Choosing a doctor who treats addiction in New Jersey is a medical decision that deserves clear, reliable facts. This article explains what these physicians do, how care is tailored, and what to expect at the first visit, so patients and families can move forward with confidence and safety while respecting privacy and long-term recovery goals.

Key Takeaways
- Verify credentials in New Jersey: active NJ medical license, board certification in Addiction Medicine or Addiction Psychiatry, and current DEA registration; safe prescribing with PDMP checks matters.
- Effective care uses medications and therapy together, such as buprenorphine, methadone, or naltrexone, with CBT, motivational interviewing, and relapse prevention. Plans are individualized, not one-size-fits-all.
- Know what to expect at intake & after: bring ID, insurance, medication list, and prior records; assessment follows DSM‑5 criteria, screens for co‑occurring conditions, sets level of care, and outlines follow‑up.
- Practical fit counts: confirm insurance coverage, wait times, coordination with primary care and psychiatry, plus privacy and clear outcomes tracking; watch for guarantees or quick fixes.
Scope of Addiction Treatment Doctors in New Jersey
Roles Across Evaluation, Diagnosis, and Longitudinal Care
Addiction treatment doctors in New Jersey evaluate, diagnose, treat, and follow patients over time, often across different levels of care.
The evaluation typically includes a focused medical history, substance use history, mental health screening, physical exam when needed, and lab testing that may include urine toxicology.
A diagnosis follows DSM-5-TR criteria for substance use disorders, specifying severity, associated conditions, and functional impacts.
Care then unfolds longitudinally. The physician develops a tailored treatment plan, prescribes medications for addiction treatment (MAT) when indicated, coordinates counseling and family work, monitors progress and safety, and adjusts interventions based on response & life changes.
This continuity matters; substance use disorders are chronic, relapsing medical conditions, and stability improves with ongoing medical oversight.
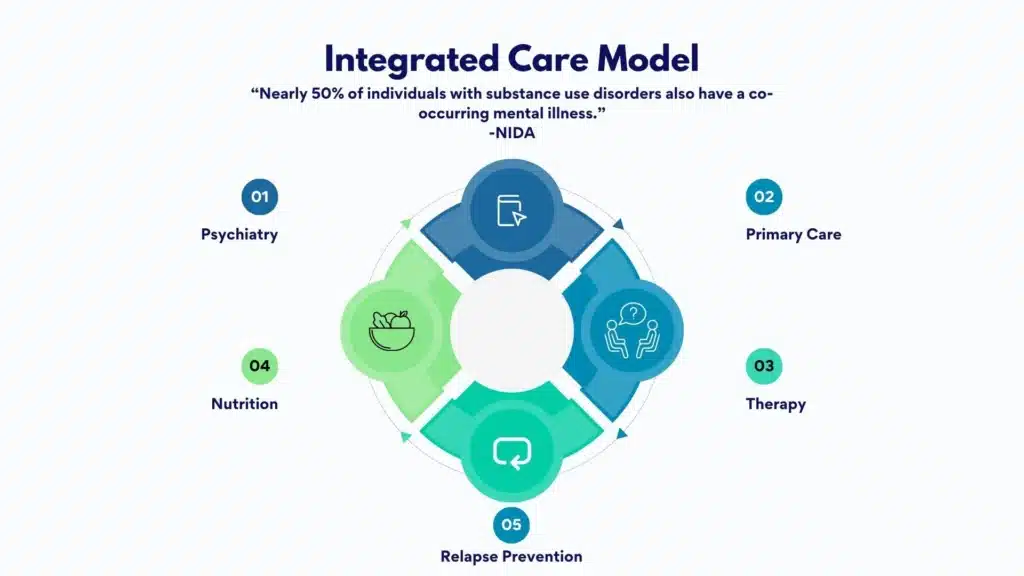
At Rolling Hills Recovery Center in New Jersey, addiction therapists integrate evidence-based care with holistic supports.
The clinical team aligns medical treatment with therapy, wellness strategies, and practical recovery supports, acknowledging each person’s strengths, goals, and culture.
Training and Credentials in NJ
Addiction doctors practice under New Jersey medical licensure and, ideally, hold board certification in addiction medicine (ABPM/ABAM) or addiction psychiatry (ABPN).
