Choosing an outpatient alcohol treatment program in NJ works best when symptoms are stable, supports are in place, and safety risks are low. From ASAM levels to medication options, this clinician overview clarifies who fits outpatient care, when to step up, what to expect session‑to‑session, and how to navigate coverage & logistics with confidence.

Key Takeaways
- Outpatient alcohol care in New Jersey fits people with safe housing, steady support, and low to moderate withdrawal risk. Red flags like seizure history, active self-harm, pregnancy complications, or unstable vitals point to detox or inpatient first.
- Clinicians match level of care (standard outpatient, IOP, secure telehealth) using ASAM dimensions. Expect CBT or MET, meds for AUD (naltrexone, acamprosate, disulfiram), random tox screens, family sessions, labs, with goals set for harm reduction or abstinence.
- Getting started means a confidential screen, medical check & withdrawal risk review, benefits verification, and scheduling that works with job or school. In New Jersey, verify state licensure, Joint Commission status, LCADC/LCSW/MD credentials, trauma-informed practice, and outcomes tracked.
- Plan for 12+ months of continuing care. Build recovery capital, housing, transport, peer support, and have a crisis plan, use digital tools, and coordinate primary care and psychiatry. Step up or down fast if risks rise; don’t wait.
Outpatient Treatment for Alcoholism in NJ: Who it Fits and When to Choose Higher Care
Defining Outpatient Levels Using ASAM Criteria
Outpatient alcohol care is not one thing. The American Society of Addiction Medicine (ASAM) defines levels that help clinicians match care to risk and need:
- Level 1: Standard Outpatient (OP). One to nine clinical hours weekly. Individual and group sessions, medication management, relapse-prevention work, and family sessions as needed. Can be in person or telehealth.
- Level 2.1: Intensive Outpatient Program (IOP). Nine to nineteen hours weekly, often three to five days per week in blocks. Adds more structure, skills groups, and close monitoring. Delivered in person or via secure video when appropriate.
- Telehealth is a delivery method, not its own level. Video visits can deliver Level 1 or Level 2.1 content if safety and privacy are assured and the ASAM dimensions support it.
In New Jersey, many people start at Level 1 or Level 2.1 based on the ASAM multidimensional assessment (acute intoxication/withdrawal potential, biomedical, emotional/behavioral, readiness to change, relapse potential, recovery environment).
Who Tends to Do Well in Outpatient Care in New Jersey
Outpatient fits adults who can stay safe at home, attend reliably, and avoid alcohol withdrawal complications. A few characteristics are typical:
- No current risk of severe withdrawal (no history of delirium tremens or seizures, and low CIWA-Ar scores).
- Stable housing and a sober or at least neutral environment.
- Some daily structure (work, school, caregiving) that becomes part of recovery goals rather than a conflict.
- Readiness to change that ranges from ambivalent to committed; motivational work happens in either case.
- Willingness to use medications for alcohol use disorder (AUD) when indicated and to complete lab monitoring.

Rolling Hills Recovery Center often sees commuters from across North and Central Jersey, union trades with early shifts, and caregivers juggling school pickups. Care plans are built around that reality instead of fighting it.
Clinical Red Flags That Point to Detox or Inpatient
Certain findings should trigger a higher level of care (ASAM 2.7–3.7 withdrawal management or residential):
- History of severe alcohol withdrawal, DTs, or withdrawal seizures; high daily intake with morning relief drinking.
- Active suicidality, homicidality, or psychosis; severe depression with intent.
- Unstable housing or no safe place to stay; domestic violence risk.
- Serious medical issues that alcohol worsens (decompensated liver disease, pancreatitis, uncontrolled diabetes), and pregnancy.
- Heavy co-use of benzodiazepines or other sedatives; recent head injury; cognitive impairment that limits outpatient safety.
If any are present, outpatient teams refer immediately to medically managed detox or inpatient stabilization. Stepping down comes later once the risk settles.
Practical NJ Factors: Commuting, Childcare, Insurance and Parity Protections
Commute and Scheduling in a Dense State
New Jersey traffic lives in calendars. Level 2.1 IOP can be scheduled early morning, lunchtime, or evening blocks to dodge turnpike bottlenecks and shift-work conflicts.
Telehealth groups help when weather or childcare falls apart on short notice. Programs should build makeup sessions into the week so one missed night does not become a lost week.
