication is the first‑line treatment for opioid use disorder. The three FDA‑approved options for heroin or fentanyl‑pattern opioid use are methadone, buprenorphine, and extended‑release naltrexone (FDA: Medications for Opioid Use Disorder).
These work best when combined with counseling such as cognitive behavioral therapy (CBT) or contingency management (CM). ASAM’s national guideline supports this approach across settings (ASAM: National Practice Guideline).
Medications for Opioid Use Disorder (MOUD) as First‑Line
| Medication | How it works | Who it fits | When it starts | Common side effects | Important notes |
|---|---|---|---|---|---|
| Methadone | Full opioid agonist that stabilizes receptors and prevents withdrawal & cravings | People with severe OUD, high tolerance, prior buprenorphine non‑response, or who benefit from daily structure | Can start even if not in withdrawal | Nausea, fatigue, injection site reactions, and elevated liver enzymes | Dispensed at certified opioid treatment programs (OTP). Daily observed dosing early on. Reduces overdose and mortality. Avoid mixing with sedatives. |
| Buprenorphine (including buprenorphine/naloxone and monthly injection) | Partial agonist with ceiling effect; reduces withdrawal and cravings with lower overdose risk | Many with moderate to severe OUD who want office‑based or telehealth‑supported care | Constipation, sweating, sedation, and QT prolongation | Headache, constipation, sleep disturbance, nausea | Can be prescribed in office settings. Extended‑release formulations improve adherence. Strong safety profile. |
| Extended‑release naltrexone (XR‑NTX) | Opioid antagonist that blocks receptors; no opioid effects | People who are fully detoxed and prefer a non‑opioid option or have contraindications to agonists | Only after 7–10+ days opioid‑free (longer with fentanyl) | Nausea, fatigue, injection site reactions, elevated liver enzymes | Risk of precipitated withdrawal if not fully detoxed. Loss of tolerance increases overdose risk if opioids are used after stopping XR‑NTX. |
All three reduce illicit use and overdose risk when used correctly. The best choice depends on goals, stability, prior treatment response, and access. Methadone is highly effective but requires OTP attendance.
Buprenorphine offers flexibility and can often be started quickly in outpatient or telehealth models. Extended‑release naltrexone’s requirement of complete detox can be a barrier, but it is useful for some.

Why Combining Medication with Counseling Matters
Medication addresses withdrawal and cravings; therapy builds the skills to stay well. CBT targets triggers and thought patterns that lead to use. CM reinforces healthy behaviors with small, tangible rewards. Family‑based supports help rebuild trust and communication.
At Rolling Hills Recovery Center, therapy is delivered by trained clinicians using evidence‑based methods and, where helpful, holistic practices like mindfulness or movement. Medication plus therapy outperforms either alone in real‑world outcomes.
Why “Detox‑Only” Isn’t Enough
A short detox without ongoing MOUD is associated with a high risk of relapse and overdose because tolerance drops. The priority is not only to get through withdrawal, but to start and maintain MOUD rapidly with follow‑up counseling and recovery supports. Any detox plan should include a bridge to ongoing medication and therapy before discharge.
Harm Reduction Supports and Relapse Prevention
Keeping people alive is the first step in recovery. Practical supports include:
- Take‑home naloxone for the patient and family, with brief training.
- Fentanyl test strips, where lawful locally, are used to check drug supplies.
- Avoid using alone; if that’s not possible, arrange a check‑in.
- Never mix opioids with alcohol or benzodiazepines unless a prescriber carefully coordinates it.
- Sleep, nutrition, hydration, and regular medical care improve resilience and reduce triggers.
- A written return‑to‑use plan that includes who to call, where to go for same‑day buprenorphine or methadone intake, and steps to reduce risk.
Levels of Care and How to Choose Locally
Care should match medical and psychosocial needs, and it should be adjusted over time. ASAM’s level‑of‑care framework guides the match between symptom acuity, risk, and services.