Many maintain credentials at hospitals or accredited clinics. In New Jersey, prescribers of buprenorphine require a current DEA registration with Schedule III authority.
Though the former federal waiver (X-waiver) is no longer required, training and competency remain essential to safe prescribing.
Credentialing often includes:
- NJ Division of Consumer Affairs licensure verification
- Hospital or ambulatory care facility privileges, when relevant
- DEA registration and compliance with state prescribing rules
- Familiarity with ASAM Criteria for placement and ongoing level-of-care decisions
Patients should expect a physician who can explain their training, experience, and outcomes. Experience with specific substances, opioids, alcohol, stimulants, sedatives, and co-occurring conditions is especially important for complex cases.
Evidence-Based Care Across ASAM Levels with Collaborative, Trauma-Informed Practice
Addiction medicine in NJ is anchored in evidence-based standards, including the ASAM Criteria.
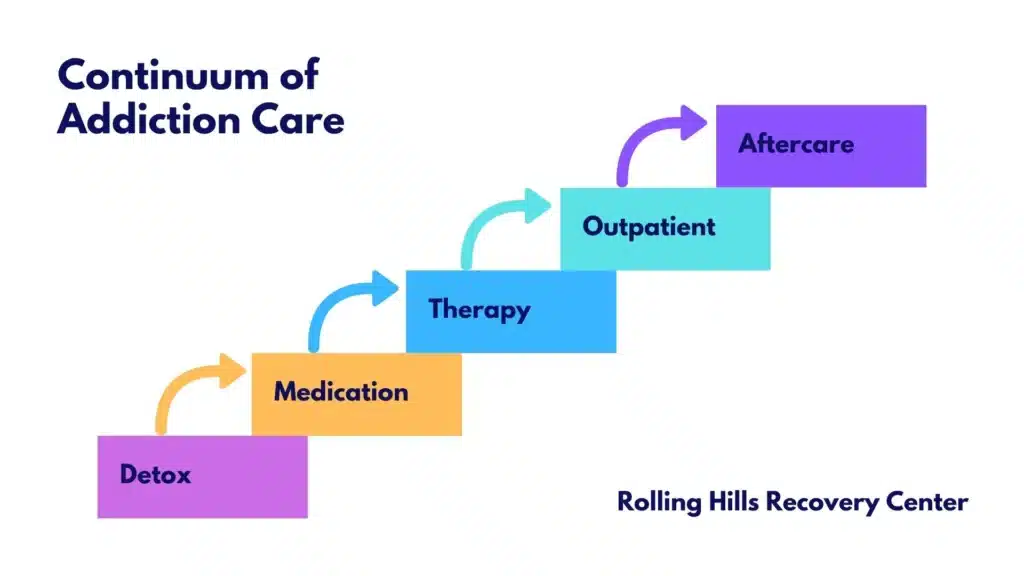
Doctors match patients to the least intensive, safe level of care: from early intervention and outpatient, to intensive outpatient (IOP), partial hospitalization (PHP), residential, or inpatient withdrawal management.
Transitions between levels occur as needs change.
Care is typically collaborative. Physicians coordinate with therapists, peer specialists, case managers, and, when appropriate, family.
Trauma-informed practice is standard: clinicians seek to build safety, choice, and empowerment, and avoid re-traumatization. Screening for trauma exposure and related symptoms guides therapy selection and pacing.
Rolling Hills Recovery Center emphasizes whole-person care, combining proven evidence-based treatments with counseling, wellness practices, and recovery skills to support durable outcomes that last beyond discharge.
Management of Co-Occurring Mental Health Disorders and Medical Comorbidities
Co-occurring disorders are common. Depression, anxiety, PTSD, bipolar disorder, ADHD, and psychotic disorders often intersect with substance use.
Medical issues, including liver disease, HIV/HCV risk, cardiac disease, pain disorders, and pregnancy, also shape the plan.
Addiction doctors coordinate diagnostic clarification, optimize psychotropic medications, and synchronize care with psychiatry, primary care, and specialists.
The physician’s role includes:
- Differentiating substance-induced symptoms from independent psychiatric disorders
- Managing risk of withdrawal or intoxication that complicates other conditions
- Monitoring drug–drug interactions
- Integrating pain management, sleep hygiene, and nutrition into treatment
- Supporting reproductive health, including pregnancy-safe MAT when needed
Safe Prescribing, PDMP Checks, and Monitoring
Responsible prescribing is non-negotiable. New Jersey addiction doctors check the NJ Prescription Drug Monitoring Program (PDMP) before initiating or renewing controlled medications and periodically thereafter.
Urine drug testing is used when clinically appropriate, with consent, to guide care safely, never as punishment. Frequency varies, but it often occurs more frequently early in treatment, then tapers as stability improves.
Physicians document informed consent, discuss risks and benefits, and use treatment agreements for controlled prescriptions.
Overdose risk counseling and naloxone distribution are part of routine care. Data-driven monitoring, symptom scales, craving assessments, and functional outcomes help clinicians adjust plans quickly when warning signs appear.
Treatments and Care Approach
Medications for Addiction Treatment (MAT)

MAT improves survival and retention in care, reduces relapse risk, and stabilizes brain and body systems affected by substance use.
Three medications anchor opioid use disorder (OUD) treatment: buprenorphine, methadone, and naltrexone.
Treatment for alcohol use disorder (AUD) includes approved medications such as naltrexone, acamprosate, and disulfiram. Dosing and monitoring are individualized.
Below is a high-level comparison of core OUD medications:
| Medication | How it works | How it’s given | Patients who can complete an opioid-free period and are motivated to avoid all opioids | Advantages | Considerations |
|---|---|---|---|---|---|
| Buprenorphine | Partial opioid agonist; reduces withdrawal and cravings | Sublingual tabs/films daily; long-acting injection also available | Patients needing office-based treatment with flexibility | Lower overdose risk than full agonists; office-based; can start soon after mild withdrawal begins | Risk of precipitated withdrawal if started too early; requires adherence; diversion safeguards |
| Methadone | Full opioid agonist; stabilizes receptors and blocks withdrawal/cravings | Daily dosing at certified opioid treatment programs (OTPs) | Patients with high physiologic dependence, prior buprenorphine non-response, or needing structured dosing | Strong evidence for retention; good for severe cases | Daily visits initially; QTc monitoring in some cases; interactions with sedatives |
| Naltrexone (extended-release) | Opioid antagonist; blocks opioid effects | Monthly injection | Patients who can complete an opioid-free period, and are motivated to avoid all opioids | No opioid agonist effect; no withdrawal if stopped | Requires full detox first; not for those requiring opioid analgesia; risk of reduced tolerance if relapse occurs |
In real life, clinicians often combine MAT with counseling and recovery skills. Rolling Hills Recovery Center uses shared decision-making to match the right medication to the right person at the right time.
For those searching for help with opioids, a resource like heroin addiction treatment near me can be a starting point to speak with a clinician about MAT options.
Psychotherapies: CBT, Motivational Interviewing, Contingency Management, and Family Work
- Cognitive behavioral therapy (CBT) helps patients identify triggers, reframe thoughts, and build coping skills.
- Motivational interviewing strengthens internal motivation, reduces ambivalence, and aligns goals with personal values.
- Contingency management uses positive reinforcement to encourage recovery behaviors like negative toxicology results or session attendance.
- Family-based interventions improve communication, set healthy boundaries, and reduce enabling or conflict.
Therapy selection is tailored. For example, early recovery may prioritize motivational work and craving management, while later phases may emphasize relapse prevention and family systems.
Rolling Hills integrates individual, group, and family sessions with practical skill-building, sleep, stress, routine, and social support, so gains hold outside the clinic.
Recovery Planning, Relapse Prevention, Harm Reduction, and Overdose Education
Relapse prevention is an active process. Doctors and therapists collaborate on a written plan that lists triggers, early warning signs, coping skills, medication adherence strategies, and a step-by-step crisis plan if a lapse occurs.
Harm reduction is always included: sterile supplies where legal, infection prevention, safe-use education, and naloxone training.
Overdose education covers tolerance changes, mixing risks (especially with alcohol or benzodiazepines), and how to use naloxone. Families and trusted supports are often trained as well.
Patients working with prescription medications, opioids, benzodiazepines, and stimulants benefit from structured tapers, alternative therapies, and lock boxes at home.
Those needing specialized support can review options such as prescription drug addiction treatment to understand next steps, insurance, and timelines.
Monitoring, Telehealth, Privacy, and Culturally Responsive Care
Monitoring includes symptoms, side effects, cravings, toxicology when appropriate, vital signs, and functional outcomes at school, work, or home.
Telehealth can extend reach and reduce barriers, especially for follow-ups and counseling, if clinically suitable.
Sensitive care requires strict HIPAA compliance; patients should understand their rights, consent forms, releases of information, and how data are protected.
Culturally and linguistically competent care meets people where they are.
This can include bilingual clinicians or certified interpreters, culturally relevant psychoeducation, spiritual or community supports, and adaptation for literacy level.
Rolling Hills Recovery Center commits to respect and inclusion, because belonging improves engagement and outcomes.
Choosing the Right Addiction Treatment Doctors in NJ
How to Verify Credentials, Experience, and Fit
Finding the right physician requires a few checks. Training in addiction medicine or psychiatry signals specialization.
New Jersey physicians must hold an active state license and an active DEA registration if prescribing controlled medicines.
Fit also matters; does the doctor have experience with your substance(s) and co-occurring conditions, including mental health or pain?
Step 1 – Confirm licensure and standing. Use the NJ Division of Consumer Affairs License Verification to verify current status, any actions, and specialty listings.
Step 2 – Confirm DEA registration for controlled prescribing. The office can attest to active registration.
Step 3 – Assess experience and scope. Ask how frequently they treat OUD, AUD, stimulant or sedative use disorders, and complex cases like pregnancy, liver disease, or severe mental illness.
Step 4 – Clarify availability. Determine wait times for new patients, same-week slots for urgent needs, and 24/7 on-call protocols.
Step 5 – Understand coverage. Verify insurance acceptance, prior authorization requirements for MAT, and estimated out-of-pocket costs.
Patients seeking comprehensive programs can explore how to find the best addiction treatment in NJ to compare services, levels of care, and integrated supports.
Questions to Ask About MAT, Therapy, Outcomes, and Coordination
The best programs combine medications, therapy, peer support, case management, and aftercare.
They track program outcomes, retention, abstinence or reduced use, employment/school stability, ER visits, adherence, and use data to improve.
Coordination with primary care and psychiatry is standard, as is aftercare planning that includes relapse prevention, alumni supports, and rapid access if symptoms recur.
A few specifics to discuss:
- MAT availability onsite (buprenorphine, methadone via OTP coordination, naltrexone), and for AUD, naltrexone, acamprosate, disulfiram
- Counseling modalities used (CBT, motivational interviewing, contingency management, family sessions)
- Expectations for toxicology testing and PDMP checks
- Telehealth policies, privacy, and HIPAA-compliant platforms
- Collaboration with outside providers and information-sharing with consent
- Safety planning, including naloxone distribution and training for loved ones
Red Flags to Avoid
- Guarantees of cure or 100% success promises
- One-size-fits-all protocols with no individualized assessment
- Refusal to discuss or offer MAT when indicated
- Lack of licensure, DEA registration, or unclear credentials
- No outcome tracking or reluctance to coordinate with other clinicians
- Cash-only with limited transparency on costs or privacy policies
- Red flags at intake or during care:
- Pressure to sign long-term contracts without a clear medical rationale
- Minimal screening for co-occurring mental health conditions
- Punitive use of urine testing rather than clinical collaboration
Access and Next Steps
How Referrals Flow: Primary Care, Emergency Departments, and Courts
Entry points vary. Many patients are referred by primary care after screening positive for risky use or a substance use disorder.
Emergency departments often begin buprenorphine for opioid withdrawal and make a warm handoff to outpatient addiction care.
Courts or probation programs may require assessment and compliance with treatment plans that meet ASAM Criteria and licensed-program requirements.
Rolling Hills Recovery Center accepts referrals from medical practices, hospitals, behavioral health providers, schools, and employers.
Self-referrals are welcome; patients or families can contact admissions to discuss symptoms, level of care, and timing.
Using Helplines, State Resources, and Transport
For immediate guidance, the SAMHSA National Helpline offers 24/7 confidential support and referrals: SAMHSA National Helpline.
New Jersey’s Department of Human Services, Division of Mental Health and Addiction Services (DMHAS), maintains programs, licensure information, and funding options for eligible residents: NJ Department of Human Services DMHAS.
Evidence standards are summarized in the NIDA Principles of Effective Treatment; physicians use these principles to shape care.
Transportation can be a barrier. Patients should ask about telehealth, evening hours, or local transit support. Some programs provide ride-share vouchers or work with county services to reduce missed visits.
What to Bring to the First Visit
Preparation shortens time to treatment and improves safety. Bring:
- Government ID, insurance card, and emergency contact information
- A list of all medications and doses (including over-the-counter, supplements)
- Past medical records, if available: discharge summaries, lab results, EKGs
- A history of substances used, amounts, timing of last use, and any prior treatments
- Names and contact info of other clinicians (primary care, psychiatry, therapists)
- Legal documents, if relevant: court orders, probation terms, or monitoring requirements
If a patient cannot gather all items, care should not be delayed; doctors can help obtain records later with consent.
Questions to Ask at Intake
- What will the first 30 days of treatment look like for me?
- Which medication options fit my goals & risks, and how soon can they start?
- How often will visits and toxicology testing occur early on?
- How will you coordinate with my primary care and psychiatrist?
- What are my rights under HIPAA, and how do I control information sharing?
- Can my family or support person join parts of the visit?
- What aftercare will be in place when I step down in level of care?
Safety Planning and Involving Supporters
Safety planning should be written, simple, and accessible to both the patient and trusted supporters.
It typically includes warning signs, coping strategies, medications to take or avoid, people to contact, and when to go to urgent care or call 911.
Doctors equip families with naloxone and training. Employers may be engaged when appropriate; honest communication, within the limits of consent, often leads to better recovery support at work.
Rolling Hills Recovery Center works with employers and EAPs when desired by the patient, aligning return-to-work timelines with medical stability and job demands.
Early involvement of supportive family members, if safe and wanted, improves adherence and reduces relapse risk.
Documentation for FMLA and Return-to-Work
Addiction doctors commonly complete paperwork for:
- FMLA or NJ Family Leave Insurance for protected time off to receive treatment
- Short-term disability forms when symptoms limit work capacity
- Return-to-work clearances with or without restrictions
- Progress notes or attendance letters were legally permitted and requested by the patient
Timely documentation requires accurate visit records and clear communication about job duties.
Patients should give their clinician job descriptions if specific physical or cognitive demands must be considered. Employers often appreciate a phased return plan that balances productivity and safety.
Practical How-to: Navigating Care Step by Step in New Jersey
Step 1 – Recognize the Need and Reach Out
If withdrawal symptoms, cravings, or consequences (health, legal, work, or relationships) are mounting, it is time to call.
Contact a reputable program like Rolling Hills Recovery Center or a 24/7 resource such as the SAMHSA National Helpline.
Ask for the next available assessment and request guidance on immediate safety needs, overdose risk, severe withdrawal, or co-occurring crises.
Step 2 – Prepare for the Assessment
Note recent substance use, last use time, and any history of withdrawal seizures or delirium tremens. List medications and allergies.
Identify someone who can help with transport and support after the visit. If there’s a risk of opioid overdose, obtain naloxone from a pharmacy or program prior to the appointment if possible.
Step 3 – Complete a Comprehensive Evaluation
At intake, the doctor will evaluate substance use patterns, mental health, medical issues, and social supports. Lab testing and urine toxicology may be ordered.
The physician will explain the diagnosis and outline level-of-care options per ASAM Criteria.
Shared decision-making determines whether to begin medication the same day and what therapy plan to pair with it.
Step 4 – Initiate Treatment and Stabilize
For OUD, buprenorphine may start once mild withdrawal begins, or methadone may be coordinated through an OTP. For AUD, medication can start even if continuing to drink, depending on the agent.
Counseling sessions begin quickly, often within the first week. Patients receive education on side effects, interactions, and warning signs to report.
Step 5 – Build Recovery Skills and Prepare for Triggers
The team helps with sleep hygiene, nutrition, exercise, and stress management. Patients learn to identify triggers and rehearse responses.
Family sessions encourage supportive communication and boundary setting. Recovery-support meetings or peer mentors can be added, matching the person’s preferences and culture.
Step 6 – Monitor, Adjust, and Plan Aftercare
As stability improves, visit frequency tapers; telehealth may replace some in-person appointments. The doctor tracks outcomes and updates the plan accordingly.
Before stepping down from IOP to standard outpatient, an aftercare plan is finalized: ongoing medication management, therapy, alumni groups, a relapse prevention plan, and re-entry pathways if symptoms recur.

Special Populations and Clinical Nuances
Adolescents and Young Adults
Adolescent treatment requires developmentally appropriate approaches, family engagement, and school coordination. Physicians weigh confidentiality with family involvement to maintain trust and safety.
Early intervention reduces the risk of long-term complications.
Pregnancy and Postpartum
Pregnant patients with OUD benefit from methadone or buprenorphine, which reduce maternal relapse and improve prenatal care engagement.
Tapering is generally discouraged during pregnancy due to relapse and overdose risk.
Postpartum support and coordination with pediatric care are essential, including planning for possible neonatal opioid withdrawal syndrome (NOWS).
Chronic Pain and Sedative Use
For co-occurring chronic pain, multimodal pain care is prioritized, including non-opioid medications, physical therapy, behavioral pain interventions, and procedures when appropriate.
If benzodiazepines are involved, physicians plan slow, carefully monitored tapers, alternative anxiety treatments, and watch for overdose risks with opioids or alcohol.
Stimulant Use Disorders
While no FDA-approved medications exist for stimulant use disorder, contingency management, CBT, structured scheduling, and sleep stabilization are effective.
Physicians carefully evaluate for co-occurring ADHD or mood disorders and treat accordingly, balancing the benefits and risks of any stimulant medications.
Quality, Measurement, and Continuous Improvement
What Good Programs Measure
Quality care is measurable. Addiction physicians and programs track:
- Engagement and retention across levels of care
- Substance use (self-report and toxicology where appropriate)
- MAT adherence and tolerability
- Emergency department visits and hospitalizations
- Functioning in work, school, and relationships
- Patient-reported outcomes and satisfaction
- Safety events, including overdose or medication interactions
Rolling Hills Recovery Center uses these indicators to refine care pathways and training, and to close equity gaps across groups. Data-driven improvements help sustain recovery results that matter to patients and families.
Holistic and Complementary Supports
Integrating Wellness Into Medical Care
Holistic supports enhance medical treatment. Stress-reduction techniques, mindfulness, yoga or gentle movement, nutritional counseling, and sleep coaching can lower cravings and improve mood stability.
Social determinants are addressed: secure housing, transportation, legal aid, and employment support.
When coordinated under a medical plan, these services can be powerful adjuncts rather than replacements for evidence-based treatment.
Patients considering comprehensive, integrated care often compare options and read about program strengths, services, and outcomes.
Rolling Hills offers referrals to medical and therapeutic approaches in one coordinated environment, with attention to culture, language, and family life.
Insurance, Authorization, and Cost Considerations
Navigating Coverage
Addiction treatment is covered under parity laws, but details vary by plan.
Physicians’ offices can help verify benefits, identify in-network options, and submit prior authorizations for medications like buprenorphine/naloxone films or extended-release naltrexone injections.
If an OTP is needed for methadone, coverage is confirmed before enrollment. Appeals may be necessary for level-of-care denials; documented medical necessity, aligned with ASAM Criteria, supports approval.
Co-pays, deductibles, and transportation costs should be discussed upfront. Sliding scales or state-funded slots may be available for eligible residents through DMHAS-designated programs.
Care teams work with patients to minimize financial barriers that could destabilize recovery.
Documentation, Privacy, and Legal Protections
HIPAA, 42 CFR Part 2, and Consent
Addiction treatment often involves sensitive information. Programs follow HIPAA and, where applicable, 42 CFR Part 2 for extra confidentiality protections.
Patients control who sees their information, with signed releases specifying what is shared and why. Digital platforms for telehealth must be secure; patients can ask how data is stored and who can access it.
Court Involvement and Monitoring
For individuals under court supervision, doctors provide required assessments, toxicology schedules, and progress reports within the bounds of consent and law.
The clinical goal remains the same: safe, effective care that supports health, work, family, and community participation.
When to Seek Higher Care or Urgent Help
Recognizing Emergencies
Rapid escalation is needed if there are:
- Signs of severe withdrawal (e.g., seizures, hallucinations)
- Overdose or suspected overdose, call 911 immediately; administer naloxone if opioids are involved
- Suicidal thoughts or plans, seek immediate emergency care
- Dangerous intoxication with risk to self or others
Doctors coordinate transitions to inpatient withdrawal management or medical units when indicated. After stabilization, the care plan is updated to reduce future crises.
How Rolling Hills Recovery Center Supports New Jersey Patients
Integrated Care Built on Evidence and Compassion
Rolling Hills Recovery Center delivers evidence-based addiction medicine with holistic support. The program provides access to MAT, therapy (CBT, motivational interviewing, and DBT), family work, and robust aftercare.
Co-occurring mental health and medical conditions are managed in concert, not in silos. Policies align with HIPAA, and culturally responsive care is standard.
For individuals seeking alcohol-focused help, opioid treatment, or broader services, the team offers clear pathways, same-week access when possible, and coordination with outside providers.
Patients and families who have questions about alcohol, opioid, stimulant, or sedative treatment options can review services and connect with admissions to explore an individualized plan.
Conclusion
Choosing the right New Jersey addiction treatment doctor is central to safe, effective care. Verify credentials, ask about MAT and therapy, and confirm insurance fit & intake steps. Expect collaborative planning with clear follow‑up. Schedule an assessment and bring records.
Frequently Asked Questions (FAQs)
What Do Addiction Treatment Doctors in New Jersey Actually Do?
Addiction treatment doctors evaluate, diagnose, and treat substance use disorders using proven medical and behavioral methods.
In New Jersey, they complete a comprehensive assessment, determine ASAM level of care, and create a plan that can include medication for addiction treatment, structured therapy, and medical monitoring.
They coordinate with primary care & psychiatry, check the NJ Prescription Drug Monitoring Program when prescribing controlled medications, and order tests like urine toxicology when clinically indicated.
Privacy is protected under HIPAA, and care is individualized for co-occurring mental health, pregnancy, chronic pain, and other medical needs.
How Can Someone Verify the Credentials of Addiction Treatment Doctors in NJ?
Verification should be simple and transparent. Confirm an active New Jersey medical license through the NJ Division of Consumer Affairs, and look for board certification in Addiction Medicine or Addiction Psychiatry.
A current DEA registration is required to prescribe controlled medications; the older waiver requirement for buprenorphine is no longer in place.
Ask about hospital or clinic privileges, experience with the specific substance involved, and whether they follow evidence-based standards like the ASAM Criteria.
Red flags: guaranteed cures, one-size-fits-all protocols, or refusal to coordinate with other clinicians and family when appropriate consents are in place.
What Should a Patient Bring to a First Visit with Addiction Treatment Doctors?
Bring a photo ID & insurance card, a list of all medications and allergies, recent medical records if available, and contact information for prior clinicians or counselors.
Expect a respectful screening that may include DSM-5 SUD criteria, withdrawal risk review, physical exam, labs when needed, and a discussion of risks & benefits of options like buprenorphine, methadone, or naltrexone.
Safety planning includes routine overdose education, naloxone access, and crisis contacts. It’s okay to bring a supportive family member; consent will be discussed first.
Are Medications Used by Addiction Treatment Doctors (Like Buprenorphine, Methadone, and Naltrexone) Safe?
When prescribed and monitored correctly, these medications are safe and effective.
Buprenorphine reduces cravings and withdrawal with a ceiling effect that lowers overdose risk; methadone is highly effective for opioid use disorder when dosed and observed properly; naltrexone blocks opioid receptors and can support relapse prevention once the patient is opioid-free.
Doctors review interactions, adjust for liver or kidney issues, and monitor side effects such as constipation, sedation, or precipitated withdrawal.
For alcohol use disorder, options like naltrexone and acamprosate may be discussed, too. Shared decision-making and regular follow-up keep treatment safe and stable.
How Does Rolling Hills Recovery Center Work with Addiction Treatment Doctors in New Jersey?
Addiction treatment doctors collaborate closely with the Center’s therapists and case managers to align medication choices with therapy, address co-occurring conditions, and support family involvement when appropriate.
Care plans emphasize measurable goals, relapse prevention, and step-down planning, with smooth transitions to outpatient services and community supports so progress isn’t lost between levels of care.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts