Drug counseling abuse is more than talk; it’s structured, evidence-based care that helps people reduce harm and rebuild health. Drawing on clinical practice and research, a medical addiction specialist outlines what works, who benefits, and how to start. Expect clear steps, practical tools, and safety-first planning that align with compassionate care & measurable outcomes.
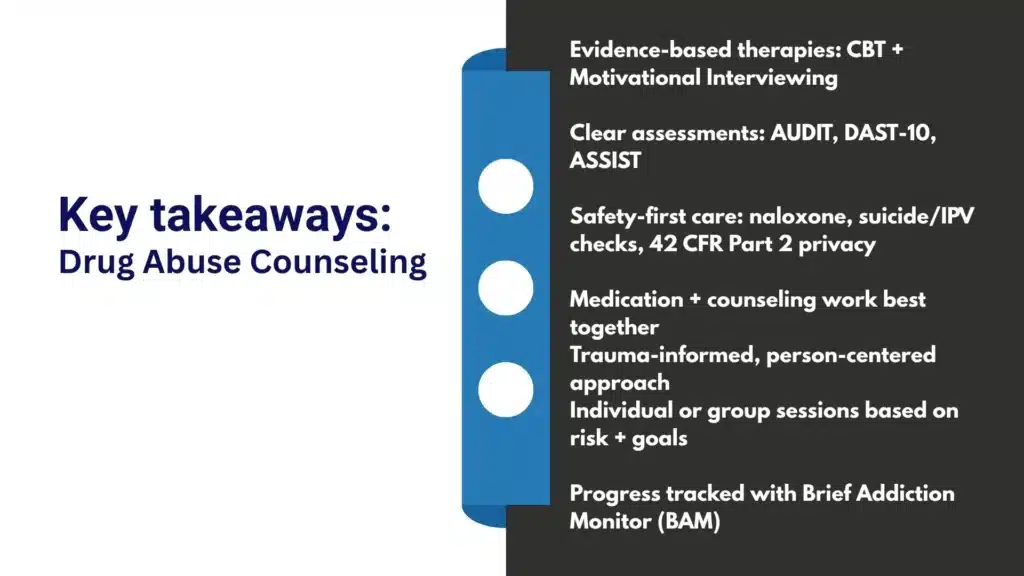
Key Takeaways
- Effective counseling blends CBT & motivational interviewing, with contingency management as needed; medications for opioid and alcohol use disorders often raise success rates.
- Start with a careful assessment: brief screens (AUDIT, DAST‑10, ASSIST), medical and mental health review, and ASAM Criteria to match level of care; goals stay specific and realistic.
- Safety first, overdose teaching with naloxone, urine drug testing when needed, privacy under HIPAA and 42 CFR Part 2, and family involvement when it helps.
- Care is delivered in person and by telehealth; sessions follow a simple flow (agenda, skills practice, homework), recovery supports continue after discharge; progress is tracked with the Brief Addiction Monitor… and clinical judgment.
Scope and Goals of Drug Abuse Counseling
Role Across the Continuum of Care
Counseling spans prevention, early intervention, acute stabilization, ongoing treatment, and long-term recovery management.
It supports people entering care for the first time, those stepping down from residential programs, and individuals re-engaging after relapse.
At Rolling Hills Recovery Center in New Jersey, counseling is integrated with medical services and wellness supports, because results are better when behavioral care and medication, plus social supports, move together rather than in silos.
Core goals include:
- Reduce substance-related harm and risks (overdose, infections, impaired driving).
- Improve control over use, then sustain abstinence or safer use depending on the plan.
- Treat co-occurring mental health symptoms.
- Strengthen life roles: health, work or school, family, and community ties.
- Build recovery capital so progress holds during stress.
The team prioritizes evidence-based counseling but respects personal choice. If someone isn’t ready to stop, harm reduction and motivational work come first. When a patient wants abstinence, strategies adjust accordingly.
Safety Planning, Confidentiality, and 42 CFR Part 2
Every patient deserves privacy and safety. Substance use disorder records receive extra protection under 42 CFR Part 2, which requires specific written consent to share SUD information outside the program (even with other health providers in many cases). Counselors:
- Obtain clear, time-limited consents stating what information can be shared, with whom, and for what purpose.
- Explain exceptions (emergencies, mandated reporting).
- Use releases that can be revoked at any time.
Safety plans cover suicide risk, self-harm, overdose, and intimate partner violence (IPV). Plans are created collaboratively and revisited as needs change.
In outpatient care, safety planning is active, not a checkbox: contacts, crisis steps, and means of safety (e.g., lockboxes for meds, removing lethal means when feasible) are documented and practiced.
Harm Reduction and Family Involvement
Harm reduction accepts that change may be gradual. Counselors provide naloxone education, safer-use strategies, syringe services referrals where appropriate, and fentanyl test strip information.
Family involvement enhances outcomes when the patient consents.
Methods such as Community Reinforcement and Family Training (CRAFT) teach loved ones how to reinforce healthy steps and reduce criticism or enabling.
Family therapy sessions focus on communication, boundaries, and practical support around medications, appointments, and triggers at home.
Rolling Hills Recovery Center combines evidence-based counseling and holistic approaches, so family, social, and wellness dimensions are woven into care.
Evidence-Based Modalities to Prioritize
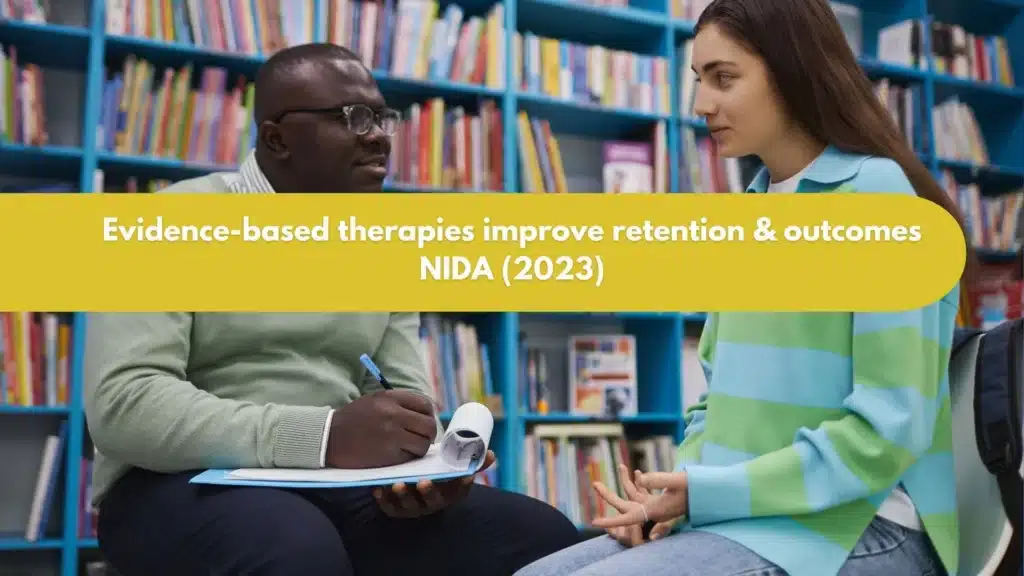
Cognitive Behavioral Therapy and Motivational Interviewing
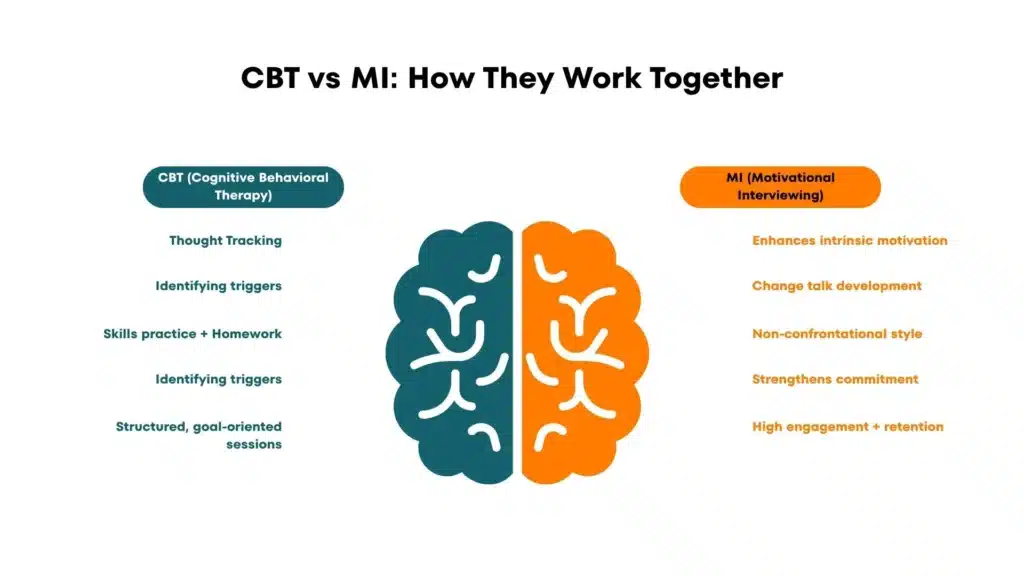
CBT for addiction equips patients to recognize triggers, challenge unhelpful thoughts, and build alternative coping skills. Counselors teach cue management, problem-solving, emotion regulation, and behavioral activation.
MI is the style that aligns with ambivalence, evoking change talk, rolling with resistance, and strengthening the person’s own reasons to change.
MI increases engagement and retention; CBT builds the skills to maintain gains. Both are first-line and work across substances and settings.
Practical markers of fidelity:
- MI: open questions, affirmations, reflective listening, summaries; minimal persuasion; reflections > questions.
- CBT: clear agendas, brief functional analyses, skills practice, and homework with troubleshooting at the next session.
Contingency Management and Community Reinforcement
Contingency Management (CM) uses immediate, meaningful reinforcers for target behaviors (negative drug screens, session attendance, medication adherence).
It is among the most effective tools for stimulants and works well for other substances when combined with therapies.
Community Reinforcement Approach (CRA) rebuilds a rewarding sober life: job skills, hobbies, family time, and social activities that make nonuse more rewarding than use.
Trauma‑Informed Care
Traumatic experiences are common in substance use disorders. Trauma-informed counseling ensures physical and emotional safety, trustworthiness, and collaboration. Therapists pace skills carefully (grounding, distress tolerance) and avoid forcing disclosure.
When indicated, evidence-focused trauma therapies (e.g., Cognitive Processing Therapy) are integrated only when the patient is stable enough to tolerate them. The therapeutic stance is nonjudgmental and transparent.
Integrated Treatment for Co‑Occurring Disorders
Substance use and mental health symptoms interact, often worsening each other. Integrated care for co-occurring disorders treats both disorders together. Examples:
- Depression or anxiety: CBT plus SSRIs or SNRIs when appropriate.
- Bipolar disorder: mood stabilizers plus routine sleep and routine scheduling skills.
- Psychosis: antipsychotic management with careful substance monitoring.
- PTSD: staged care with coping first, then trauma-focused work when ready.
Care managers coordinate across prescribers and therapists; unified treatment plans avoid conflicting instructions.
Medication Coordination for OUD and Stimulant Use Disorder
For opioid use disorder, FDA‑approved medications, methadone, buprenorphine, and extended‑release naltrexone cut mortality and reduce illicit opioid use.
Counseling coordinates dosing schedules, addresses stigma, and targets barriers like missed appointments or withdrawal anxiety. For stimulant use disorders, there is no FDA‑approved medication; CM, CRA, and CBT remain the foundation.
Some patients benefit from targeted pharmacotherapy for co-occurring conditions (e.g., bupropion for depression), sleep normalization, nutritionally dense meals, and exercise plans.
Rolling Hills clinicians align therapy plans with medications, monitor side effects, and coach people through transitions like initiating buprenorphine or, if appropriate, a naltrexone trial. For comprehensive care in New Jersey, explore treatment for substance abuse.
Individual vs Group Formats: When and Why
Both formats are useful; selection depends on goals, stage of change, and risk profile.
| Format | Indications | Advantages | Considerations |
|---|---|---|---|
| Individual counseling | Acute risk, high symptom burden, complex comorbidity, privacy needs, trauma sensitivity | Stable engagement, peer support potential, skills practice with others,and cost-effective | May limit peer learning; schedule demand |
| Group counseling | Normalizes experience, shared strategies, role modeling, and CM can be group-based | Stable engagement, peer support potential, skills practice with others, and cost-effective | Not ideal for acute risk, certain trauma triggers, or strict confidentiality needs |
Group therapy for addiction is powerful for relapse prevention, skills practice, and peer learning. Individuals with active IPV concerns or severe social anxiety may start in individual sessions and later join groups as comfort grows.
Assessment and Care Planning
Standardized Screening: AUDIT, DAST‑10, ASSIST, CRAFFT
Use brief screens at intake and periodically:
- AUDIT for alcohol risk and severity.
- DAST‑10 for drug-related problems.
- ASSIST to identify risk across substances and guide brief interventions.
- CRAFFT for adolescents; it captures risky use patterns in teens.
When positive, move to diagnostic interviewing aligned with DSM‑5 criteria. Screening results inform the level of care, urgency, and immediate safety steps.
Brief Interventions (SBIRT): A Step‑by‑Step
SBIRT fits primary care and specialty settings alike, and it pairs well with MI.
- Screen: administer AUDIT/DAST‑10/ASSIST (CRAFFT if adolescent).
- Brief advice: feedback on results, link substance use to patient goals; elicit change talk rather than tell.
- Negotiate goal: reduce or stop; agree on a small next step.
- Arrange follow‑up: referral to specialty counseling or MOUD if indicated; set a date to check progress.
Sample script:
- “Your score shows a higher risk. What do you make of that?”
- “On a scale of 0–10, how ready are you to change your use?”
- “What’s one change you could try over the next week?”
ASAM Criteria for Level‑of‑Care Decisions
The ASAM Criteria guide placement using six dimensions: intoxication/withdrawal potential; biomedical conditions; emotional/behavioral conditions; readiness to change; relapse/continued use potential; recovery environment.
Counselors synthesize assessment data to match the least restrictive, safe level: outpatient, intensive outpatient, partial hospitalization, residential, or withdrawal management. Reassess regularly; movement between levels is normal and clinically appropriate.
Toxicology Testing: UDT with Confirmatory GC/MS
Urine drug testing supports clinical decisions, not punishment. Set expectations up front. Use immunoassay screens for speed, but confirm unexpected positives or negatives with GC/MS or LC‑MS/MS.
Document timing, medications, allergens, and cross‑reactants. Discuss results in MI style:
- Explore the patient’s view.
- Problem-solve rather than confront.
- Modify the plan if risk increases (e.g., more frequent visits, medication adjustments, stepped-up CM).
Collaborative Treatment Planning with SMART and Cultural Considerations
Plans must be co-authored. Use SMART goals (Specific, Measurable, Achievable, Relevant, Time‑bound). Respect cultural values, language preferences, faith practices, family roles, and stigma concerns.
Ensure materials are readable and interpreters are offered if needed. Examples:
- “Reduce cocaine use from daily to none for the next 30 days, verified by weekly UDT and two skills groups per week.”
- “Attend two family sessions this month to practice boundary statements.”
Example Tools and Templates
Template: Safety Plan
- Warning signs:
- Internal coping strategies:
- People and places for distraction:
- People to ask for help:
- Professionals and clinics:
- Means safety steps:
- Crisis lines:
Template: Weekly Recovery Schedule
- Sleep target:
- Medication times:
- Appointments (therapy, groups, MAT):
- Exercise or movement:
- Meals and hydration:
- Connection time (peer group, family, sponsor):
- Unstructured recovery activity:
Template: CBT Functional Analysis
- Trigger:
- Thoughts:
- Feelings (0–10):
- Behavior:
- Consequence:
- Alternative response for next time:
Delivery and Engagement
Telehealth and In‑Person Workflows
Telehealth expands access and works well for many. Decide format by patient preference, privacy, technology, risk level, and clinical needs.
- Before session: confirm location and a callback number; verify privacy; check consent for telehealth.
- Risk checks: ask about suicidality and safety; know local emergency resources.
- Identity and medication verification when relevant; secure platform.
- Contingency plan: if video drops, call immediately; document.
In-person sessions are preferred when patient privacy at home is limited, when trauma cues are high, or complex assessments are needed. For both formats, begin on time, set an agenda, and end with a brief summary and next steps.
Session Structure: Rapport, Agenda, Skills Practice, Homework
A reliable structure helps:
- Warm check-in and vitals if medically indicated.
- Quick review of wins, barriers, and the last homework.
- Agenda setting (two or three items max).
- Short skills segment (e.g., urge surfing practice).
- Action plan, homework, and troubleshooting obstacles.
- Measure brief outcomes (e.g., craving 0–10) and confirm next appointment.
Even “small” homework, one thought record, or one coping practice, keeps momentum.
Relapse Prevention and Overdose Education with Naloxone
Relapse prevention is both skills and environment shaping. Counselors teach trigger mapping, coping skills, refusal scripts, and crisis cards. Overdose education belongs in every plan for anyone using opioids or at risk due to fentanyl contamination.
- Naloxone: how to get it, when to use, and quick instructions.
- Never use alone; test dose; avoid mixing with alcohol/benzodiazepines.
- Tolerance drops fast after abstinence; warn strongly after detox or jail.
- Encourage carrying naloxone and teaching family/roommates.
Document overdose education and naloxone access at intake and updates over time.
Building Recovery Capital and Connecting to Peer Supports
Recovery capital refers to the personal, social, and community assets that sustain change. Counselors map strengths (skills, supportive people, housing, transportation, purpose) and build deficits one at a time: ID documents, health insurance, resume, childcare, credit repair, and sober recreation.
Peer mutual-help groups complement, not replace, clinical care. Options include 12‑Step (AA/NA), SMART Recovery, LifeRing, Celebrate Recovery, and Refuge Recovery. Counselors help patients test options and choose what fits.
Adolescents benefit from youth-specific supports, family coaching, and school coordination. Rolling Hills offers coordinated adolescent care; see our article on substance abuse treatment for teens.
Outcomes, Ethics, and Quality
Tracking Progress: Brief Addiction Monitor and PROMs
Routine measurement improves care. The Brief Addiction Monitor (BAM or BAM‑R) tracks risk and protective factors over the past week. Pair it with patient-reported outcome measures (PROMs) such as craving scales, PHQ‑9 for depression, GAD‑7 for anxiety, and quality-of-life measures.
Clinician instruments like the Addiction Severity Index (ASI‑Lite) or Clinical Global Impressions add structure. Graph changes over time, and sharing with the patient, collaborative, transparent feedback, sharpens plans quickly when things drift.
Risk Management: Suicidality and IPV
Suicide risk is monitored at intake and ongoing. Ask directly about ideation, intent, plan, and access to means.
If risk is acute, enact the safety plan and escalate care, same-day psychiatry, higher level of care, or emergency evaluation. For IPV, screen privately and validate disclosures; create a safety plan that may include confidential shelter resources and careful communication strategies.
Document clearly, avoid placing the patient at risk by informing a partner without consent, and know the mandated reporting rules in your state.
Counselors should maintain calm, precise documentation of risk assessments and actions taken, including collateral contacts when authorized.
Informed Consent and Documentation
Informed consent covers the nature of services, risks, benefits, alternatives, limits of confidentiality (including 42 CFR Part 2), telehealth specifics, UDT policies, and CM procedures.
Use plain language and review it aloud. Keep releases of information updated and narrow. Progress notes should state session focus, interventions (MI, CBT skill taught), patient response, any risk updates, and plan.
Avoid stigmatizing language; use person-first, nonjudgmental terms.
Supervision, Fidelity, and Continuous Quality Improvement
High-quality counseling requires supervision, especially for MI and CBT fidelity. Methods:
- Use session checklists (e.g., MI treatment integrity measures, CBT agenda/homework check).
- Audio or video review with patient consent per policy.
- Regular case conferences to review outcomes and safety events.
- Plan–Do–Study–Act cycles to improve no-show rates, retention, and CM workflows.
Rolling Hills emphasizes clinician development, structured onboarding, competency refreshers, and integrated behavioral huddles.
Programs should also monitor disparities in access or outcomes by race, language, gender identity, or insurance type and correct them.
Helpful References for Clinicians
For clinicians who want to go deeper, authoritative resources include:
- NIDA’s Principles of Drug Addiction Treatment (NIDA principles of treatment) for what works and why.
- WHO’s mhGAP Intervention Guide (WHO mhGAP) for scalable counseling procedures in varied settings.
- American Psychiatric Association resources on SUD care (APA SUD resources) for comorbidity and ethics.
- ASAM Criteria overview (ASAM Criteria) for placement and continuing care decisions.
- Cochrane Drugs and Alcohol reviews (Cochrane evidence) to evaluate modality effectiveness and retention.
These references align with the approaches described here and reflect consensus evidence. They underpin how Rolling Hills Recovery Center designs its counseling pathways and integrates medications, trauma-aware care, and family participation.
Practical Worksheets and Quick-Start Checklists
Because patients move fast and life gets messy, having ready-to-use tools helps.
Template: First-Session Checklist
- Obtain consents (treatment, telehealth if used, 42 CFR Part 2 release as desired).
- Complete screens (AUDIT, DAST‑10, ASSIST, CRAFFT for adolescents).
- Risk screen (suicide, overdose, IPV) and initial safety plan.
- Brief intervention (SBIRT) if positive screens.
- Identify immediate goals; schedule next visit; provide naloxone education if indicated.
Template: Medication Alignment Note Snippet
- Current SUD medications: name, dose, adherence.
- Reported side effects and functional impacts.
- Behavioral plan adaptation: transportation, dosing schedule cues, cravings management.
- Pharmacy issues or prior authorization needs.
- Next medication review date.
Template: Recovery Capital Map (condensed)
- Personal: health, skills, coping, motivation.
- Social: supportive people, safe relationships, family alignment, peer groups.
- Community: housing, transport, employment/education, legal, and financial.
- Cultural/spiritual: identity, values, faith, meaning.
- Action items for the lowest two domains this week.
Programs that embed these small templates into routine visits tend to retain patients longer and catch problems early. For coordinated care and access to these tools within a comprehensive program in New Jersey, patients and families can connect with Rolling Hills Recovery Center through the page on substance abuse counseling in New Jersey.
Conclusion
Recovery starts with honest assessment, evidence-based counseling, and steady support. Key takeaways: use proven therapies like CBT & motivational interviewing, protect safety and confidentiality, and pair counseling with medications when appropriate. If you’re ready, schedule an assessment, check benefits, and bring a support person.
Frequently Asked Questions (FAQs)
What is Drug Abuse Counseling and How Does it Work?
Drug abuse counseling is structured, evidence‑based talk therapy that helps a person reduce or stop substance use and stabilize health. Clinicians use methods like cognitive behavioral therapy, motivational interviewing, contingency management, and trauma‑informed care.
Counseling often includes skills practice (craving control, triggers, sleep), relapse prevention, family involvement when appropriate, and coordination with medications for addiction treatment. It’s practical and measured; plans are adjusted by progress, not guesswork.
What Happens in the First Drug Abuse Counseling Session?
The first visit focuses on safety, an honest assessment, and a clear plan. A medical addiction specialist reviews substance use history, mental health, medical issues, and strengths.
Brief screens such as AUDIT or DAST‑10 may be used, and the ASAM Criteria helps match the right level of care. A safety plan is created (overdose risk, naloxone access, crisis contacts), urine drug testing may be discussed, and privacy rights are explained under HIPAA and 42 CFR Part 2. Together, realistic goals are set, what to change first, and how often to meet.
Can Medications Be Used with Drug Abuse Counseling?
Yes, combining medication and drug abuse counseling is often the most effective approach. For opioid use disorder, medications such as buprenorphine or methadone reduce withdrawal and cravings; naltrexone is another option. For alcohol use disorder, acamprosate or naltrexone can help.
Counseling then builds coping skills, strengthens motivation, and addresses mood, trauma, and daily routines. The prescriber and counselor coordinate care, monitor side effects & benefits, and update the plan as recovery moves forward.
Is Drug Abuse Counseling Confidential and Safe?
Confidentiality is a core standard. Programs follow HIPAA and the federal confidentiality rule 42 CFR Part 2, which tightly limits disclosure of identifiable substance use information.
Consent is needed before talking with family or other providers, except in emergencies.
Safety is addressed head‑on: overdose education and naloxone, suicide risk checks, domestic violence screening, and a written safety plan. Family can be involved, with permission, so support is aligned, not working at cross‑purposes.
Author
-
Our editorial team includes licensed clinicians and board-certified addiction specialists. Every article is written and reviewed to be clear, accurate, and rooted in real treatment experience.
View all posts -
Dr. Williams has held senior leadership positions in the behavioral health field for over 30 years. He has worked with diverse populations in various private and public sectors.
View all posts