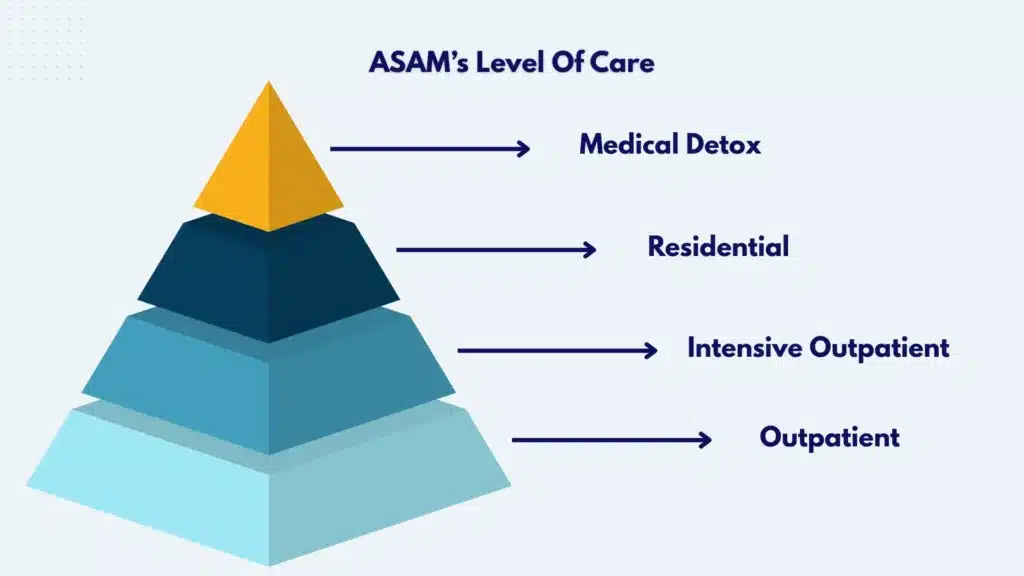
Matching Level of Care to Acuity
| Level of care | What it includes | Who benefits | Typical duration | MOUD availability |
|---|---|---|---|---|
| Medical detox (inpatient withdrawal management) | 24/7 nursing and medical oversight, symptom management, induction onto MOUD when possible | Severe withdrawal, polysubstance use with sedatives, medical or psychiatric instability, high overdose risk, unsafe housing | 3–7 days (varies) | Should initiate methadone or buprenorphine and connect to next‑step care |
| Residential treatment | 24‑hour structured setting, individual and group therapy, recovery coaching, relapse‑prevention skills | Those needing structure and safety without hospital level monitoring | 2–6+ weeks, individualized | MOUD should be continued onsite; verify capability |
| Intensive outpatient (IOP) | 9–15 hours/week of group + individual therapy, medication management | Moderate severity with stable housing and support | Weeks to months | MOUD management integrated |
| Standard outpatient | 1–8 hours/week therapy plus medication visits | Step‑down or stable recovery with ongoing monitoring | Ongoing | MOUD management and monitoring |
If withdrawal is the immediate problem, consider medical detox services near you. Many then step into residential or IOP, and later to outpatient.
Co‑Occurring Needs and Trauma‑Informed Care
Depression, anxiety, PTSD, ADHD, bipolar disorder, and personality disorders are common alongside heroin use. An integrated, trauma‑informed approach treats both addiction and mental health at the same time.
Ask programs how they assess and treat co‑occurring conditions and whether psychiatric medication management is available. For New Jersey residents, explore dual diagnosis treatment in NJ to understand how coordinated care works.
Practical Filters That Matter in New Jersey
- Verify licensure, accreditation, and the availability of MOUD. Ask directly: “Do you start methadone, buprenorphine, or XR‑naltrexone onsite?”
- Transportation and childcare can make or break attendance. Ask if programs offer or coordinate rides, telehealth groups, or evening hours.
- Insurance parity: Federal and NJ laws require parity for mental health and substance use care. If a plan denies a medically necessary level of care, request the medical necessity criteria and appeal. Ask programs for help navigating prior authorizations.
- Privacy: Your health information is protected by HIPAA and 42 CFR Part 2, which gives extra confidentiality to substance use treatment records. Written consent is needed before programs share your records, except in limited emergencies.
- Holistic supports: Mindfulness, exercise, nutrition counseling, and recovery coaching can help. These should complement, not replace, MOUD and therapy.
Rolling Hills Recovery Center offers evidence‑based and holistic approaches under one roof. For guidance on choosing the best addiction treatment in New Jersey, ask to speak with an admissions specialist who can map care to needs.
What the First 24–72 Hours Often Look Like
First day: Brief phone pre‑screen, insurance verification or self‑pay discussion, and scheduling of intake. On-site or telehealth intake includes medical history, substance use timeline, overdose history, psychiatric review, and labs, including urine toxicology.
If withdrawal is present and moderate, buprenorphine induction often starts the same day after assessing readiness; for methadone, OTP intake and initial dose are set up. Naloxone education is provided. Family or support persons can be engaged with consent.
Day two: Dose adjustments and symptom check; safety and coping planning; introduction to therapy schedule (group and individual); coordination with primary care for any medical concerns; medication reconciliation with a pharmacist when needed. If withdrawal is severe or complicated by sedatives, a short inpatient detox placement may occur before stepping down.
Day three: Stabilization continues. If buprenorphine is effective, dosing is fine‑tuned, for those pursuing XR‑naltrexone, detox planning and comfort medications are discussed, with a target start date after adequate opioid‑free days. A concrete aftercare schedule is set: therapy cadence, medication management cadence, and urine tox monitoring.
How to Find Help Near You Fast
Step 1 – Use the official SAMHSA Treatment Locator. Go to the SAMHSA Treatment Locator at https://findtreatment.gov. Enter your ZIP code. Filter for “Programs that offer medications” and specify “buprenorphine practitioners” or “Opioid Treatment Programs (methadone).” Sort by distance and call.
Step 2 – Confirm rapid access. Ask if they offer same‑day inductions or “bridge” prescriptions, evening/weekend intakes, and whether naloxone is provided. For methadone OTPs, ask about the next available intake slot and what to bring.
Step 3 – Coordinate with local care. If you have a primary care clinician or pharmacist, let them know you are starting MOUD so they can help with follow‑up, refills, and any drug interactions. Pharmacists can clarify dosing schedules and safety; they are an underused resource.
Step 4 – Consider telehealth adjuncts. Many providers offer telehealth for counseling and some medication follow‑ups. This can reduce transportation barriers and keep momentum.
Step 5 – Prepare essential documents and a safety plan. Bring ID, insurance card, a list of current medications, prior treatment records if available, and a contact for emergencies. Plan transportation and childcare. Keep naloxone at home and with a trusted person.
Sample call script to speed things up: “Hi, I’m looking for help with heroin use and would like to start medication as soon as possible. Do you offer same‑day buprenorphine or methadone intake? Do you take my insurance, and what will my out‑of‑pocket cost be? How often are counseling sessions? Do you provide naloxone and overdose education? Can you help with urine testing at intake and ongoing? If today isn’t possible, may I have a bridge plan or a telehealth option?”
If you prefer a program that integrates counseling with MOUD and holistic supports in New Jersey, call Rolling Hills Recovery Center admissions to discuss options and timing. They can explain how intake works, what the first sessions look like, and how the family can be involved with consent.
Provider questions checklist to use on calls:
- Do you start methadone, buprenorphine (including long‑acting injections), or extended‑release naltrexone onsite? What is your same‑day or 24‑hour access process?
- What does the first visit include (medical exam, urine tox, labs, overdose education)?
- How often are follow‑up visits and counseling sessions? Do you offer CBT or CM?
- Do you dispense or prescribe naloxone? Do you teach the family how to use it?
- Do you accept my insurance, and what are the estimated costs? What if prior authorization is required?
- Do you offer telehealth visits, evening/weekend hours, or transportation coordination?
- How do you handle co‑occurring mental health conditions? Is psychiatry available?
- How do you protect confidentiality under HIPAA and 42 CFR Part 2?
What to bring and a simple safety plan:
- Government ID, insurance card, medication list, allergies, and any recent labs
- Contact info for a support person; rides or a plan for transport
- Naloxone for home and a person trained to use it; avoid using alone; avoid mixing with alcohol or benzodiazepines
- A short list of triggers and coping strategies; who to call if cravings escalate
- A plan for next‑day follow‑up if same‑day induction isn’t available
Recovery Supports and Staying Well
Recovery begins with stabilization and extends into daily life. The goal is to make the healthiest choice the easiest one, most days.
Craving management
- MOUD is the most powerful craving reducer. Dose adjustments matter; speak up if cravings or withdrawal break through.
- Identify two or three high‑risk times of day. Place short, concrete actions there: call a peer, take a walk, do a 5‑minute breathing exercise, check in with a sponsor or coach, or join a brief online group.
- Keep fast supports close: water, light snacks, non‑sedating comfort meds if prescribed (like clonidine or ondansetron), and a written plan.
Naloxone in the home
- Everyone in the household should know where naloxone is and how to use it. Practice with a trainer device if available. Replace units before expiration.
Fentanyl test strips and safer‑use practices
- If the local laws allow, use fentanyl test strips before use. A positive result is a red flag for extreme risk. Even with a negative, assume variability in the supply.
- Never mix opioids with sedatives or alcohol. If a clinician prescribes a benzodiazepine for a medical reason, make sure all prescribers coordinate and review risks.
- Avoid using alone. If you must, arrange a live check‑in and keep naloxone within reach.
Sleep and nutrition basics
- Withdrawal disrupts sleep. Gentle routines help: consistent times, a dark room, no late caffeine, and light exercise during the day. Many find magnesium or non‑sedating sleep hygiene habits helpful; discuss any supplements with your clinician.
- Appetite can be poor early on. Small, protein‑rich meals, fluids with electrolytes, and fiber help manage constipation and fatigue common with opioids and MOUD.

Family involvement
- With consent, family can learn about OUD as a medical condition and what recovery looks like. Short, structured family sessions lower conflict and improve outcomes.
- Offer relatives clear roles: bring to appointments, store naloxone, attend an education session, or help with childcare on therapy days.
Return‑to‑use plan
- Because OUD is chronic, slips can happen. A written plan treats a return to use like a flare of asthma: promptly increase support without shame. Steps often include contacting the therapist the same day, scheduling an extra medication check, adding a group session, and reviewing high‑risk cues.
- Keep a list of same‑day options for buprenorphine induction or methadone OTP intake with hours, plus the nearest urgent care or ED for emergencies.
Milestones and monitoring
- Early stabilization: the first 2–4 weeks. Focus on consistent MOUD dosing, hydration, and sleep.
- Skill building: weeks 4–12. Practice CBT skills, relapse‑prevention plans, and family sessions as needed.
- Maintenance: months 3–12 and beyond. Cement routines, adjust medication as life changes, and monitor labs or urine tox as clinically indicated.
- Consider long‑acting formulations of buprenorphine if daily dosing becomes a burden.
- Periodically reassess goals. Some step down therapy frequency; some maintain a steady cadence to stay grounded.
Coordinating with medical care
- Primary care should remain involved for vaccinations, infection screening (HIV, hepatitis C), wound care, and general health. Pharmacists can review interactions and support adherence.
- If pregnancy is possible, discuss contraceptive options and the safety of methadone or buprenorphine during pregnancy. MOUD is considered standard of care in pregnancy (ASAM Guideline).
Rolling Hills Recovery Center’s team in New Jersey provides evidence‑based addiction treatment combined with holistic supports, delivered by experienced professionals. If heroin use is affecting life or safety, call for an assessment. Admissions can review insurance, arrange rapid intake, and map a plan for the first 72 hours and beyond.
Conclusion
Heroin addiction is urgent but treatable. Key takeaways: MOUD & counseling save lives, and the right level of care matters. Take basic safety steps, carry naloxone, and ask about same‑day induction. When ready, reach out. For compassionate, evidence-based care, contact Rolling Hills Recovery Center.
Frequently Asked Questions (FAQs)
What Does Heroin Addiction Treatment Usually Include, and How Fast Can it Start?
Treatment for heroin addiction typically begins with a same-day or next-day medical assessment & safety check. A clinician screens for overdose risk, withdrawal, other substance use, and mental health needs.
If withdrawal has started, buprenorphine induction can often begin within hours; methadone is started through an Opioid Treatment Program. Extended-release naltrexone is an option after full detox.
Care also includes naloxone for overdose reversal, counseling such as cognitive behavioral therapy, contingency management, and recovery planning.
Follow-ups are frequent at first, often 1–2 visits per week, and then taper as stability grows. In many places, telehealth may be used when allowed by law; either way, treatment aims to start quickly because time matters.
Which Medications Are Used in Heroin Addiction Treatment, and Are They Safe?
Medications for heroin addiction include buprenorphine, methadone, and extended-release naltrexone. Buprenorphine (a partial opioid agonist) eases withdrawal & cravings with a ceiling effect that lowers overdose risk. Methadone (a full agonist) is delivered in structured clinics and steadily controls symptoms.
Extended-release naltrexone (an antagonist) blocks opioid effects after detox. When prescribed and monitored, these medicines cut overdose death risk by half or more.
Common side effects can include constipation, mild nausea, or sleep changes. Mixing with alcohol and benzodiazepines raises risk, but treatment is not withheld; clinicians adjust dosing and monitor closely.
In pregnancy, methadone or buprenorphine is preferred; naltrexone is usually deferred. This is the medical standard for addiction treatment.
How Does Someone Choose the Right Level of Care for Heroin Addiction Treatment?
A medical specialist matches the level of care to the need. For treatment, outpatient or intensive outpatient works when withdrawal is manageable, housing is safe, and support is steady.
Residential treatment or hospital-based detox is considered for severe withdrawal, repeated overdose, unstable housing, pregnancy, or significant medical and mental health issues.
Always confirm the program offers medications for opioid use disorder, is properly licensed (for example, in New Jersey and other states), protects privacy under HIPAA and 42 CFR Part 2, and can coordinate counseling plus primary care. Ask about same-day buprenorphine starts, weekend access, transportation help, and insurance coverage.
A short phone screening can quickly point to the safest fit; it doesn’t have to be perfect on day one.
What Can Families Do Right Now While Arranging Heroin Addiction Treatment?
Keep naloxone on hand and learn how to use it. Avoid “cold-turkey” at home; instead, schedule a rapid medical visit for treatment. Stay with the person during early withdrawal when possible, encourage fluids, light food, and rest.
Use calm, nonjudgmental language; shame makes care harder. Secure medications and firearms, and remove obvious triggers in the home.
Write down current substances, doses, and prior treatments to bring to the first appointment. If laws allow, consider fentanyl test strips to lower overdose risk while waiting for care.
Plan safe transport, and if anxiety spikes, practice slow breathing together: small steps, steady safety.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