Childcare and Privacy at Home
Outpatient only works if patients can speak freely. Teams help set up a private space at home for telehealth, arrange earbuds, and use white noise.
Some patients bring a support person to the first visit to align family expectations. If childcare is a barrier, programs should help brainstorm swaps with family, school after-care, or community supports.
Insurance and Parity
The Mental Health Parity and Addiction Equity Act (MHPAEA) requires most plans to cover substance use treatment comparably to medical/surgical care. Insurers can still require prior authorization or use in-network providers, but they must apply rules fairly.
If coverage seems unfair, patients can ask the plan for the “nonquantitative treatment limitation” rationale in writing. The NJ Department of Banking and Insurance and the NJ Division of Mental Health and Addiction Services provide consumer help and state policy guidance.
Screening and Diagnosis: Quick Tools and Clinical Confirmation
Fast Screeners
Two simple options identify risk quickly:
- AUDIT (Alcohol Use Disorders Identification Test). Ten questions, scored 0–40; 8+ suggests hazardous use, higher scores point toward probable AUD. The CDC provides information and links to validated screening tools on its Alcohol Screening Module.
- Single-item screen: “How many times in the past year have you had 5 (men), or 4 (women), or more drinks in a day?” One or more is a positive screen warranting further assessment.
When screeners are positive, clinicians move to diagnostic criteria.
DSM-5 Criteria and Specifiers
AUD is diagnosed by the number of criteria met in the past 12 months (2–3 mild, 4–5 moderate, 6+ severe). Criteria include loss of control, time spent using, craving, role failures, hazardous use, tolerance, withdrawal, and more.
Severity and current withdrawal risk guide ASAM level of care. The diagnosis is confirmed in a structured interview, along with collateral when appropriate.
The Medical Evaluation
A brief medical workup supports safe outpatient care:
- Vital signs, CIWA-Ar if withdrawal is present; mental status.
- Labs: CBC, CMP with liver enzymes, GGT, sometimes CDT or PEth; pregnancy test when relevant.
- Medication review, including benzodiazepines or opioids.
- Safety screen: suicidality, violence risk, intimate partner violence.
- Social determinants: housing, transport, food security.
This is where New Jersey practicalities return; if labs or imaging are needed, programs coordinate close to home or work.
What to Expect Session-to-Session
Evidence-Based Therapies Used Routinely
Two cornerstones are common:
- Cognitive Behavioral Therapy (CBT): identifying triggers, thoughts, and patterns; practicing alternative skills; and small homework between sessions.
- Motivational Enhancement Therapy (MET): brief, structured sessions that explore ambivalence, clarify goals, and reinforce self-efficacy.
Other modalities are layered in: relapse-prevention skills, mindfulness, contingency management principles, Community Reinforcement Approach, and, when appropriate, Behavioral Couples Therapy or CRAFT to engage the family. Rolling Hills teams also integrate stress management and sleep coaching, because fatigue fuels relapse.
Medications for AUD with Medical Monitoring
Medication can double the odds of success for many patients. Typical options include:
- Naltrexone (oral daily or extended-release monthly injection): decreases heavy-drinking days and craving. Baseline and periodic liver function tests are needed.
- Acamprosate (three times daily): supports abstinence, especially after detox; renally cleared, so kidney function is checked.
- Disulfiram: creates an aversive reaction if alcohol is consumed. Works best with supervision and careful education.
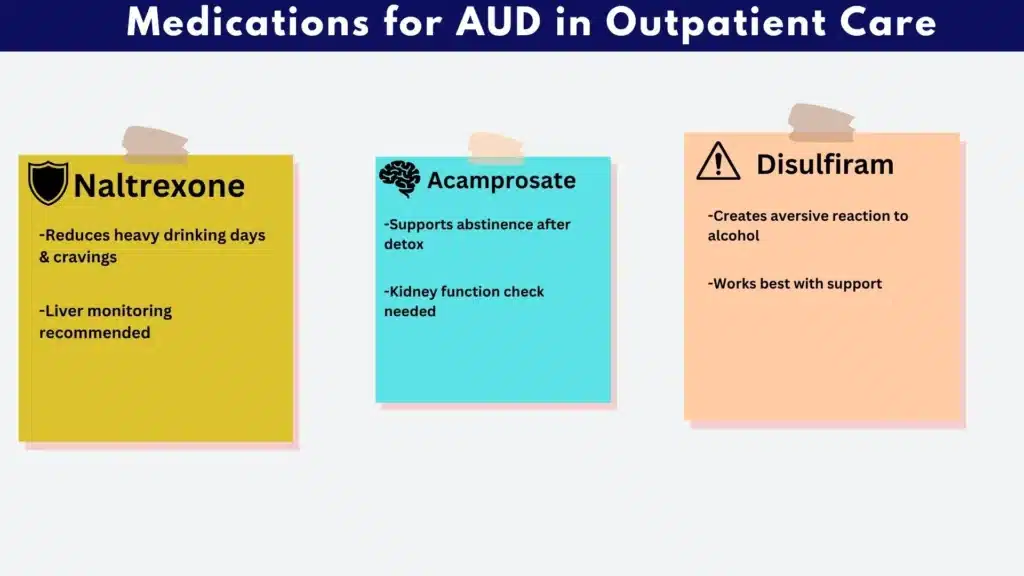
Off-label options (topiramate, gabapentin) are considered on a case-by-case basis. Medication decisions are made jointly, documented, and reviewed monthly. See an overview of approaches in medical treatment for alcoholism.
Frequency, Duration, Family Involvement, and Monitoring
Most outpatient episodes last three to twelve months. Early weeks may be 2–4 clinical hours weekly (Level 1) or 9–12 hours (Level 2.1). Frequency tapers with progress, but check-ins continue.
Random monitoring is part of care, not punishment: breath alcohol testing during visits, urine ethyl glucuronide/sulfate (EtG/EtS) for recent use, and sometimes PEth blood testing for longer windows. Results are used to adjust the plan and to keep everyone honest, kindly.
Family sessions are offered to reduce conflict, teach boundary setting, and coach loved ones on not reinforcing use. A short, scripted “supporter plan” is built so families know how to respond to risk days without panic.
Relapse Prevention Planning and Harm-Reduction Goals
Abstinence is often recommended for moderate to severe AUD, but harm-reduction goals can be appropriate, especially at the start: fewer heavy-drinking days, alcohol-free days scheduled each week, no drinking before work or driving. The plan is written, specific, and updated:
- High-risk map (places, times, moods).
- If-then coping plans (“If I get an urge after work, I text my counselor, walk 10 minutes, then ride home.”).
- Delay-and-distraction skills; urge surfing; breath work.
- A 72-hour stabilization plan after any alcohol use: safe sleep, hydration, food, medication check, notify team.
Integration with Primary Care and Psychiatry
Many patients arrive with depression, anxiety, ADHD, PTSD, or sleep disorders. Outpatient programs coordinate with primary care and psychiatry to align medications (for example, avoiding benzodiazepines when possible), monitor blood pressure and liver health, and treat co-occurring disorders alongside AUD. Consent forms make communication smooth and legal.
Adjusting Level of Care: Step Up, Step Down
Using ASAM Dimensions to Guide Changes
Care is dynamic. When cravings spike, stress rises, or life throws a curveball, programs can add evening groups, increase individual sessions, or step to IOP level temporarily. When stability holds for a month or two, frequency can taper. Decisions are anchored to ASAM’s six dimensions:
- Dimension 1 (withdrawal risk): any new morning shakes, sweats, nausea? If yes, pause and reassess.
- Dimension 2 (biomedical): rising liver enzymes or new pain may trigger medical consults.
- Dimension 3 (emotional/behavioral): worsening depression or trauma symptoms may require psychiatry or higher structure.
- Dimensions 4–6: motivation, relapse risk, and environment decide whether telehealth is enough or in-person is safer.
When Abstinence is Not the Immediate Goal
For some, a phased approach helps. The team might set a first-month plan of zero drinking on work nights, all alcohol off the property, medication daily, and one supportive meeting weekly. Data are reviewed weekly. If harm-reduction stalls or risks rise, the team revisits abstinence and higher care without judgment.
Getting Started: A Simple Step-by-Step
- Confidential screening. A 15–30 minute phone or video screen uses AUDIT, brief risk questions, and a review of current medications and safety.
- Medical evaluation. A clinician visit confirms DSM-5 criteria, orders labs if needed, and assesses withdrawal risk with CIWA-Ar.
- Withdrawal risk check. If any risk flags appear, an immediate referral to ambulatory or inpatient withdrawal management is made before outpatient treatment starts.
- Benefits verification and cost estimate. Insurance is verified, co-pays or deductibles explained in plain numbers, and options for payment plans or financial help are reviewed.
- Safety plan. A written plan includes crisis contacts, 24/7 helplines, and home-safety steps (remove alcohol, identify safe rooms and supporters).
- Scheduling that fits work and school. Sessions are placed into the weekly calendar; telehealth backup is arranged for predictable conflicts.
Patients can request a one-page “Employer Accommodation Letter” stating dates/times needed for treatment without revealing a diagnosis. Employers usually accept recurring medical appointment language.
Vetting Programs in NJ: A Quick Checklist
- NJ licensure and national accreditation. Ask for the current NJ DMHAS license and accreditation by The Joint Commission or CARF; verify on agency sites. NJ policy information is at the NJ Division of Mental Health and Addiction Services.
- Clinician credentials. Look for LCADC, LCSW, LPC, LMFT, psychologists, and physicians (MD/DO) experienced in AUD. Board-certified addiction medicine is a plus.
- Medication capability. The program should prescribe and manage AUD medications on-site or in tight collaboration with labs and liver monitoring in place.
- Trauma-informed, culturally responsive care. Private spaces, respectful language, options for gender-specific groups, and screening for trauma with appropriate therapies.
- Telehealth reliability. Encrypted platforms, tech support, and clear contingency plans if video fails mid-session.
- Outcome tracking. Programs should measure heavy-drinking days, retention, medication adherence, return to work/school, and hospitalizations; and share aggregate outcomes.
- Family engagement. Offer structured family sessions and education, not just ad hoc check-ins.
- Fit and accessibility. Evening/weekend options; parking or transit access; reasonable wait times. If driving is tough, consider hybrid schedules.
When comparing facilities, it helps to review how they integrate evidence-based care and holistic supports. A fuller overview of program elements is available at our alcoholism treatment facility page.
Know Your Protections at Work and with Insurance
FMLA, MHPAEA Parity, ADA, and Employer Paperwork
- FMLA. Eligible employees may take unpaid, job-protected leave for their own serious health condition, which can include treatment for AUD. Employers can request a medical certification that confirms the need for leave and duration; it does not have to list a diagnosis. Intermittent leave for recurring appointments is allowed when medically necessary. Employers may ask for a fitness-for-duty note to return to work if the policy applies equally to similar conditions.
- MHPAEA. Health plans that cover mental health and substance use disorders must apply treatment limitations (such as prior authorization or visit caps) no more restrictively than for medical/surgical conditions. Patients can ask insurers for the plan’s parity analyses for nonquantitative limits.
- ADA. Individuals in recovery not currently engaged in illegal drug use may have protections under the Americans with Disabilities Act. Employers must provide reasonable accommodations unless they cause undue hardship.
- Confidentiality. Substance use disorder records are protected by HIPAA and, in many cases, 42 CFR Part 2. Employers should not receive treatment details beyond scheduling and fitness-for-duty statements.
If disputes arise, patients can speak to the plan’s member services, the employer’s HR or EAP, or seek help from state regulators. Keep copies of all letters and forms.
Aftercare That Sticks: Continuing Care for 12+ Months
Longer-term support keeps gains. It is less about intensity and more about rhythm: brief check-ins, data review, and fast response to risk. Many patients continue with monthly individual therapy, medication follow-up, and low-burden group support for a year.
A simple “Recovery Continuity Plan” is written before discharge from IOP or weekly OP. It includes:

- Recovery capital supports: stable housing, backup childcare, transportation, and at least two reliable peers or mentors. Programs help map public transit routes or carpool plans when driving is shaky.
- Crisis plan: who to call (by name), 24/7 helplines, nearest urgent care and ER, and steps to remove alcohol from the home during a flare.
- Digital supports: secure messaging with the care team; a daily check-in via text or app for mood/craving; calendar reminders for medication and labs; optional breathalyzer with Bluetooth logging if chosen.
- Family education: short modules on boundaries, substance-free home routines, and how to respond to slips without shaming.
- Alcohol-related health monitoring: periodic liver enzymes, blood pressure checks, nutrition counseling, and sleep assessments. Primary care is looped in with consent.
Patients who prefer community recovery supports can choose among options without pressure, mutual-help groups, faith-based communities, or secular groups. The NIAAA Alcohol Treatment Navigator explains evidence-based options and offers worksheets to compare local care.
Finding Help Now: Navigation and Helplines in NJ
New Jersey maintains statewide navigation so people do not get stuck:
- ReachNJ: 1-844-732-2465 (24/7). Live connection to treatment navigation across NJ.
- NJ Division of Mental Health and Addiction Services: policy updates, licensure info, and links to county services at NJ Division of Mental Health and Addiction Services.
- SAMHSA: national 24/7 helpline at 1-800-662-HELP (4357) and a searchable directory at SAMHSA’s Treatment Locator.
For understanding treatment quality and how to vet options, the NIAAA Alcohol Treatment Navigator offers plain-language guidance and checklists. The ASAM Criteria explain how clinicians determine the level of care in a consistent way.
For those who prefer to begin with a local, flexible program that combines evidence-based care with whole-person supports, medications, therapy, and practical problem-solving, Rolling Hills Recovery Center offers outpatient and IOP options across New Jersey, with hybrid scheduling when needed.
More on program structure and medical services is available in our article about outpatient alcohol rehab centers in NJ.
Conclusion
Outpatient alcohol care in NJ works when symptoms are stable, support is steady, and safety is clear. Key points: match ASAM level, use therapy plus meds, plan costs & scheduling. Step up if withdrawal risks or unstable housing appear. Next, book a confidential assessment and verify benefits.
See how Rolling Hills Recovery Center, a New Jersey rehab offering evidence-based and holistic care with experienced clinicians, can help you.
Frequently Asked Questions (FAQs)
What is Outpatient Treatment for Alcoholism in New Jersey, and Who Benefits?
Outpatient treatment for alcoholism in New Jersey is structured, evidence-based care delivered without an overnight stay. It suits individuals with stable housing, reliable transportation, and manageable withdrawal risk.
Care may include weekly therapy (often 1–3 visits), medication management, and family involvement. Those with strong support, steady medical conditions, and low immediate safety concerns often do well.
Suppose past alcohol withdrawal was severe, or there is suicidality, pregnancy with complications, or unstable housing. In that case, clinicians advise higher care first, then step down to outpatient treatment once safe.
How Does Outpatient Treatment for Alcoholism Work Week to Week in NJ?
Outpatient treatment for alcoholism in NJ blends therapy and medications with practical relapse-prevention. Clinicians use cognitive behavioral therapy (CBT), motivational enhancement, and trauma-informed approaches.
Medications like naltrexone, acamprosate, or disulfiram can reduce craving or support abstinence; labs and brief medical checks maintain safety.
Visits occur in person or via secure telehealth, often 1–3 times weekly at first, then taper. Random toxicology screens, skill building, and family sessions are common.
Plans are flexible around work & school, but remain structured. Goals are reviewed often, and adjustments are made quickly if symptoms change.
When is Outpatient Treatment for Alcoholism Not Enough, and What Are the Red Flags in NJ?
Outpatient treatment is not enough when safety is uncertain. Red flags include a history of severe withdrawal (seizures, delirium), current high blood alcohol with vital sign instability, active suicidality or self-harm risk, uncontrolled medical illness, pregnancy with risk, and lack of safe housing.
In these cases, clinicians in NJ step up care for medical detox or inpatient stabilization first, then return to an outpatient program as soon as medically appropriate. A rapid evaluation, a clear safety plan, and close follow-up limit risk and reduce gaps in care.
Can Outpatient Treatment for Alcoholism Support Co-Occurring Mental Health Needs and Busy Schedules in NJ?
Yes. Outpatient treatment for alcoholism in NJ commonly integrates care for depression, anxiety, PTSD, ADHD, and other conditions.
Psychiatric evaluation, medication coordination, and therapy address both alcohol use and mental health at the same time.
Scheduling is made to fit work and family duties; early morning, evening, or telehealth blocks are typical. Employers may accept medical leave under FMLA, and parity laws help with coverage.
The approach is flexible but not loose; if symptoms escalate, clinicians step up intensity, then step down once stable. Simple, practical, and accountable.
How Does Rolling Hills Recovery Center Deliver Outpatient Treatment for Alcoholism in NJ?
Treatment plans for outpatient typically include CBT-driven therapy, medication options such as naltrexone or acamprosate, family education, and coordinated medical monitoring.
The team emphasizes measurable goals, compassionate support, and smooth transitions, stepping up if risks appear, and stepping down as recovery strengthens.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts












